Background and aim. Bacterial peritonitis (SBP) is the most frequent infection in patients with cirrhosis causing significant mortality. Delay in SBP diagnosis is a serious problem. The aim of this study was to evaluate the diagnostic yield of Uri-Quick Clini-10SGR vs. Multistix 10SGR reagent strips in an Emergency Department.
Material and methods. A prospective study of consecutive patients with ascites and paracentesis attending to Emergency Department from March 2005 to February 2007 was made. SBP was defined by 250 neutrophiles /mm3. The ascites obtained at bedside was immediately tested in a dry test tube with both the Uri-Quick Clini 10SGR and MultistixSG10R. The Uri-Quick Clini 10SGR and Multistix SG10R. Strips were considered positive at grade. 3 (.125 leukocytes/mL).
Results. A total of 223 ascitic fluid samples were obtained. There were 49 episodes of SBP. Median age was 54 (range 18-87 year) years; 62.3% were female. The sensitivity, specificity, PPV, NPV, and 95% CI for Uri-Quick Clini 10SGR were 79.6 (64-87), 98.2 (94-99), 90.5 (78-96) and 93.9 (89-96), respectively. For MultistixSG10R the values were 77.5 (64-88), 97.7 (93-98), 90 (77.9-96.2), and 94 (89.4-96.6), respectively.
Conclusion. The use of reagent strip is useful for SBP diagnosis in an emergency setting. The high PPV allow start antibiotic treatment. In areas without the resources to perform conventional ascites fluid analyses, these strips could be presentlyused.
Infections in cirrhotic patients are the major cause of hospitalization and death, being responsible until 30 and 50% of cases, respectively.1 Spontaneous bacterial peritonitis (SBP) is the most frequent infection in these patients.2 The gold standard for the diagnosis of SBP is the neutrophile count in ascites fluid, defined by polymorphonuclear (PMN) count of > 250 cell/mm3.3 Unfortunately the manual cellular count with special smears, actual method for SBP diagnosis is a laborious and time-dependent procedure, and expertise is required.4 If this resource is not available, a delay in diagnosis and treatment exposes patients to a high risk of death, whereas the systematic use of empirical large spectrum antibiotics leads to unjustified iatrogenic or nosocomial complications, and increased medical cost.
The leukocyte esterase reagent strips are special devices that allow leukocyte detection in different biological fluids via a colorimetric reaction.5,6 There are previous reports that describe the use of test strips to make an "instant" diagnosis of SBP.7,8 However, the reagent strips used in these previous reports are scarce and difficult to obtain in our environment. Therefore, we assessed their diagnostic accuracy of two different reagent strip in an emergency setting with a big sample, using multiple observers.
Material and MethodsPatientsAll consecutive patients attending Emergency Department with ascites and paracentesis from March 2005 to February 2007 were included. Asymptomatic patients and patients with SBP suspicion were included. SBP was defined by PMN count of > 250 cell/ mm3. Paracentesis were performed on admission as dictated by standard medical practice, and repeated as indicated. These included diagnostic paracentesis alone, or combined therapeutic and diagnostic. The ascites obtained at bedside was immediately tested in a dry test tube with both the Uri-Quick Clini 10SG® (Stanbio Laboratory, Texas, USA) and MultistixSG10® (Bayer diagnostics, Bridgend, UK) strips, according to the manufacturer's guidelines for urine testing: strips were immersed in the ascitic fluid, immediately removed and after the required waiting period the color of the reagent square corresponding to leukocytes was compared with the color chart on the bottle. The Uri-Quick Clini 10SG® is read at 120 s and is either negative or four-tier positive (+1 to +3). The MultistixSG10s is read at 120 s and is either negative or four-tier positive (trace, +1 to +3). The strips were considered positive at grade 3 (125 leukocytes/mL), because grade 4 is above the cutoff defining SBP. Two physicians participated in reading the strips, one of them in patient's charge. In all cases both physician were unaware of the results of ascites manual cellular count. All ascites fluid samples were then processed in the hospital laboratory for manual cell count with differential, ascitic fluid culture and biochemistry. Cultures were performed using 10 mL of fluid in aerobic and anaerobic media blood culture bottles. Antibiotic therapy was initiated if the ascites fluid PMN cell count was > 250/mL.
Statistical analysisResults of leukocyte esterase reagent strip testing were compared with leukocyte (total count) and PMN counts, ascitic fluid culture and biochemical analysis and clinical data in all patients. Sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios of each reagent strip in the diagnosis of SBP were calculated. 95% confidence intervals for proportions were calculated. Likelihood ratios were weighted by prevalence. Concordance between investigator and physician on patient's charge readings and between reagent strips was also evaluated using the kappa statistic (к). All analyses were conducted using the statistics program SPSS/PC version12.0 (Chicago, IL, USA).
ResultsTwo-hundred and twenty-nine ascites fluid samples were obtained of 138 patients during 48 months. Six samples were excluded because does not have manual cellular count. There were 49 episodes of SBP. The median number of samples/patient was 1 (range 1-7). Median age was 54 (range 18-87) years; 62.3% were female; and 4 (2.9%) were Child A, 51 (37%) were Child B and 83 (60.1%) were Child C. Cirrhosis was caused by chronic hepatitis C in 29.7% of cases, autoimmune hepatitis on 13%, cryptogenetic cirrhosis on 11.6%, alcohol in 7%, 19.6% of patients were cirrhosis under diagnosis process and others causes in 19%. At the time of fluid collection 59 cases (26.5%) were associated with a presumptive diagnosis of SBP.
Total cell count ranged from 0 to 11,800/mm3. Forty-nine samples (21.9%) had an ascites PMN count > 250/mL (range: 255-10,620), obtained in 40 patients with total counts ranging from 267 to 11,800. Of these 49 cases, 14 (28.5%) were associated with positive ascites cultures. Of the 49 patients with SBP, 39 (79.6%) had had the presumptive diagnosis of SBP. Four patients diagnosed with SBP were under prophylaxis at the time of diagnosis.
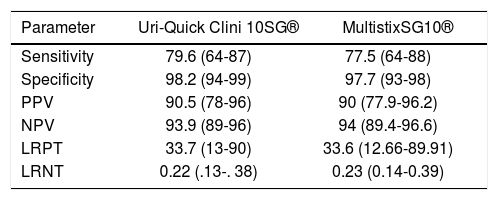
In all 223 samples, when results were expressed as either positive or negative, the readings of the two physicians concurred 100%. Table 1 shows the sensitivity, specificity, PPV, NPV, likelihood ratio for a positive test, likelihood ratio for a negative test, and 95% CI when we considered a reagent strip positive with grade 3. When results were characterized, as either positive or negative, kappa value was 0.94; p < 0.001.
Sensitivity, specificity, PPV, NPV, LRPT, LRNT, and 95% CI when we considered a reagent strip positive with grade 3.
| Parameter | Uri-Quick Clini 10SG® | MultistixSG10® |
|---|---|---|
| Sensitivity | 79.6 (64-87) | 77.5 (64-88) |
| Specificity | 98.2 (94-99) | 97.7 (93-98) |
| PPV | 90.5 (78-96) | 90 (77.9-96.2) |
| NPV | 93.9 (89-96) | 94 (89.4-96.6) |
| LRPT | 33.7 (13-90) | 33.6 (12.66-89.91) |
| LRNT | 0.22 (.13-. 38) | 0.23 (0.14-0.39) |
PPV: positive predictive value. NPV: negative predictive value. LRPT: likelihood ratio for a positive test. LRNT: likelihood ratio for a negative test.
For patients without a priori clinical or biological signs of infection (164 patients; 73.5%), sensitivity was 77.2%, specificity was 98.5%, PPV 89.4%, and NPV 96.5% for Uri-Quick Clini 10SG®. For MultistixSG10® strips sensitivity was 77.2%, specificity was 97.8%, PPV 85%, and NPV 96.5%.
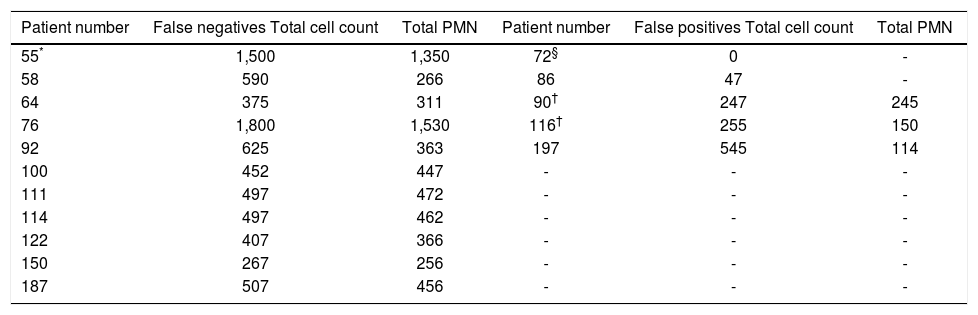
In table 2 are shown discordant results (negative and positive false) obtained from ascitic samples with leukocyte esterase reagent strip according manual cellular count result as gold standard.
Discordant results obtained from ascitic samples with leukocyte esterase reagent strip according manual cellular count result as gold standard.
| Patient number | False negatives Total cell count | Total PMN | Patient number | False positives Total cell count | Total PMN |
|---|---|---|---|---|---|
| 55* | 1,500 | 1,350 | 72§ | 0 | - |
| 58 | 590 | 266 | 86 | 47 | - |
| 64 | 375 | 311 | 90† | 247 | 245 |
| 76 | 1,800 | 1,530 | 116† | 255 | 150 |
| 92 | 625 | 363 | 197 | 545 | 114 |
| 100 | 452 | 447 | - | - | - |
| 111 | 497 | 472 | - | - | - |
| 114 | 497 | 462 | - | - | - |
| 122 | 407 | 366 | - | - | - |
| 150 | 267 | 256 | - | - | - |
| 187 | 507 | 456 | - | - | - |
This study represents the first report from a Latin American center of diagnostic yield of a reagent strip easily available in our environment and the only one in worldwide, for our knowledge, with patients exclusively arising from an emergency department. According with our results the Uri-Quick Clini 10SG® and MultistixSG10® strips are both useful for a rapid SBP diagnosis in an emergency setting. These data are according with previous reports.7,8
The rapidity in diagnosis is an important issue in SBP because it could, as similar as with other septic patients, it represents an early treatment application with a potential positive effect morbi-mortality.1 Delay in diagnosis because the scarcity of trained personal, and therefore treatment of patients with SBP is an important problem previously reported.4 According with our results, use of reagent strips available in our environment could be use to decide about to initiate treatment or continue the diagnostic approach of cirrhotic patients attending Emergency Department. The positive predictive value of reagent strips allow start treatment without considerable risk to unjustified iatrogenic, nosocomial complications, or increased medical cost. The negative predictive value, however, for be a high mortality-disease is not enough for discard SBP. In terms of the severity of SBP, the rate of false-negative results could be considered high.
The test with Uri-Quick Clini 10SG® may help the clinician in some circumstances when a cell count is not available within a few hours. These reagent strips may be useful in developing countries without sufficient resources. The cost of the strip is only 0.50USD.
We chose to use in this study the Uri-Quick Clini 10SG® for several reasons: there is no previous study with this strip and this test is widely available in public institutions in Mexico. Nonetheless, other reagent strips can be used with greater accuracy. Castellote, et al.9 used Aution sticks® manufactured in Italy and observed 89% sensitivity. However, these strips are not available in our country. To our knowledge, no study had yet compared Aution sticks® and Uri-Quick Clini 10SG® strips. Sapey, et al.,10 compared the Multistix 10 SG® and the Nephur test® and showed that the Nephur test® was more sensitive (88.2 vs. 64.7%). The Combur test®, which is a modified version of the Nephur test®, has also been recently compared with the Multistix® in 2 studies.8,11 The sensitivity of the tests was identical in the study by Thevenot, et al.,8 whereas the Combur® test was more sensitive than the Multistix® test in the first when using the threshold of grade 2 on a colorimetric scale (63.0 vs. 45.7%).11
These results support the need to evaluate the strips easy-available in our environment. In a previous review article that summarize published related articles the authors concludes that the use of reagent strips for the diagnosis of SBP cannot be recommended because low sensitivity, especially in patient with low PMN count, however is important to consider that any of the included studies in that review was carried-out using Uri-Quick Clini 10SG® strips.12 More recent papers (one systematic review, and editorial and one with original data) conclude that there is reasonable amount of evidence to support the use of reagent strips in the work-up of patients suspected of having SBP mainly in poorer were ascitic fluid testing may not be readily available.13-15
One limitation of our study is the subjectivity of the reading strip, common to all colorimetric tests.
In summary, the use of reagent strip is useful for SBP diagnosis in an emergency setting. The high PPV allow start treatment without concern about possible collateral effects, however because the severity of disease and the NPV of the test we do not recommend ruleout SBP diagnosis in a patient with negative reagent strip test but a clinical presentation suggestive of SBP. We do not suggest that standard ascites fluid analyses be systematically replaced by the use of leukocyte esterase reagent strips. Nonetheless, in areas without the resources to perform ascites fluid analyses, these strips could be presently used.