Introduction. Spontaneous bacterial peritonitis (SBP) is associated with a high in-hospital mortality rate ranging from 20-40%. The model for end-stage liver disease (MELD) has been suggested as a predictor of inhospital mortality in patients with SBP. However, the accuracy of the MELD has been questioned, and the integrated MELD (iMELD) score, which incorporates age and serum sodium to the previous model, has been proposed to improve prognostic accuracy. The iMELD has not yet been evaluated in patients with SBP.
Aim. To evaluate the accuracy of iMELD and MELD scores in predicting in-hospital mortality in patients with SBP and to identify other prognostic factors of mortality in this group of patients.
Results. Of 40 patients analyzed, 65% were male, 50% had hepatitis C, and 27.5% had hepatocellular carcinoma. Mean age was 55.6 years; 25.7% were classified as Child-Pugh class B, and 74.3% as class C. Mean scores were 46.0 and 19.9 for iMELD and MELD, respectively. In-hospital mortality was 40%. Univariate analysis showed that total bilirubin, creatinine, MELD and iMELD scores were significantly associated with in-hospital mortality. The prognostic accuracy was 80% and 77% for iMELD and MELD scores, respectively.
Conclusion. In conclusion, bilirubin, creatinine, MELD and iMELD were predictors of in-hospital mortality in cirrhotic patients with SPB. iMELD was slightly more accurate than MELD in this group of patients.
Spontaneous bacterial peritonitis (SBP) accounts for 24% of infections affecting cirrhotic patients with ascites,1 with an inpatient prevalence of approximately 10% in this population.2,3 Despite the use of protective measures such as early diagnosis and albumin therapy, as well as the introduction of new antibiotics, the prognosis of SBP remains poor, with an in-hospital mortality rate of 20-40%.4
In this context, the identification of patients at high risk of death is extremely important to support evidence-based decision-making and improve prognosis. Age, bilirubin and creatinine rates, among others, are predictors of in-hospital mortality in patients with SBP.5-7 More recently, the model for endstage liver disease (MELD) score has also been suggested as an independent risk factor for mortality in patients with SBP;4,8,9 however, the predictive accuracy of MELD score has been questioned. An integrated MELD (iMELD) incorporating age and serum sodium has been proposed to improve the prognostic accuracy of MELD,10 but has not yet been specifically evaluated as a predictor of mortality in patients with SBP.
ObjectiveThe objectives of this study were:
- •
To identify prognostic factors for in-hospital mortality in patients with SBP, and
To evaluate and compare the predictive power of MELD and iMELD scores for in-hospital mortality in patients with SBP.
Adults with cirrhosis and SBP were consecutively enrolled between January 2007 and May 2010 at the Gastroenterology and Hepatology Service at Complexo Hospitalar Santa Casa de Porto Alegre, Brazil. The study was approved by the local Ethics Committee (Institutional Review Board-equivalent) and was conducted in accordance with the provisions of the Declaration of Helsinki.
The diagnosis of cirrhosis was based on clinical, laboratory and imaging findings. All patients underwent diagnostic paracentesis within 24 h of admission or whenever peritonitis was suspected. SBP was diagnosed in the presence of a polymorphonuclear (PMN) cell count ≥ 250 cells/mm3 in peritoneal fluid and absence of any other source of intra-abdominal infection, with no need to identify the infecting organisms.11 SBP was considered as hospital-acquired when diagnosed after 48 h of admission or within 48 h of admission in patients meeting any of the following criteria:
- •
Having been in hospital care, hemodialysis or intravenous chemotherapy 30 days before the onset of infection; or
- •
Hospitalization for at least two days or surgery 180 days before the onset of infection; or
- •
Institutionalized patients.
SBP was considered as community-acquired when diagnosed at admission or within 48 h of admission in the absence of the criteria mentioned above.12
Patients were treated with intravenous cefotaxime or amoxicillin-sulbactam. Piperacillin-tazobactam or carbapenems were used in patients with hospital-acquired SBP or receiving norfloxacin prophylaxis. Intravenous human albumin was used at the discretion of the attending physician.
Variables of interestInformation was collected on sex, age, etiology of cirrhosis, severity of ascites (graded clinically or by ultrasound as mild, moderate or gross), degree of hepatic encephalopathy according to West Haven criteria,13 and concomitant hepatocellular carcinoma. Laboratory variables included serum creatinine, total bilirubin, international normalized ratio (INR), albumin, serum sodium, and ascitic fluid PMN cell count.
MELD score was calculated according to the United Network for Organ Sharing (UNOS) formula:14
MELD = 3.78 loge total bilirubin (mg/dL) + 11.2 loge INR + 9.57 loge serum creatinine (mg/dL) + 6.43
Bilirubin, INR or creatinine values < 1.0 were rounded to 1.0 to avoid negative scores, and creatinine values were capped at 4.0. MELD scores were not capped at 40, and additional points were not added for patients with hepatocellular carcinoma. For the iMELD score, MELD, age (years) and serum Na (mEq/L) were considered:11
MELD + [age x 0.3] - [0.7 x Na] + 100.
The Child-Turcotte-Pugh (CTP) score was determined on the basis of the presence of ascites, hepatic encephalopathy, levels of total serum bilirubin and albumin, and prothrombin time.15
Statistical analysisContinuous variables were expressed as mean ± standard deviation (SD) and categorical variables as count and percentage. Comparisons between groups were performed using Student's t test or Mann-Whitney test for continuous variables and the chi-square test for categorical variables. Values were considered to be statistically significant if p-value was < 0.05. Univariate analysis was performed by using simple logistic regression. A receiver operating characteristic (ROC) curve was generated for MELD and iMELD scores to assess the predictive accuracy of these models to determine death risk. An area under the curve (AUC) between 0.80 and 0.90 indicated good discriminatory ability. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 17.0.
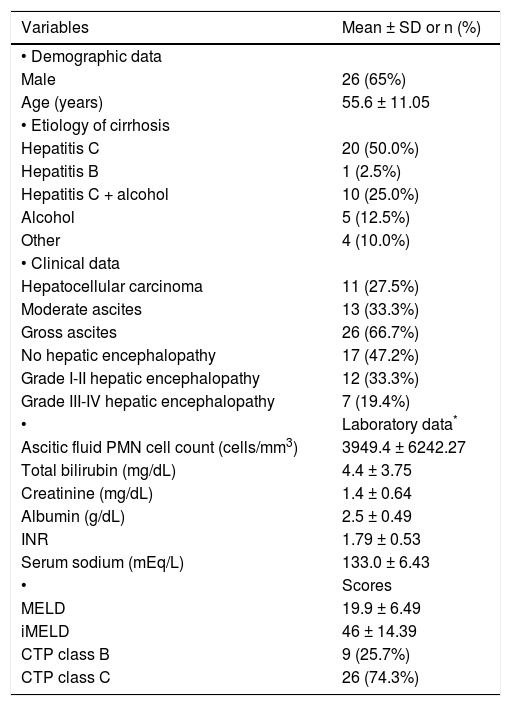
ResultsForty patients were included in the analysis. The demographic, clinical, and laboratory characteristics of patients are described in table 1. Mean MELD and iMELD scores were 19.9 and 46.0, respectively, and most patients were classified as CTP class C (Table 1). Five patients with incomplete data were not classified according to CTP.
Characteristics of patients with spontaneous bacterial peritonitis (n = 40).
| Variables | Mean ± SD or n (%) |
|---|---|
| • Demographic data | |
| Male | 26 (65%) |
| Age (years) | 55.6 ± 11.05 |
| • Etiology of cirrhosis | |
| Hepatitis C | 20 (50.0%) |
| Hepatitis B | 1 (2.5%) |
| Hepatitis C + alcohol | 10 (25.0%) |
| Alcohol | 5 (12.5%) |
| Other | 4 (10.0%) |
| • Clinical data | |
| Hepatocellular carcinoma | 11 (27.5%) |
| Moderate ascites | 13 (33.3%) |
| Gross ascites | 26 (66.7%) |
| No hepatic encephalopathy | 17 (47.2%) |
| Grade I-II hepatic encephalopathy | 12 (33.3%) |
| Grade III-IV hepatic encephalopathy | 7 (19.4%) |
| • | Laboratory data* |
| Ascitic fluid PMN cell count (cells/mm3) | 3949.4 ± 6242.27 |
| Total bilirubin (mg/dL) | 4.4 ± 3.75 |
| Creatinine (mg/dL) | 1.4 ± 0.64 |
| Albumin (g/dL) | 2.5 ± 0.49 |
| INR | 1.79 ± 0.53 |
| Serum sodium (mEq/L) | 133.0 ± 6.43 |
| • | Scores |
| MELD | 19.9 ± 6.49 |
| iMELD | 46 ± 14.39 |
| CTP class B | 9 (25.7%) |
| CTP class C | 26 (74.3%) |
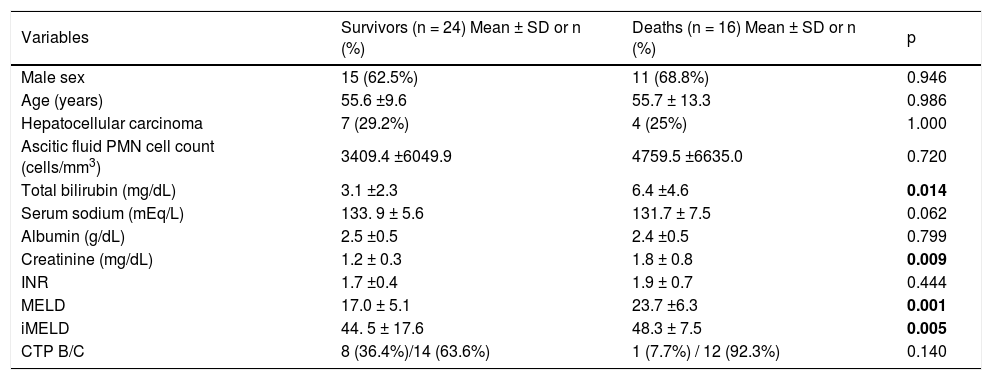
In-hospital mortality rate was 40% (n = 16). Univariate analysis showed that bilirubin, creatinine, MELD and iMELD scores were significantly associated with in-hospital mortality (Table 2).
Univariate analysis of parameters analyzed in patients with SBP.
| Variables | Survivors (n = 24) Mean ± SD or n (%) | Deaths (n = 16) Mean ± SD or n (%) | p |
|---|---|---|---|
| Male sex | 15 (62.5%) | 11 (68.8%) | 0.946 |
| Age (years) | 55.6 ±9.6 | 55.7 ± 13.3 | 0.986 |
| Hepatocellular carcinoma | 7 (29.2%) | 4 (25%) | 1.000 |
| Ascitic fluid PMN cell count (cells/mm3) | 3409.4 ±6049.9 | 4759.5 ±6635.0 | 0.720 |
| Total bilirubin (mg/dL) | 3.1 ±2.3 | 6.4 ±4.6 | 0.014 |
| Serum sodium (mEq/L) | 133. 9 ± 5.6 | 131.7 ± 7.5 | 0.062 |
| Albumin (g/dL) | 2.5 ±0.5 | 2.4 ±0.5 | 0.799 |
| Creatinine (mg/dL) | 1.2 ± 0.3 | 1.8 ± 0.8 | 0.009 |
| INR | 1.7 ±0.4 | 1.9 ± 0.7 | 0.444 |
| MELD | 17.0 ± 5.1 | 23.7 ±6.3 | 0.001 |
| iMELD | 44. 5 ± 17.6 | 48.3 ± 7.5 | 0.005 |
| CTP B/C | 8 (36.4%)/14 (63.6%) | 1 (7.7%) / 12 (92.3%) | 0.140 |
CTP: Child-Turcotte-Pugh. iMELD: integrated MELD. INR: international normalized ratio. MELD: model for end-stage liver disease. PMN: polymorphonu-clear. SBP: spontaneous bacterial peritonitis. SD: standard deviation.
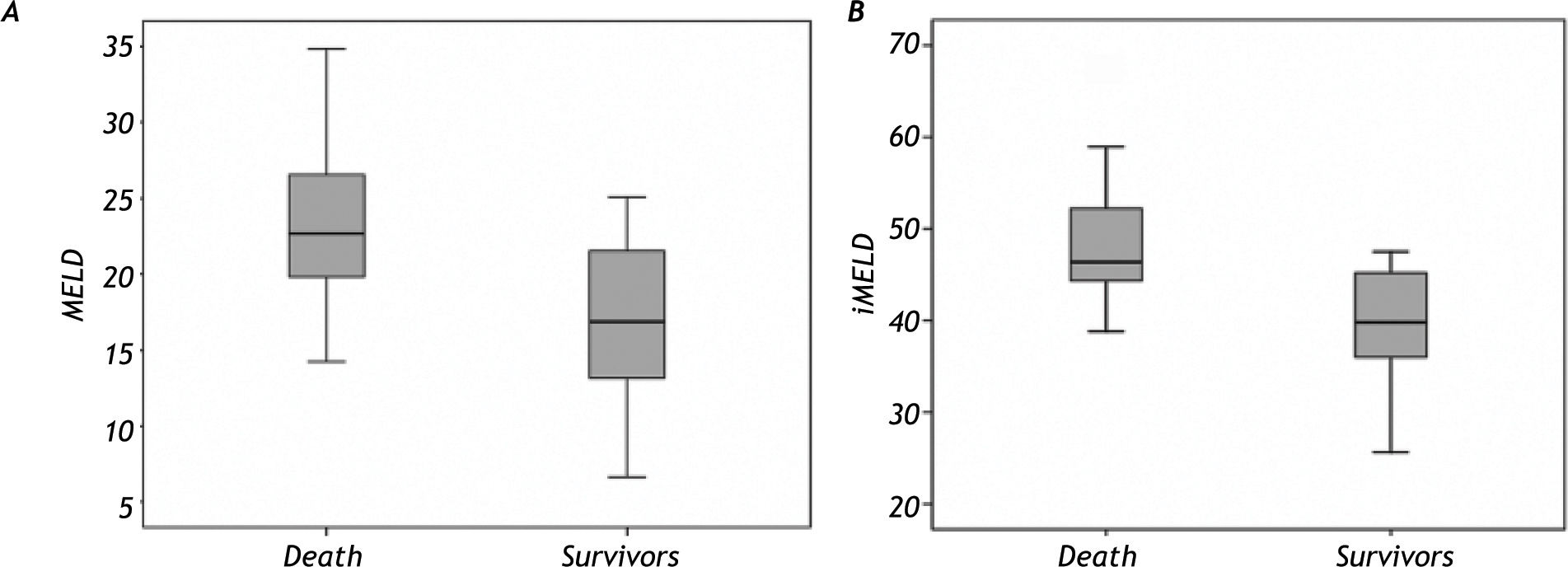
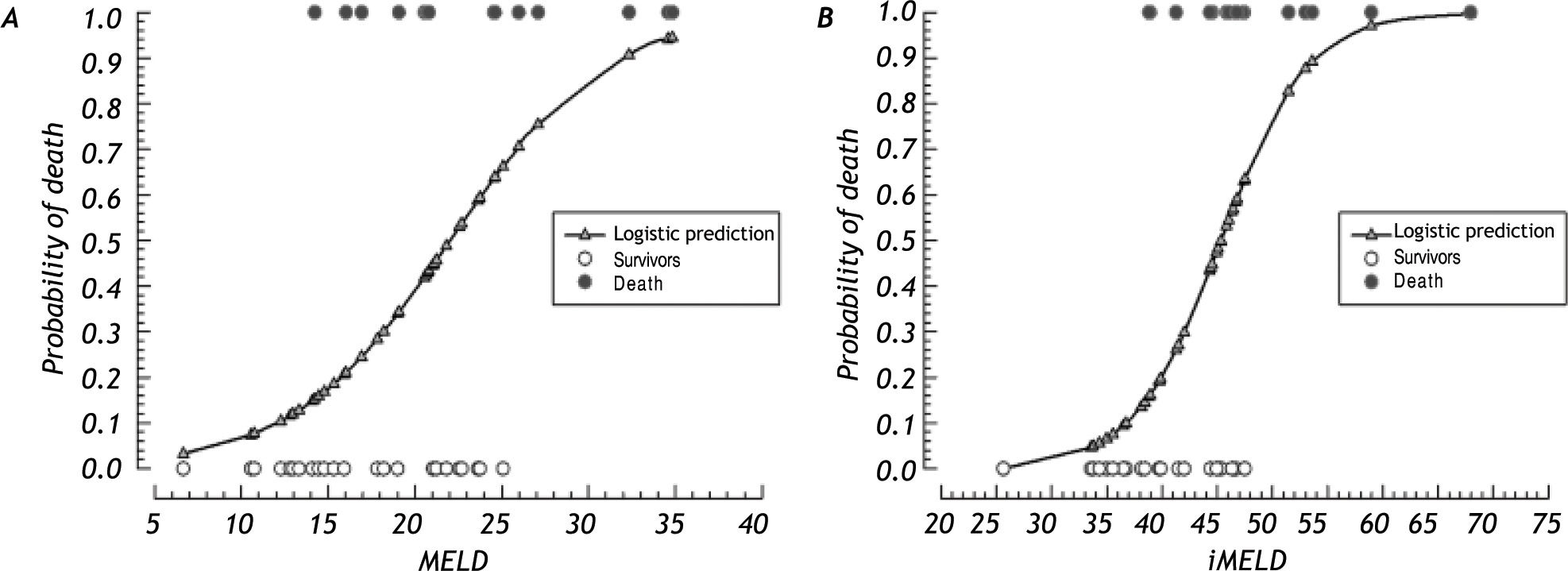
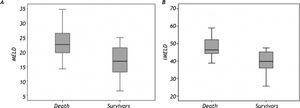
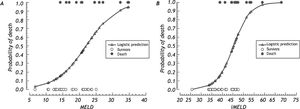
The mean MELD and iMELD scores of patients who died were significantly higher than those of survivors (p = 0.001 and p = 0.005, respectively); the accuracy of iMELD to predict mortality was slightly better than that of MELD (Figure 1). Figure 2 shows the comparison between the estimated mortality for MELD or iMELD scores and the actual proportion of deaths. There seems to be a benefit associated with the use of iMELD, because this model shows a narrower range of inconclusive results, i.e., scores that do not allow the prediction of the actual outcome (death or survival).
The AUCs for MELD and iMELD scores were as high as 0.77 (95% CI 0.62-0.91) and 0.80 (95% CI 0.66-0.93), respectively, indicating that in up to 77% and 80% of the pairs (death-survival) the models correctly estimated that the probability of death was higher than that of survival.
DiscussionIn this study, bilirubin, serum creatinine, MELD and iMELD scores were identified as predictors of in-hospital mortality in patients with SBP. This is the first study to evaluate the prognostic value of iMELD in cirrhotic patients with SBP.
Our study corroborates the value of bilirubin and creatinine as predictors of death in patients with SPB as indicated by previous studies.7,16 For example, Terg, et al.,7 report that mortality was higher in patients with bilirubin levels > 4 mg/dL or serum creatinine > 1 mg/dL, considered to be at high risk, as compared to low risk patients (23.0% x 6.5%, p = 0.01).
In our series, creatinine was significantly higher in patients who died during hospitalization than in survivors (1.8 mg/dL vs. 1.2 mg/dL). A review of English-language articles16 has shown that renal dysfunction, usually defined as creatinine > 1.5 mg/dL, was the most robust predictor of death among prognostic parameters for in-hospital mortality in patients with SBP. That finding warrants the identification of patients at high risk of death and the intravenous administration of albumin to reduce renal impairment and improve survival, as previously described.17 Another study analyzing four data sets18 has questioned the value of creatinine level as a predictor of death. However, since most patients in that study did not receive intravenous albumin, it is possible that its conclusions could not be generalized.
We identified MELD score as a predictor of death, in agreement with other studies.4,8,10 Previous studies18 have suggested that the ability of MELD score to predict prognosis should be validated in patients at high risk of death receiving albumin systematically. If MELD score remains as an independent predictor in such a population, a cutoff point could be identified, indicating the need for more intensive measures in order to reduce the high mortality rates still observed in patients with SBP.18
MELD score is a predictor of three-month survival in cirrhotic patients,19,20 including those awaiting liver transplantation.21,22 However, some limitations of the model23 have prompted the creation of other scores derived from MELD, including the iMELD. The iMELD incorporates two additional variables: age and serum sodium.10 Therefore, in the iMELD, age –a well-known predictor of death in cirrhotic patients–24 was recognized as a prognostic factor independent of MELD. In addition, iMELD confirmed that hyponatremia (defined as Na < 130 mEq/L) is an independent risk factor for death in cirrhotic patients, as shown in previous studies.25,26 As shown in figure 1, iMELD was slightly more accurate than MELD in predicting mortality.
The present study has limitations that should be addressed: the inclusion of a small number of patients may have affected the analysis of some variables, such as age, which is a predictor of death in patients with SBP.4 Also, in our hospital, a considerable number of patients are admitted to the Hepatology Service via the emergency room. Thus, the diagnosis of SBP is often established and treatment started in an emergency setting, and cefotaxime and albumin are not always prescribed, as recommended.26 Nevertheless, the mortality observed in our study was similar to that reported in the literature.4
ConclusionIn conclusion, bilirubin, creatinine, MELD score and iMELD score were confirmed as prognostic factors for mortality in patients with SBP. iMELD was shown to be more accurate than MELD in this context. Prospective studies including patients regularly treated with albumin following clinical practice guidelines are needed to establish the actual value of MELD and iMELD in predicting mortality in patients with SBP and to establish cutoff points to identify high-risk patients.
Abbreviations- •
AUC: area under the curve.
- •
CTP: Child-Turcotte-Pugh.
- •
iMELD: integrated MELD model.
- •
INR: international normalized ratio.
- •
MELD: model for end-stage liver disease.
- •
PMN: polymorphonuclear.
- •
ROC curve: receiver operating characteristic curve.
- •
SBP: spontaneous bacterial peritonitis.
- •
SPSS: statistical Package for the Social Sciences.
- •
UNOS: United Network for Organ Sharing.
The study did not receive financial support or grants.