The MELD score has been established as an efficient and rigorous prioritization system for liver transplant (LT). Our study aimed to evaluate the effectiveness of the MELD score as a system for prioritization for LT, in terms of decreasing the dropout rate in the waiting list and maintaining an adequate survival post-LT in Chile.
Materials and methodsWe analyzed the Chilean Public Health Institute liver transplant registry of candidates listed from October 15th 2011 to December 31st 2014. We included adult candidates (>15 years old) listed for elective cadaveric LT with a MELD score of 15 or higher. Statistical analysis included survival curves (Kaplan–Meier), log-rank statistics and multivariate logistic regression.
Results420 candidates were analyzed. Mean age was 53.6±11.8 years, and 244 were men (58%). Causes of LT included: Liver cirrhosis without exceptions (HC) 177 (66.4%); hepatocellular carcinoma (HCC) 111 (26.4%); cirrhosis with non-HCC exceptions 102 (24.3%) and non-cirrhotic candidates 30 (7.2%). LT rate was 43.2%. The dropout rate was 37.6% at 1-year. Even though the LT rate was higher, the annual dropout rate was significantly higher in cirrhotic candidates (without exceptions) compared with cirrhotics with HCC, and non-HCC exceptions plus non-cirrhotic candidates (47.9%; 37.2% and 24.2%, respectively, with p=0.004). Post-LT survival was 84% per year, with no significant differences between the three groups (p=0.95).
ConclusionPrioritization for LT using the MELD score system has not decreased the dropout rate in Chile (persistent low donor's rate). Exceptions generate inequities in dropout rate, disadvantaging patients without exceptions.
Cirrhosis is a prevalent disease with high morbidity and mortality. It constitutes an important cause of death worldwide, reaching 1.03 million deaths per year [1]. In Chile, cirrhosis is the 5th cause of death [2,3]. As the disease progresses, complications occur that can be dependent or not from portal hypertension, including ascites, variceal bleeding, hepatic encephalopathy, spontaneous bacterial peritonitis, among others.
Decompensated cirrhosis is associated with poor prognosis and impaired quality of life. Therapies are generally targeted to delay disease progression and prevent complications. In this scenario, liver transplantation (LT) is the only available curative therapy [4]. The long-term survival post-LT has increased substantially thanks to the better intensive care and immunosuppressive treatments. The 1-year survival post-LT reaches 90% in developed countries.
The allocation for LT in our country has been an important topic since the liver donor's rate is extremely low (10 donors per million population) compared to other countries with high LT rate (35 donors per million population in Spain) [5]. Our previous system of prioritization for LT considered a MELD score of 15 or higher to be enlisted, and posterior allocation was performed by time in the waiting list. Some candidates with exceptions could be enlisted for LT, receiving an organ by waiting as well. However, this system had flaws that included early LT in candidates with low mortality risk, and a high dropout rate within the waiting list of candidates with advanced liver disease secondary to death or disease progression. To avoid these problems, a new allocation system that accurately predicted long-term survival on the waiting list while maintaining a high post-LT survival was necessary.
There are several models to predict survival in advanced cirrhosis. One of the most important is the Child–Turcotte–Pugh score, originally devised in the assessment of severity in cirrhotic patients undergoing surgery for portal hypertension [6]. Although this model could be helpful for prioritizing liver transplant recipients and was used for prioritization in several countries, it considers subjective aspects like ascites and encephalopathy [7]. Also, it does not include renal function, a well-established prognostic factor in advanced cirrhosis [8].
The Model for End-Stage Liver Disease (MELD) score system was published originally to predict 30-day mortality in cirrhotic patients going to TIPS treatment (Transjugular Intrahepatic Portosystemic Shunt) [9]. Later, it was adapted to predict short-term survival in cirrhotic candidates and proposed for prioritization of recipients for LT in the United States in 2002. Nowadays, the MELD score has been established as an efficient and rigorous allocation system for LT worldwide. However, MELD score does not consider complications such as digestive hemorrhage due to portal hypertension, hepatic encephalopathy, ascites or bacterial peritonitis. On the other hand, creatinine can fluctuate overestimating patients with parenchymal kidney disease. In addition, results have not been satisfactory in terms of justice and dropout from the waiting list for some countries [10]. In Chile, MELD was adopted as an allocation system in October 2011. However, no data regarding its efficiency in terms of survival and dropout from the waiting list during this period have been published.
The aim of our study was to evaluate the effectiveness of the MELD score as a system for prioritization for LT. Additionally, we compared dropout in waiting list between cirrhotic candidates prioritized per real MELD score and candidates enrolled for transplants by exceptions who are assigned an arbitrary operational score agreed in a consensus group. Finally, we evaluated the properties of the MELD score in predicting the dropout rate within the waiting list and mortality post-LT.
1Methods1.1Candidates and inclusion criteriaWe examined the Chilean Public Health Institute (PHI) registry of candidates listed for a liver transplant from October of 2011 until December of 2014. We included adult candidates (>15 years old) listed for elective cadaveric liver transplant with a MELD score of 15 or higher. Exclusion criteria included: pediatric candidates (≤15 years old), candidates delisted for active substance abuse, surgical contraindication before the start date of the study, and candidates who lost their outpatient controls. This study did not include candidates listed for acute liver failure.
Information used was authorized by the National Transplant Coordinator, the governmental institution responsible for transplant allocation in Chile. All data were de-identified, and additional information was requested in exceptional cases, to the seven centers of liver transplantation in Chile using an anonymous code allocated by the PHI.
1.2National Liver Transplantation System: MELD scoring and exceptionsThe MELD score was calculated based on the previously published model [11]. We used the MELD score for the analysis since the MELD-Na (MELD-Sodium score) was incorporated as a criterion for enlistment in October 2016 (posterior to the follow-up period). We considered an operational MELD score for the analysis: (1) The real MELD score in candidates with liver cirrhosis without exceptions. (2) The adjusted MELD score in candidates with exceptional situations where the real MELD score does not adequately reflect mortality or the quality of life. The exceptions are defined by the Liver Transplant Committee who assign, in a consensual way, an adjusted score to the conditions (expressed in the National Liver Transplant Standards):
- -
Malignant liver tumors: including candidates with hepatocellular carcinoma (HCC) per Milan Criteria for LT, without vascular or extrahepatic dissemination [12]. We did not include a downstaging strategy because it was incorporated into our system after the end of the follow-up of the study [13,14]. This condition receives an initial operational MELD score of 20 and posteriorly increases 1 point every two months.
- -
Chronic cholestatic diseases: including primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC) and overlap syndrome. We used the Mayo score (≥9.6 in PBC & overlap syndrome and ≥3.6 in PSC) for enlistment, with an initial operational MELD score of 15 [15,16]. We used the Mayo because the MELD score does not adequately predict mortality in this group [17]. Posteriorly, the operational MELD score increases according to a correlation between the Mayo and MELD score previously defined (for example a patient with PBC and a Mayo score of 10.3 obtain an operational MELD score of 20 since mortality is too similar in these cut-off points [28% at 12 months]).
- -
Complications from chronic cirrhosis: including refractory ascites (considered in candidates with more than one paracentesis per month for at least 6 months), recurrent spontaneous bacterial peritonitis (SBP) (receiving 1 extra point for each episode of SBP) and recurrent hepatic encephalopathy (requiring multiple hospitalizations, chronic invalidating or persistent after a solved acute liver failure). These conditions can receive an initial operational MELD score of 15 and posteriorly increases 2 points every three months. On the other side, candidates with intense itching refractory to medical treatment and severe impairment of quality of life can be enlisted (requires a photo-documentation showing excoriations of skin); they receive an initial operational MELD score of 15 and posteriorly increases 1 point every three months.
- -
Other conditions: hepatopulmonary syndrome, portopulmonary hypertension, type 1 hepatorenal syndrome, polycystic disease (associated with decreased renal clearance <30ml/min, severity impaired quality of life or malnutrition) and metabolic diseases.
The criteria for score assignment in exceptions are the same in all centers for liver transplantation in Chile. Also, every patient enlisted for a liver transplant is presented in a meeting including a representative from every center for liver transplant, where they discuss if every enlistment is appropriate or not.
1.3Statistical analysisContinuous data were described using mean and standard deviation (SD), median or interquartile ranges [IQ] (between percentiles 25 and 75%) per data distribution. Nominal data were described using percentages. We compared three groups: 1. Cirrhotic candidates without exceptions, 2. Candidates with HCC and 3. Cirrhotic candidates with exceptions (non-HCC). The main outcome was dropout defined by death, poor physical condition for the transplant or disease progression in HCC (outside Milan criteria). Kaplan–Meier estimates were used to calculate survival curves. Differences in survival curves were compared using a log-rank test. Differences in proportions were tested using the chi-square test (or the Fisher exact test). Additionally, we conducted a multivariate logistic regression to assess the association between MELD score and dropout from the waiting list and mortality post-LT. Odds ratio (OR) and 95% confidence interval (CI) were used to report these results. Statistical analysis was performed with IBM SPSS software version 22.0 (Armonk, NY: IBM Corp.) and STATA software version 13.0 (College Station, TX: StataCorp LP). A p value of <0.05 was considered statistically significant.
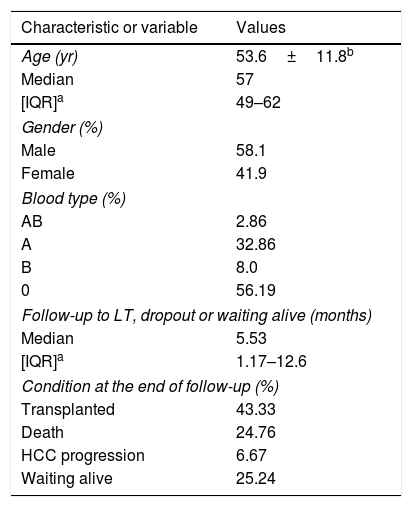
2Results2.1General characteristics and etiologiesFive hundred seventy-three candidates were listed for LT between October 15th 2011 and December 31st 2014. We included 420 elective candidates in the analysis (77.5%); 58.1% were males (n=244). The mean age was 53.6±11.8 years; with a range between 17 and 70 years old (Table 1). In this analysis, we excluded 153 candidates by several criteria previously expressed (pediatric candidates, acute liver failure, active substance abuse, surgical contraindication, candidates who lost their outpatient controls, among others).
Clinical, demographic, and other characteristics of the candidates.
| Characteristic or variable | Values |
|---|---|
| Age (yr) | 53.6±11.8b |
| Median | 57 |
| [IQR]a | 49–62 |
| Gender (%) | |
| Male | 58.1 |
| Female | 41.9 |
| Blood type (%) | |
| AB | 2.86 |
| A | 32.86 |
| B | 8.0 |
| 0 | 56.19 |
| Follow-up to LT, dropout or waiting alive (months) | |
| Median | 5.53 |
| [IQR]a | 1.17–12.6 |
| Condition at the end of follow-up (%) | |
| Transplanted | 43.33 |
| Death | 24.76 |
| HCC progression | 6.67 |
| Waiting alive | 25.24 |
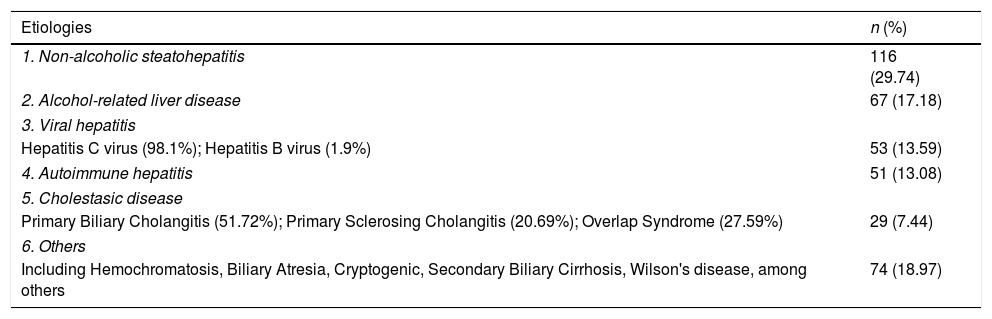
Candidates with liver cirrhosis without exceptions represented the most frequent cause of LT (n=177; 42.15%), followed by liver cirrhosis with HCC (n=111; 26.4%), cirrhosis with non-HCC exceptions (n=102; 24.3%) and non-cirrhotic causes (n=30; 7.15%). Table 2 shows the etiology of cirrhosis among cirrhotic candidates (n=390). The predominant etiology was non-alcoholic steatohepatitis (NASH), followed by alcohol-related liver disease, viral hepatitis, autoimmune hepatitis, cholestatic diseases, and others. The non-cirrhotic group (n=30) included hepatorenal polycystic disease, graft failure, hepatic epithelioid hemangioendothelioma, liver adenomatosis, recurrent cholangitis, among others.
Leading causes of enlistment for LT of cirrhotic candidates (n=390).
| Etiologies | n (%) |
|---|---|
| 1. Non-alcoholic steatohepatitis | 116 (29.74) |
| 2. Alcohol-related liver disease | 67 (17.18) |
| 3. Viral hepatitis | |
| Hepatitis C virus (98.1%); Hepatitis B virus (1.9%) | 53 (13.59) |
| 4. Autoimmune hepatitis | 51 (13.08) |
| 5. Cholestasic disease | |
| Primary Biliary Cholangitis (51.72%); Primary Sclerosing Cholangitis (20.69%); Overlap Syndrome (27.59%) | 29 (7.44) |
| 6. Others | |
| Including Hemochromatosis, Biliary Atresia, Cryptogenic, Secondary Biliary Cirrhosis, Wilson's disease, among others | 74 (18.97) |
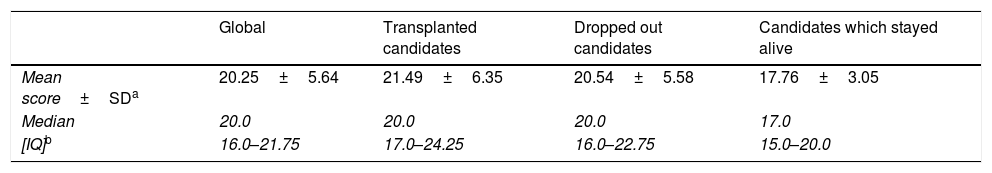
In a 38 months’ period, the follow-up rate was 100%. The median follow-up to an event was 5.53 months ([IQ] 1.17–12.6) (Table 1). Transplanted and dropped out candidates stayed on the waiting list a median of 4.25 months ([IQ] 0.7–11.55) and 5.1 months ([IQ] 2.0–9.7), respectively. Candidates still waiting for LT at the end of follow-up stayed a median of 10.4 months ([IQ] 4.2–22.15). Table 3 shows the mean MELD scores at enlistment for the whole population and by groups.
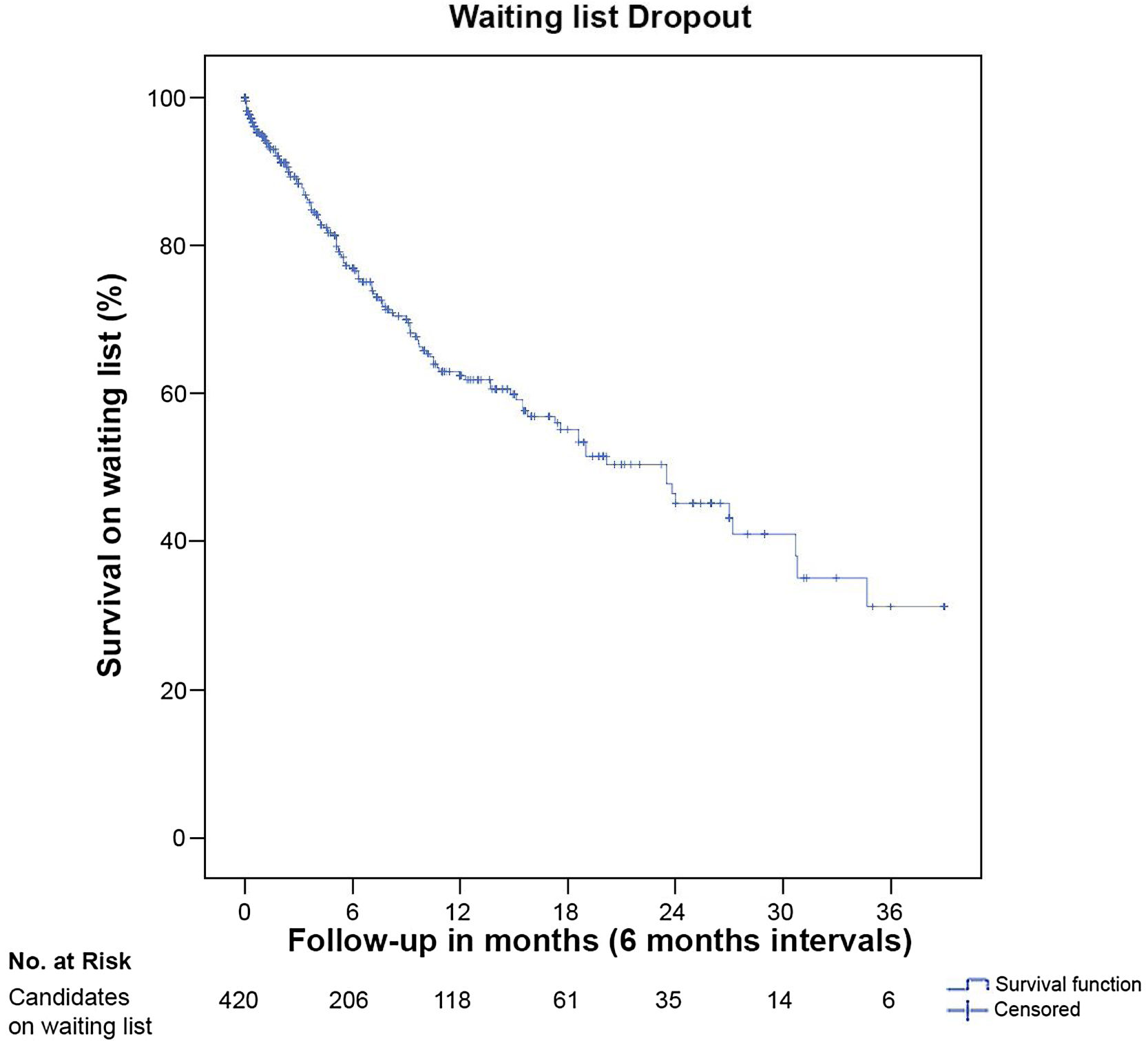
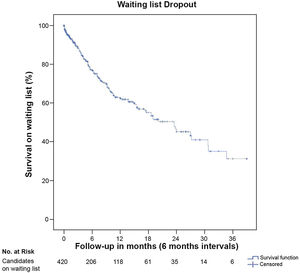
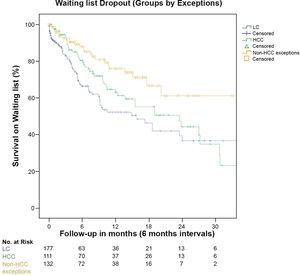
2.3Dropout rate within waiting listDropout occurred in 132 candidates (31.4%) (Table 1). Of these candidates, 21.2% occurred because of HCC progression and 78.8% death. Dropout risk at 12-months on the waiting list was 37.6% (Fig. 1). Secondly, at the end of follow-up, only 106 candidates remained on the waiting list (25.2%) (Fig. 1).
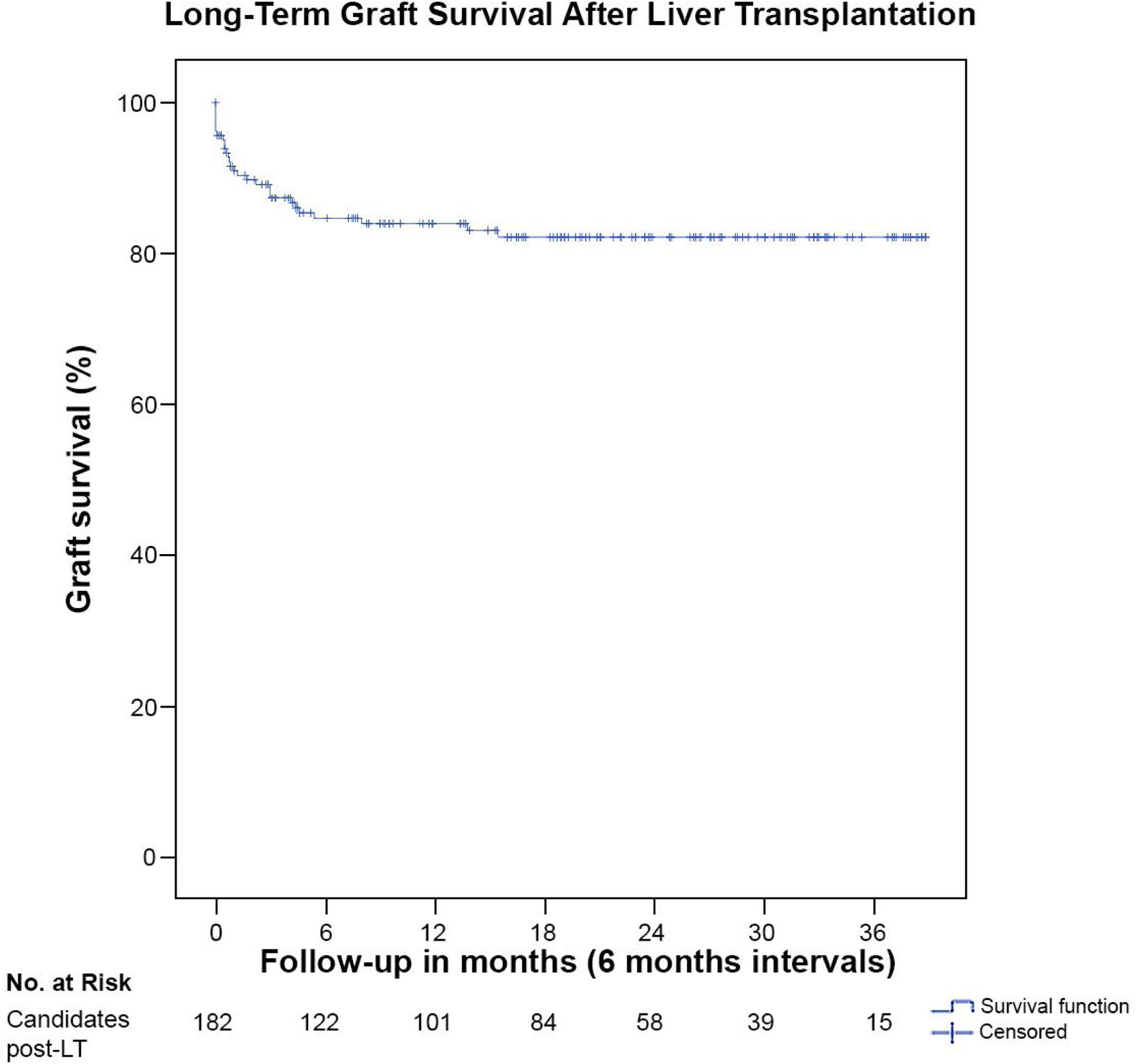
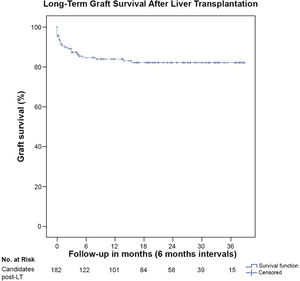
2.4Transplanted groupOut of the 420 candidates who electively enlisted for LT, 182 were transplanted (43.6%), 4 (0.95%) required re-transplantation and 5 (1.19%) needed a double transplant (liver and kidney). Survival at 12 months after LT was 83.2% (Fig. 2). Survival was not significantly different between cirrhotic candidates without exceptions, candidates with HCC and non-HCC plus non-cirrhotic exceptions (p=0.997). The MELD score at LT was 26.74±6.29 (median 26; [IQ] 23.0–30.0). Median follow-up post-LT was 15.75 months ([IQ] 3.68–27.62).
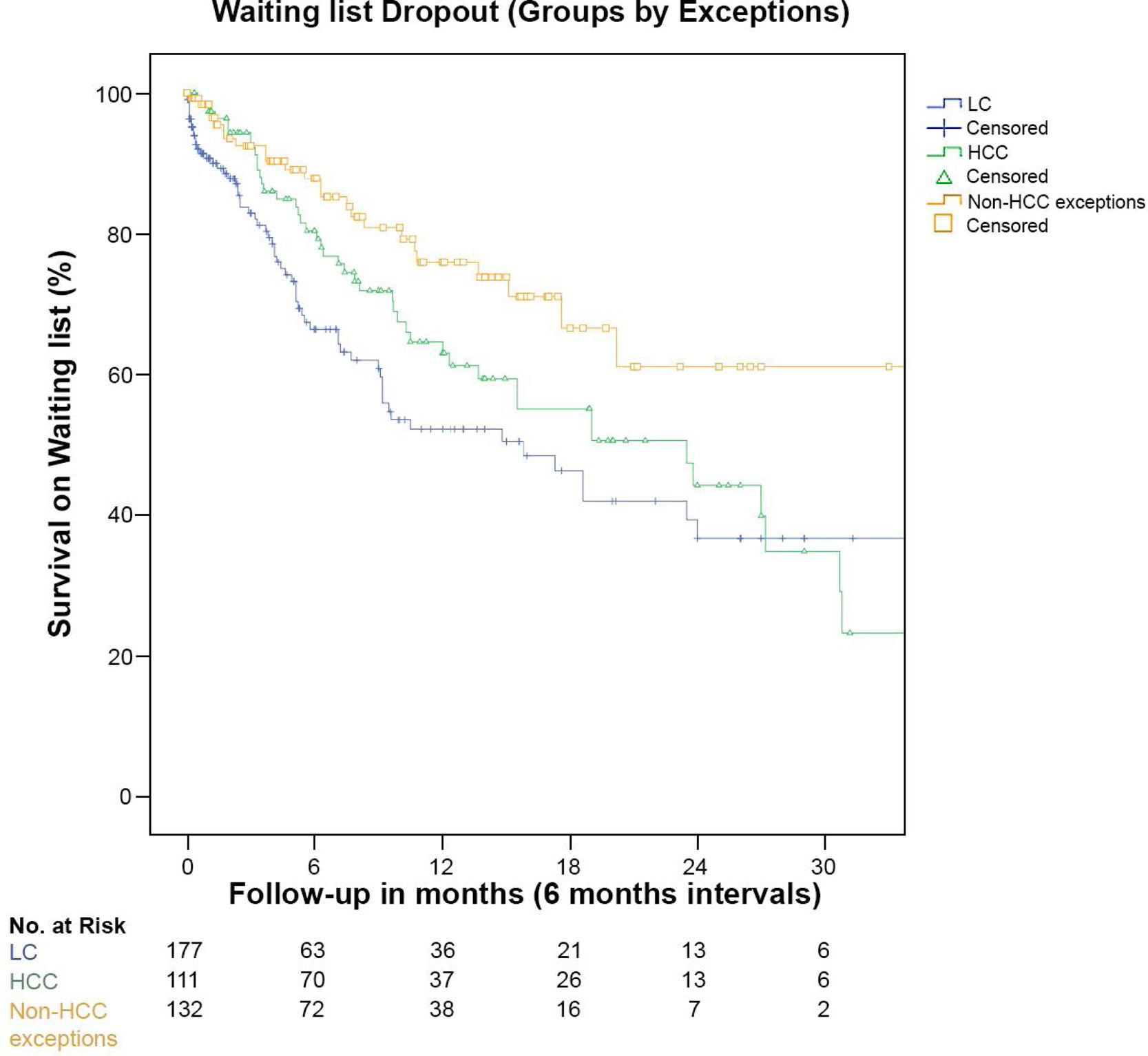
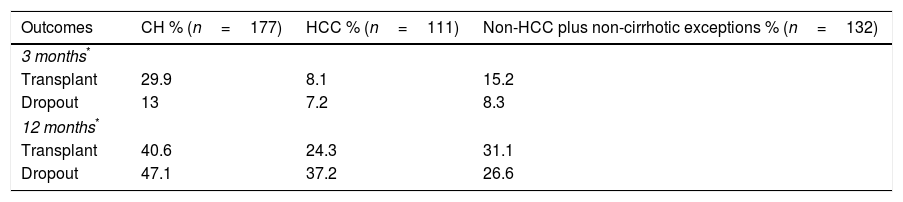
2.5Equity within the waiting listTo identify differences between candidates, we compared the dropout rate between the 3 groups. Dropout for cirrhotic candidates without exceptions was 47.1%, significantly higher than in candidates with HCC and non-HCC plus non-cirrhotic exceptions (37.2% and 26.7%, respectively (p=0.016). Fig. 3 shows the survival rate within the waiting list in the 3 groups of candidates.
We additionally assessed the equity within the waiting list comparing the transplantation rate and dropout at 3 and 12 months. At 3 months, the transplantation rate and dropout was higher in cirrhotics without exceptions than in candidates with HCC and non-HCC plus non-cirrhotic exceptions. Also, at 12 months the liver transplantation rate was higher in cirrhotics without exceptions. All differences were statistically significant (p<0.01) (Table 4).
2.6Association analysis between the MELD score, dropout rate and mortality post-LTWe observed a positive relationship between the MELD score and the probability of transplantation (OR 21.7; p<0.001). There was no relationship between age, sex, the presence of cirrhosis, HCC, other exceptions and probability of transplantation.
The MELD score at the time of LT was not related to mortality post-LT (OR 1.02, IC95% 0.96–1.08; p=0.47); neither was time on the waiting list (OR 1.0, IC95% 0.99–1.0; p=0.52) either. The MELD score at enlistment was also not associated with mortality while on the waiting list (OR 1.0, IC95% 0.96–1.04). Finally, neither age, sex, the presence of cirrhosis, HCC nor other exceptions were related to mortality post-LT.
3DiscussionThe equity organs allocation for LT has been an important issue within the last decades, especially in countries with low donor's rate. The Meld score was adopted, like previously in other countries, as an allocation system for LT in Chile since October 2011 to reduce the high dropout rate observed with the previous allocation system by antiquity in transplant list, while maintaining a high post-LT survival.
The survival post-LT in Chile with the new system is similar to the survival worldwide published in previous reports (83.2% at following 1-year) [18], even though the sicker the candidates are at the moment of transplant. Nevertheless, the dropout rate at 12 months on the waiting list of 37.6%, a higher value than the dropout internationally recommended (lower than 15%). Previously publications do not exist to compare dropout accurately between both periods. However, an unpublished study from a single center showed a dropout rate of 32% at 1-year of follow-up (from 2006 to 2009). Therefore, the dropout rate has not decreased after the incorporation of the MELD system in Chile. Also, the dropout rate observed in our analysis was associated with a long stay enlisted, with an average time of 6.9 months to be transplanted.
The observed differences in transplantation and dropout rates between the 3 subgroups analyzed, could be a reflex of inequity in the assignment in the score for exceptions (Table 4). In fact, cirrhotics without exceptions presented the higher dropout rate despite the higher transplantation rate. This inequity is favored by the MELD exceptions since the assigned score was established arbitrarily by the National Transplant Commission. Thus, when the exceptions are given in great number, disadvantage non-exception candidates and lead to increase dropout and waiting list death. On the other side, the very low donor's rate reported in our country with a subsequent low transplantation rate, which has not been increased in the last 10 years, may explain the elevated dropout rate.
The MELD score was not a good predictor of mortality post-LT. The results are different from previously published studies, which reported a low association [19]. These differences can be explained by the statistic used (ROC curves and c-statistics) and the heterogeneity of studies and centers.
Based on this data, it seems that the MELD scoring is an acceptable allocation system for our country, with respect to equity for organ allocation for liver transplantation and post-LT survival, despite a low donor's rate. However, a strict review of the score allocation to candidates with exceptions should be made to improve the equity of the system nationally.
Future challenges include the re-evaluation of equity allocation and the assessment of other strategies to increase the available grafts as LT from living donors or split-liver transplantation, that can increase the LT rate and decrease dropout [20–23]. Finally, despite the allocation system, it is critically important to establish efforts to educate the population and generate new public policies to increase the donor's rate.
In conclusion, prioritization for LT with the MELD score system has not decreased the dropout rate in Chile, with a persistent low donor's rate. Exceptions given in the system generates inequities in dropout rate, disadvantaging candidates without exceptions. The post-LT survival was similar to the pre-MELD period, despite a higher MELD score at the transplant. Furthermore, there was no association between the MELD score at the transplant and mortality post-LT and between the MELD score at enlistment and dropout within waiting list.AbbreviationsLT liver transplantation Model for End-Stage Liver Disease Transjugular Intrahepatic Portosystemic Shunt Public Health Institute hepatocellular carcinoma primary biliary cholangitis primary sclerosing cholangitis non-alcoholic steatohepatitis spontaneous bacterial peritonitis standard deviation interquartile ranges
This article was not funded.
Conflict of interestThe authors of this article do not have conflicts of interest.
To Mauricio Bouey Carrasco (Toronto, Canada) for the critical proofreading of this manuscript.