While liver transplantation is the definitive therapy for end stage liver disease, it remains a major procedure, with many potential complications. Hospital readmissions after the initial hospitalization for liver transplantation can be associated with adverse outcomes, increased cost, and resource utilization. Our aim was to define the incidence and reasons for hospital readmission after liver transplant and the impact of readmissions on patient outcomes. We retrospectively analyzed 30- and 90-day readmission rates and indications in patients who underwent liver transplant at a large-volume transplant center over a 3-year period. Four hundred seventy-nine adult patients underwent their first liver transplant during the study period. The 30-day readmission rate was 29.6%. Recipient and donor age, etiology of liver disease, biological Model for End-Stage Liver Disease score, and cold ischemia time were similar between patients who were readmitted within 30 days and those who were not readmitted. Readmissions occurred in 25% of patients who were hospitalized prior to liver transplant compared to 30% who were admitted for liver transplant. The most common indications for readmission were infection, severe abdominal pain, and biliary complications. Early discharge from hospital (fewer than 7 days after liver transplant), was not associated with readmission; however, a prolonged hospital stay after liver transplant was associated with an increased risk of readmission (p = 0.04). In conclusion, patients who undergo liver transplant have a high rate of readmission. In our cohort, readmissions were unrelated to pre-existing recipient or donor factors, but were associated with a longer hospital stay after liver transplant.
Liver transplantation (LT) is a life-saving treatment for patients with end-stage liver disease (ESLD). In the United States, over 6,000 LT are performed annually, with an overall annual cost estimated at a quarter of a million USD per patient for the first year after LT, costing Medicare over 370 million USD in the first year after transplant.1 Patients with ESLD often require intensive medical and surgical care before and after LT. While the published data is scarce, readmissions to hospital after initial transplant hospitalization is relatively common.2 Recent legislature in the United States has placed a particular focus on re-admission rates in hospitalized patients: provisions in the Affordable Care Act have established the “Hospital Readmissions Reduction Program”, requiring the Centers for Medicare and Medicaid Services to reduce payments to hospitals with excess readmissions.
Understanding the reasons for hospital readmission and development of strategies to predict and prevent readmis-sions may help in improving the quality of care delivered and potentially reduce the overall cost of care. One strategy is to identify the incidence and risk factors, with the goal of developing clinically applicable algorithms that could help predict which LT recipients are likely to be readmitted. Prior studies have reported predictive factors for readmission in patients with ESLD.3–5 These studies, in part, contributed to practice modifications that have reduced readmissions in this subset of patients.6,7 In contrast, there is limited published information and a relative lack of knowledge regarding reliable prediction or prevention of readmissions post-LT. In the previous studies, pre-existing medical or social conditions, such as portal vein thrombosis, hospitalization within 90 days prior to LT, chronic HCV infection, hypoalbuminemia, elevated creatinine, postoperative complications, and education level were found to be risk factors.2,8 However, the contribution and relative impact of practice-based factors, such as the use of marginal donor allografts, intra-opera-tive transfusion requirements, or so-called fast-tracking protocols, remain unknown.9 The aims of this study were to examine incidence and reasons for hospital readmission in LT recipients and the association between readmis-sions and patient outcomes, and to identify potential predictors of readmissions at a high-volume single center.
Material and MethodsApproval for this study was obtained from the Mayo Clinic Institutional Review Board. Patients who underwent LT at Mayo Clinic in Florida were identified by retrospective analysis of the LT database. All patients who underwent primary LT between January 1, 2009 and December 31, 2011 were included in the study. Post-transplant care, including immunosuppressive therapy and infectious disease prophylaxis, were managed following a standard protocol. Following discharge after transplant hospitalization, patients were followed at least twice a week as an outpatient for the first 3 weeks and then weekly thereafter, as deemed necessary. All hospital readmissions were documented in the electronic medical record (EMR). We also separately examined re-admission rates in patients who received simultaneous liver and kidney transplantation (SLKT), patients who had been hospitalized prior to LT, and patients who received donation after cardiac death (DCD) allografts.
Demographic and clinical information were obtained from the transplant database and EMR. Data collected included recipient age, gender, race, and biological Model for End-Stage Liver Disease (MELD) score at LT. The length of hospital and ICU stay before and after LT were recorded. Information on donor age, gender, race, type of liver allograft (brain-dead, DCD, split, or pediatric allo-graft), cold ischemia time (CIT) and warm ischemia time (WIT) of the liver allograft, and donor risk index (DRI) were obtained.
Information regarding hospital readmissions was extracted from EMR. For the 30-day readmission analyses, we excluded patients who were still in the hospital at day 30 post-LT and those patients who died during LT hospitaliza-tion. For the 90-day readmission analyses, we also excluded patients who were still in the hospital at day 90 post-LT and those patients who died during LT hospitalization.
All LT were performed utilizing the piggyback technique without portacaval shunt, caval clamping, or venovenous by-pass. All liver allografts were reperfused with portal flow followed by arterial flow. Duct-to-duct biliary reconstruction with placement of a transcystic biliary tube was used except in recipients with primary sclerosing cholangitis or when another approach was deemed necessary by the surgeon. Post-transplant management was performed by a dedicated group of experienced physicians, advanced practitioner, and nurses using protocol-driven care for immediate postoperative management, ICU admission, immunosuppression, medication teaching, and discharge coordination.
Statistical analysisContinuous variables were summarized using means and standard deviations, or medians and ranges. Categorical variables were summarized using frequencies and percentages. Baseline donor and recipient characteristics were compared between patients who had readmissions and those that did not. For each variable, odds ratios, p values, and 95% confidence intervals were calculated. The t-test was used to compare continuous variables between those patients who were readmitted and those who were not. A value of p < 0.05 was considered statistically significant. Cox proportional hazard model was used to calculate hazard risk. Kaplan-Meier curves with a log-rank test were used for survival analysis. JMP Pro 9.0 and SPSS 17.0 software (SPSS, Inc., Chicago, IL) were used for the analysis.
ResultsStudy population and readmissionsDuring the 3-year study period, 496 patients underwent LT at our program. We excluded 17 patients undergoing re-transplantation. From the 479 patients who underwent primary LT, 30 patients were still in the hospital by day 30 post-LT, and four patients died during the initial LT hos-pitalization. Median MELD score in patients who stayed in the hospital for over 30 days post LT was 29 (range: 1344). When MELD score of patients who stayed > 30 days post LT was compare with patients who were discharge < 30 days post LT (median 18; range: 6-43), there was a significant difference between these groups (p < 0.0001).
A total of 445 patients were included in our 30-day re-admission analysis and 478 patients were included in our 90-day readmission analysis. The 30-day and 90-day re-admission rates were 29.6 and 42%, respectively. Because the 30-day readmission rate is increasingly being used in literature as a quality metric, we chose this cut-off time for most of our analyses.2
The most common indications for LT were ESLD secondary to chronic HCV (39%), alcoholic cirrhosis (19%), cryptogenic cirrhosis (15%), and non-alcoholic steatohep-atitis (11%). One-hundred and fifteen (26%) patients underwent LT with secondary diagnosis of hepatocellular cancer. The median age of recipients was 58 years (range: 20- 74). The median biological MELD score at time of LT was 18 (range: 6-43). The median CIT and WIT were 6.1 hours (range: 3-12.4) and 31 min (range: 12-75), respectively.
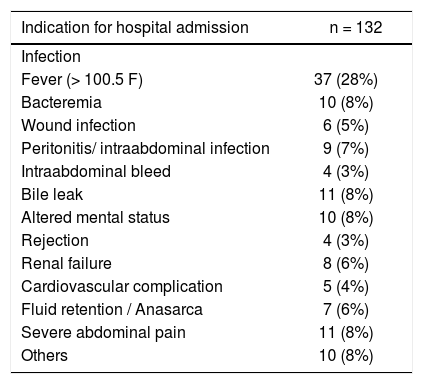
The median time from dismissal after LT hospitaliza-tion to readmission was 8 days (range 1-24). The most frequent indication for readmission to the hospital was infection (fever > 100.5 F°, bacteremia, peritonitis, wound infection non responsive to outpatient treatment or associated with septicemia) followed by severe abdominal pain and biliary complications. Biliary leak and peritonitis were diagnosed in several patients who were admitted with abdominal pain. Table 1 shows the indications for readmission in post-LT patients. All recipients except one were readmitted to our institution.
Indication for readmission within 30 days after liver transplantation.
| Indication for hospital admission | n = 132 |
|---|---|
| Infection | |
| Fever (> 100.5 F) | 37 (28%) |
| Bacteremia | 10 (8%) |
| Wound infection | 6 (5%) |
| Peritonitis/ intraabdominal infection | 9 (7%) |
| Intraabdominal bleed | 4 (3%) |
| Bile leak | 11 (8%) |
| Altered mental status | 10 (8%) |
| Rejection | 4 (3%) |
| Renal failure | 8 (6%) |
| Cardiovascular complication | 5 (4%) |
| Fluid retention / Anasarca | 7 (6%) |
| Severe abdominal pain | 11 (8%) |
| Others | 10 (8%) |
The median duration of initial hospital stay after LT in the study group was 7 days (range: 4- 30). Postoperatively, 248 patients (56%) were transferred to the ICU while 197 patients (44%) were fast-tracked to the surgical ward without being admitted to the ICU. Readmission to the hospital within 30 days occurred in 27% of the patients who were fast-tracked to the surgical ward compared with 32% of the patients who were admitted to the ICU (p = 0.25).
Recipients who had initial LT hospitalization of 7 days or fewer had a 30-day readmission rate of 24%, while recipients who had initial hospitalization of more than 7 days had a 30-day readmission rate of 33% (p = 0.04).
Outcomes of readmissionThree recipients who were readmitted within 30 days post-LT died during the readmission hospitalization; two patients died due to bleeding, and one patient died due to a cardiovascular event.
In order to evaluate the relationship between readmis-sions after LT and subsequent outcomes, we examined patient survival at 1-year. There was no significant difference in 1-year patient survival rate between the recipients who had at least one readmission either within 30 days or within 90 days, compared to those who did not require any re-admission (Figure 1).
Survival after LT in patients with readmission to hospital. A. Patients with re-admissions within 30 days of LT are represented by the blue (upper) line, whereas patients without readmissions are represented by the red (lower) curve. The horizontal axis represents days after LT, whereas the vertical axis represents the surviving fraction. B. Patients with re-admissions within 90 days of LT are represented by the blue (upper) line, whereas patients without readmissions are represented by the red (lower) curve. The horizontal axis represents days after LT, whereas the vertical axis represents the surviving fraction.
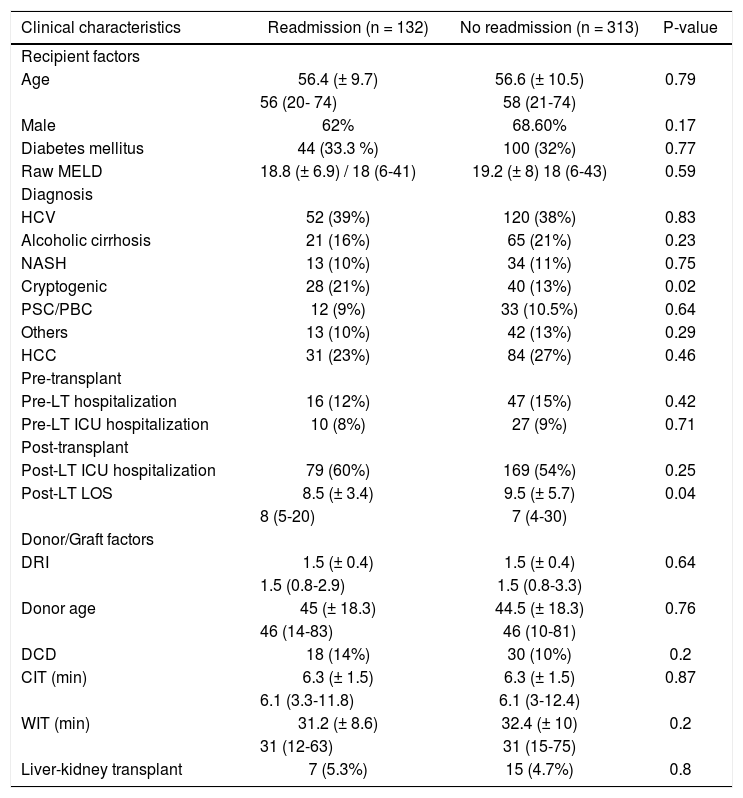
In order to identify potential predictors of 30-day re-admission, we analyzed several donor and recipient factors (Table 2). Patients with cryptogenic cirrhosis appeared to have an increased risk for readmission compared to other etiologies of ESLD; however, this difference did not reach statistical significance (p = 0.09).
Pre-transplant recipient characteristics, donor variables, and post-transplant recipient characteristics in patients who required readmission within 30 days and patient who did not required readmission.
| Clinical characteristics | Readmission (n = 132) | No readmission (n = 313) | P-value |
|---|---|---|---|
| Recipient factors | |||
| Age | 56.4 (± 9.7) | 56.6 (± 10.5) | 0.79 |
| 56 (20- 74) | 58 (21-74) | ||
| Male | 62% | 68.60% | 0.17 |
| Diabetes mellitus | 44 (33.3 %) | 100 (32%) | 0.77 |
| Raw MELD | 18.8 (± 6.9) / 18 (6-41) | 19.2 (± 8) 18 (6-43) | 0.59 |
| Diagnosis | |||
| HCV | 52 (39%) | 120 (38%) | 0.83 |
| Alcoholic cirrhosis | 21 (16%) | 65 (21%) | 0.23 |
| NASH | 13 (10%) | 34 (11%) | 0.75 |
| Cryptogenic | 28 (21%) | 40 (13%) | 0.02 |
| PSC/PBC | 12 (9%) | 33 (10.5%) | 0.64 |
| Others | 13 (10%) | 42 (13%) | 0.29 |
| HCC | 31 (23%) | 84 (27%) | 0.46 |
| Pre-transplant | |||
| Pre-LT hospitalization | 16 (12%) | 47 (15%) | 0.42 |
| Pre-LT ICU hospitalization | 10 (8%) | 27 (9%) | 0.71 |
| Post-transplant | |||
| Post-LT ICU hospitalization | 79 (60%) | 169 (54%) | 0.25 |
| Post-LT LOS | 8.5 (± 3.4) | 9.5 (± 5.7) | 0.04 |
| 8 (5-20) | 7 (4-30) | ||
| Donor/Graft factors | |||
| DRI | 1.5 (± 0.4) | 1.5 (± 0.4) | 0.64 |
| 1.5 (0.8-2.9) | 1.5 (0.8-3.3) | ||
| Donor age | 45 (± 18.3) | 44.5 (± 18.3) | 0.76 |
| 46 (14-83) | 46 (10-81) | ||
| DCD | 18 (14%) | 30 (10%) | 0.2 |
| CIT (min) | 6.3 (± 1.5) | 6.3 (± 1.5) | 0.87 |
| 6.1 (3.3-11.8) | 6.1 (3-12.4) | ||
| WIT (min) | 31.2 (± 8.6) | 32.4 (± 10) | 0.2 |
| 31 (12-63) | 31 (15-75) | ||
| Liver-kidney transplant | 7 (5.3%) | 15 (4.7%) | 0.8 |
Mean (± SD). Median (max-min). MELD: Model of End-Stage Liver Disease. HCV: hepatitis C virus. NASH: non-alcoholic steatohepatitis. PSC/PBC: primary sclerosing cholangitis/primary biliary cirrhosis. HCC: hepatocellular carcinoma. LT: liver transplantation. ICU: Intensive Care Unit. DRI: donor risk index. LOS: length of stay. DCD: donation after cardiac death. CIT: cold ischemia time. WIT: warm ischemia time.
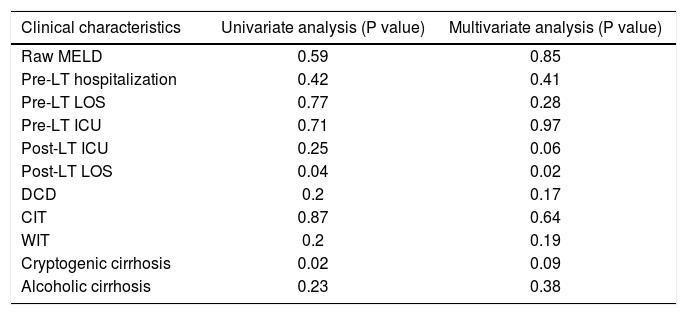
Biological MELD score at the time of LT, recipient age, recipient gender, CIT, WIT, DRI and DCD graft status were similar between the recipients who were readmitted and those who were not readmitted (Table 2). Pre-LT hospitalization and pre-LT ICU stay were not associated with a higher readmission rate. In recipients with prolonged hospital stay post-LT, readmission was more common within 30 days (p = 0.04). Table 3 illustrates single and multivariable analyses for factors associated with 30-day hospital readmission.
Factors associated with 30-day hospital readmission.
| Clinical characteristics | Univariate analysis (P value) | Multivariate analysis (P value) |
|---|---|---|
| Raw MELD | 0.59 | 0.85 |
| Pre-LT hospitalization | 0.42 | 0.41 |
| Pre-LT LOS | 0.77 | 0.28 |
| Pre-LT ICU | 0.71 | 0.97 |
| Post-LT ICU | 0.25 | 0.06 |
| Post-LT LOS | 0.04 | 0.02 |
| DCD | 0.2 | 0.17 |
| CIT | 0.87 | 0.64 |
| WIT | 0.2 | 0.19 |
| Cryptogenic cirrhosis | 0.02 | 0.09 |
| Alcoholic cirrhosis | 0.23 | 0.38 |
MELD: Model of End-Stage Liver Disease. LT: liver transplantation. LOS: length of stay. ICU: Intensive Care Unit. DCD: donation after cardiac death. CIT: cold ischemia time. WIT: warm ischemia time.
In a separate analysis, we compared LT alone recipients and SLKT recipients; readmissions within 30-days occurred in 125 of the 423 patients (29.5%) who received an LT alone and in 7 of 22 patients (31.8%) who received SLKT. The median post-transplant hospital stay for the LT alone group was 7 days (range: 4-30), whereas the median post-transplant hospital stay for the SLKT group was 10 days (range: 5 20).
A total of 48 patients received liver allografts from DCD donors. There was a trend toward a higher rate of 30-day hospital readmission in the recipients of DCD al-lografts compared to that of recipients of donation after brain death allografts (38 vs. 29%); however, this difference did not reach statistical significance (p = 0.2).
Impact of pre-transplant hospitalizationOf the 445 patients in our study group who underwent primary LT, 382 were outpatient at the time they were called for LT, whereas 63 were already hospitalized at the time of LT. Of the 63 patients who had previously been hospitalized, 16 patients (25%) were readmitted within 30 days, compared with 116 patients (30%) of the 382 who had not been previously hospitalized. This difference was not statistically significant (P = 0.42).
DiscussionGiven the paucity of data on readmissions after LT, this report provides a systematic analysis of readmissions in consecutive patients from a large-volume LT center.2,8 Like in other medical conditions, hospital readmission data may be used as a measure of quality of health care in patients receiving a LT.10 In addition to resource utilization and healthcare expenditures, readmissions can affect a health care service’s patient referral pattern in the medium- to long-term. Therefore, it is critical to understand the reasons for readmissions in every medical and surgical practice. Understanding these reasons may allow identification of preventable causes that can then lead to improvements in overall patient care and satisfaction and a decrease in resource utilization. To the best of our knowledge, there have been only a few reports in the scientific literature looking into reasons for readmissions after liver transplantation.2
In the MELD era, due to the complexity of patients and the increase in resource utilization, the cost of LT has significantly increased.11,12 Reimbursement from private health insurances is established by contractual agreements with case rates for different stages of transplant care.13 Unfortunately, these rates do not necessarily reflect the increased costs of LT.11,14 In addition, transplant centers are forced to limit costs by developing efficient practice pathways. Reducing readmission rates offers an opportunity to reduce costs associated with LT. Thus, strategies to avoid unnecessary readmissions are warranted, and mandate careful examination of potential risk factors and determinants of readmission, along with their impact on outcomes and resource utilization.
Due to the complexity of LT patients, it is expected to have a high readmission rate after LT.2,8 Even though the criteria for hospital readmission vary per institution, the threshold for readmission in this group of patients is low due to their recent surgery and immunosuppressive state.
In order to understand the risk factors and impact of our clinical practice model, which emphasizes early discharge from hospital, we analyzed the relationship between length of stay of the initial hospitalization and subsequent readmission. There was an increased frequency of readmissions at 30 days in the recipients who had a longer hospital stay after LT compared to the recipients who were discharged earlier (p = 0.04). Recipients with a complex surgical, medical or psychosocial complication post-LT may require a longer hospital stay and an increased risk for readmission. Their condition at the time of LT, as measured by the biological MELD score, was not associated with readmission. Buchanan, et al., also found that MELD score was not a significant predictor of readmission following LT.15 On the other hand, the 30-day readmission analysis did not include patients who remained in the hospital for longer than 30 days and who had higher MELD scores at the time of transplant. Prior studies had showed the association between a higher MELD score with higher costs and resource utiliza-tion11,15 and the need for further institutional care upon discharge.2
Certain factors, including, but not limited to, overall functional status of a recipient, previous significant en-cephalopathy, and sarcopenia, are not captured by the MELD score and should be the focus of future studies about length of hospitalization and readmission rates.16 In addition, the use of immunosuppressive agents following LT can be associated with complications, such as rejection, infection, or renal dysfunction that could result in readmissions after initial hospitalization. Such complications may not develop within the first few days after transplant. However, to prolonged hospitaliza-tion after LT may not necessarily be helpful in reducing readmission rates. Based in our data, reasons for re-admission do not appear to be predictable at the time of the initial hospitalization.
Readmissions after transplantation have been previously shown to be associated with pre-existing portal vein thrombosis, hypoalbuminemia, or renal dysfunction.2 However, these data have been retrospectively obtained over an extended period of time during which perioperative care and post-transplant management have evolved. In contrast, the current study draws from a single practice that utilizes consistent, protocol-driven care with a dedicated and experienced team involved in peri- and post-transplant management, providing the ability to examine the impact of any future practice modifications to further reduce readmission rates.
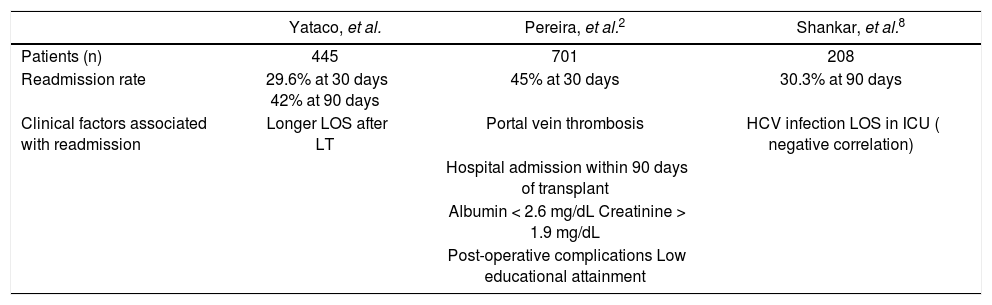
The main limitation of this study is its retrospective nature. Furthermore, this was a single-center experience, and other LT programs may have higher or lower rates of readmission as reported in previous studies (Table 4).2,8 This variability could be partially attributed to differences in MELD score and inpatient hospital status at the time LT.
Readmission rates and clinical factors.
| Yataco, et al. | Pereira, et al.2 | Shankar, et al.8 | |
|---|---|---|---|
| Patients (n) | 445 | 701 | 208 |
| Readmission rate | 29.6% at 30 days 42% at 90 days | 45% at 30 days | 30.3% at 90 days |
| Clinical factors associated with readmission | Longer LOS after LT | Portal vein thrombosis | HCV infection LOS in ICU ( negative correlation) |
| Hospital admission within 90 days of transplant | |||
| Albumin < 2.6 mg/dL Creatinine > 1.9 mg/dL | |||
| Post-operative complications Low educational attainment |
HCV: hepatitis C virus. ICU: Intensive Care Unit. LOS: length of stay. LT: liver transplant.
While the validity of the use of readmission rates as a metric of quality of care may be unrelated to the quality of care during the transplant admission, transplant programs must have quality initiatives in order to decrease readmis-sion rates. Recognizing LT recipients who may be at risk for readmission may provide opportunities for reduced costs by deferring early discharge. As this study shows, preexisting recipient or donor factors do not adequately enable prediction of LT recipients who may require re-admission. Thus, continuation of a strategy to emphasize early discharge accompanied by close follow-up and re-admission for any emerging issues continues to be our current practice. Identification of additional potential factors not currently captured in databases should be the future focus to better predict and prevent readmissions.
ConclusionIn conclusion, patients who undergo LT have a high rate of readmission. This high readmission rate may be due to the complexity of LT patients and the low threshold for readmission in LT centers. In our cohort, re-admissions were unrelated to pre-existing recipient or donor factors, but were associated with a longer hospital stay after liver transplant. Further studies are needed to evaluate possible strategies to decrease readmission rates and reduce cost.
Financial SupportNone.
Conflict of InterestThe authors declare no conflicts of interest.
Abbreviations- •
CIT: cold ischemia time.
- •
DCD: donation after cardiac death.
- •
DRI: donor risk index.
- •
EMR: electronic medical record.
- •
ESLD: end-stage liver disease.
- •
LT: liver transplantation.
- •
MELD: Model for End-Stage Liver Disease.
- •
SLKT: simultaneous liver and kidney transplantation.
- •
WIT: warm ischemia time.
None.