Cholangiocarcinoma (CC) is the second most common primary hepatic malignancy. Although the frequency of malignancy is generally increased in chronic liver disease, CC rarely presents in Wilson disease (WD). The incidence of hepatic malignancy in WD is only 1.2%, with CC accounting for 0.5%. A 66 year old male with history of hypertension, diabetes, and compensated cryptogenic cirrhosis presented with acute onset dyspnea and pleuritic chest pain. He was incidentally found to have a sizeable mass in the right hepatic lobe. Ultimately, a liver biopsy revealed dense demoplasia and increased mucin production, consistent with diagnosis of CC. Biopsy also demonstrated increased copper deposition consistent with WD, explaining the patient's underlying cirrhosis. Unlike other forms of chronic liver disease where incidence of liver cancer is increased, the lower rate of malignancy seen in WD may be explained by a protective effect of copper in WD. Copper acts to both directly stabilize DNA and inhibit angiogenesis. In this case, it is possible that the degree of copper deposition in his liver was mild, causing cirrhosis and the chronic liver inflammation that caused his CC. However, it may not have been sufficient to “protect” against development of CC.
Cholangiocarcinoma (CC) is the second most common primary hepatic malignancy [1]. Although the frequency of malignancy is generally increased in chronic liver disease, CC rarely presents in Wilson disease (WD) [2]. The incidence of hepatic malignancy in WD is only 1.2%, with CC accounting for 0.5% [2].
WD presents with neurologic symptoms including tremor, gait imbalance, dysarthria, parkinsonism, as well as psychiatric symptoms including psychosis [3]. They may also present with Kayser–Fleischer rings, or corneal copper deposits [3]. Only about 60% of patients with WD experience hepatic symptoms and 45% have neuropsychiatric features [3].
2Case descriptionA 66 year old male with history of hypertension, diabetes, and compensated cryptogenic cirrhosis presented with acute onset dyspnea and pleuritic chest pain. He denied cough, congestion, fever, chills, orthopnea. Of note, the patient was recently diagnosed with metastatic cancer of unknown primary origin after suffering cord compression syndrome due to a metastatic spine lesion. He was treated with radiation and was undergoing further evaluation as an outpatient prior to this presentation. His past surgical history was significant for laparoscopic cholecystectomy. He had no family history of liver disease or malignancy. He denied history of smoking and heavy alcohol use.
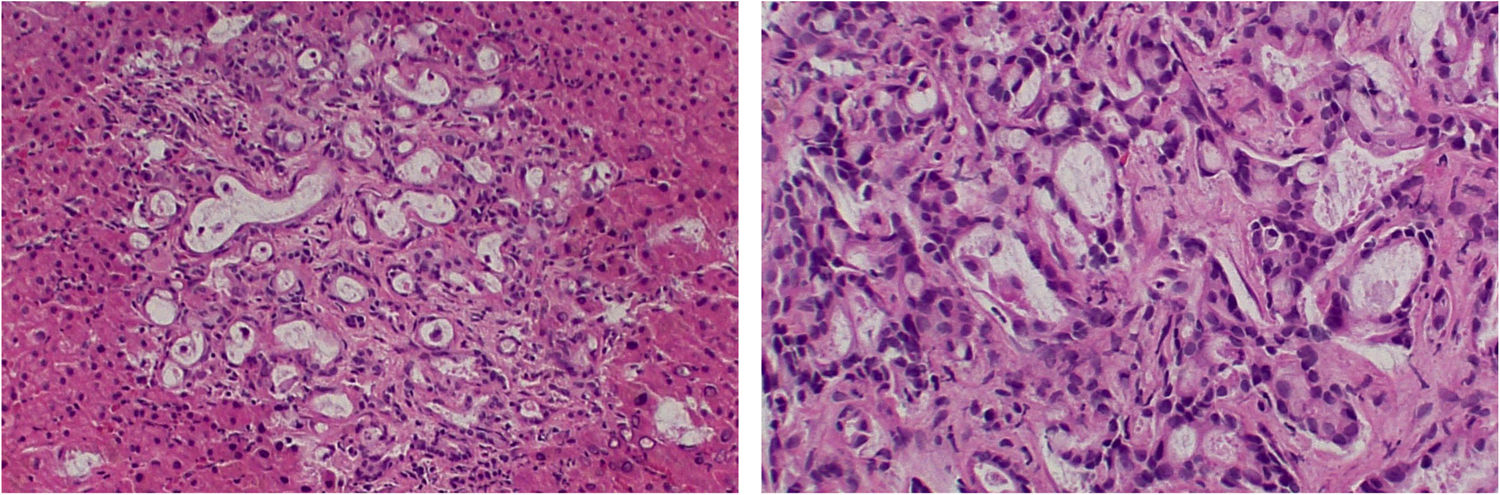
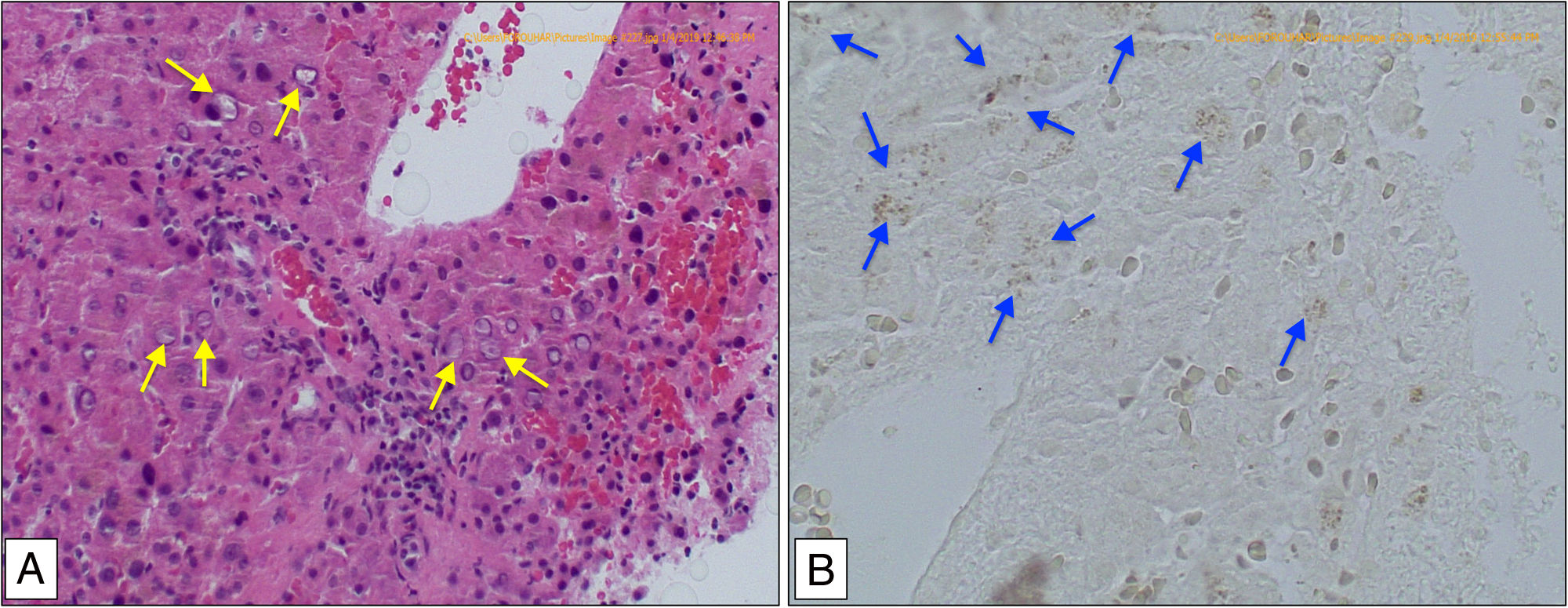
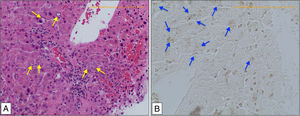
The patient was afebrile, tachycardic to 125bpm, tachypneic to 24bpm and hypoxic to 80% on room air. Physical exam was notable for diffuse bilateral rhonchi, with a normal eye exam and neuropsychiatric exam. Computed tomography (CT) of the chest showed a 5.8cm hypodensity in the right hepatic lobe, innumerable punctate pulmonary nodules, and diffuse bony metastasis. His laboratory results were remarkable for an elevated alkaline phosphatase to 252IU/L, with normal aspartate aminostransferase, alanine aminotransferase and bilirubin. His CEA was 6.7ng/mL and CA19-9 was 19,653U/mL. Colonoscopy was negative. PET/CT scan confirmed hypermetabolic uptake in the liver lesion and extensive lesions consistent with metastases throughout the lungs and axial skeleton. A liver biopsy revealed an area of dense demoplasia and increased mucin production with staining positive for CK 7 and CK 19, consistent with diagnosis of CC (Fig. 1). In sections without neoplasia, the liver biopsy demonstrated very large nuclear pseudo-inclusions and Mallory bodies in the periportal areas as well as periportal fibrosis (Fig. 2). These histopathologic findings are characteristic of WD. Rhodainine staining was performed and confirmed accumulation of copper in the liver (Fig. 2). In this case the histopathologic findings confirmed the diagnosis of WD, and no further serologic, urinary or genetic testing was performed. Furthermore, the diagnosis of WD explained the patient's underlying cirrhosis (formerly cryptogenic).
In Panel A, an H&E preparation (400×) shows large nuclear pseudo-inclusions and Mallory bodies in the periportal areas (red arrows), which are characteristic findings in WD. In Panel B, a Rhodanine preparation (400×) demonstrates increased copper deposition, depicted as gray granules (blue arrows).
Having presented with late stage, widespread metastatic disease, our patient's prognosis was very poor. He was stabilized from a respiratory perspective with supportive measures and was discharged with hospice care. His family declined palliative treatment for his malignancy. He ultimately died from respiratory complications of metastatic cholangiocarcinoma due to significant tumor burden in the lungs. Furthermore, given the very late discovery of WD, he did not receive any treatment for copper overload.
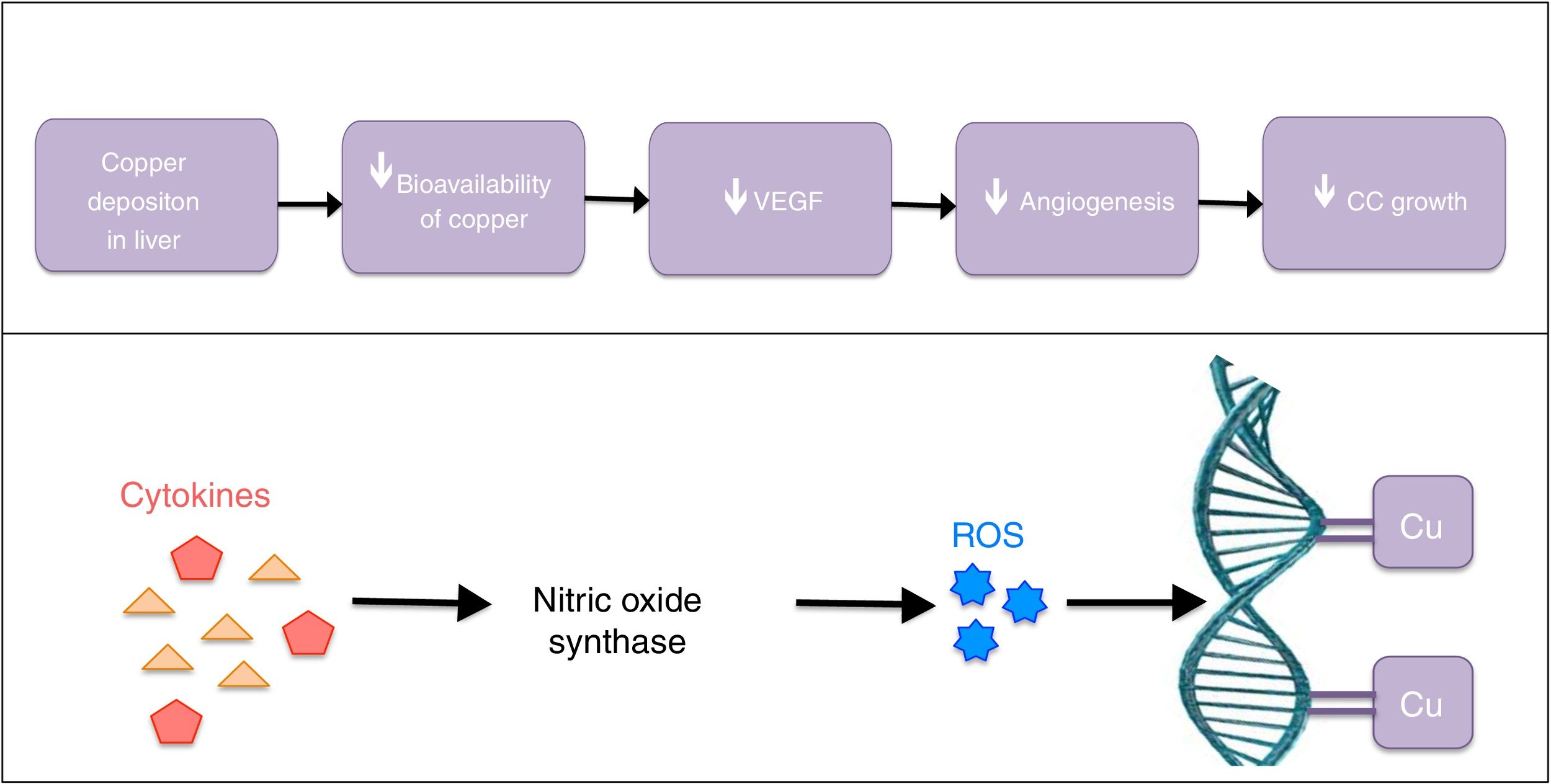
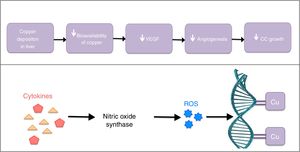
3DiscussionCommon risk factors for CC include viral and alcoholic hepatitis, hepatolithiasis, primary sclerosing cholangitis, parasitic liver disease and cystic liver disease [1]. In these conditions, chronic inflammation and bile stasis stimulate cytokines, leading to formation of reactive oxygen species (ROS) [4]. ROS damage DNA and allow for neoplastic growth of cholangiocytes. Unlike other etiologies of chronic liver disease, WD has a low prevalence of CC. This may be explained by a protective effect of copper in WD, which occurs by two mechanisms (Fig. 3). First, copper acts to stabilize DNA by direct binding to DNA [5]. This helps to prevent damage by ROS. The second protective mechanism is by inhibition of angiogenesis, which is a copper dependent process. As copper is deposited in the liver and other tissue, the serum copper level is decreased. Therefore there is less copper available to stimulate vascular endothelial growth factor (VEGF) expression [5].
In this case, WD had not been diagnosed prior to this presentation. The liver biopsy diagnosed CC and incidentally revealed WD. He also did not display any of the typical neuropsychiatric or ophthalmic signs and symptoms of WD. It is possible that the degree of copper deposition in his liver was mild, causing cirrhosis and the chronic liver inflammation that caused his CC. However, it may not have been sufficient to “protect” against development of CC.
AbbreviationsCC cholangiocarcinoma Wilson disease computed tomography reactive oxygen species vascular endothelial growth factor
Mavilia – drafting article, literature review.
Sharma – clinical care of the patient involved, major revisions.
Forouhar – development of figures, critical analysis of histopathologic data, revisions.
Informed consentInformed consent was obtained from this patient's healthcare representative prior to submission of this report.
Conflicts of interestThe authors have no conflicts of interest related to this work.