Objective. To determine intrafamilial seropositivity of HBV and HCV and to compare them in families of infected persons with HBV and HCV in Hamadan clinic of hepatitis.
Material and methods. In this analytic cross-sectional study, 651 family members of 200 HBV and HCV infection index cases were entered into the study and after signing an informed consent, they were referred to Blood Transfusion Center. With completion of laboratory tests, interviewers filled the questionnaires.
Results. One hundred and eighteen (20.5%) and 107 (18.6%) family members were HBsAg and HBcAb positive respectively. 21 (3.6%) were isolated HBcAb positive. Only one person (1.3%) was HCVAb positive. The general rate of infection in family members of HBV infected people (atleast one case) (49.4%) was significantly higher than that of HCV infected people (3.3%), p < 0.001. Interspouses transmission was evaluated and prevalence of interspouses HBV and HCV infection were 32.3 and 8%, respectively.
Conclusion. Intrafamilial and interspousal seropositivity of HBV is obviously more than those of HCV. More attention should be paid to screening and risk lowering activities particularly about HBV infected people and their families.
Hepatitis B and C virus infection are of the most substantial problems in public health. In Iran, hepatitis B prevalence is low as 1.07% in Shiraz and as high as 8.96% in Toiserkan.1 There are three main routes of HBV transmission including blood transfution, sexual contacts, and horizontal. In endemic regions of the world such as Africa, Greece, and Hong Kong, vertical majority of cases acquire HBV infection at birth or after early childhood (i.e., both vertical and horizontal transmission in early life). In contrast, in North America and Western Europe, sexual contact is dominant mode of transmission.2-4
In a prospective study in North India, 265 household contacts of 91 HBsAg-positive patients were evaluated and the highest prevalence of HBsAg was seen in pediatric age groups and especially in siblings (48.3%).5 In other study in city of Nahavand in Hamadan Province (in west of Iran), family members of 115 HBs Ag positive were studied and the results showed that 11% of them were HBs Ag positive and sons and daughters were the most frequent seropositive relatives.6
The prevalence of HCV infection in Iran is estimated 0.59-0.8%.7 Common routes of HCV infection are infected blood donor, needle-stick injuries among health professionals, tattooing, intravenous drug abuse, hemodialysis or organ transplantation. HCV infection transmits through sexual contacts, although it seems sexual contact does not play an independent role in the spread of HCV infection in the family setting.8,9 40-45% of HCV infections occur through persons with no clear risk factor that has been defined.10 Vertical transmission has also been demonstrated;11 however, HCV infection is still spreading in population through other transmission routes that is unknown and is not completely explored.
A study of 300-household contacts of 60 index cases in Southern Iran (Khuzestan) estimated1.33% HCV seroprevalence among the household contacts of HCV-seropositive index cases.12 A study in Egypt reported highest prevalence of anti-HCV in the world between 6 to 28% (mean 22%) in parenteral antischisto-somal therapy.13 Other studies such as Italian local health district study have reported a lower prevalence of 4.7% HCV infection in household contacts of index cases.14
To our knowledge, little information is available about HBV and HCV infection due to contacts of patients infected with HCV and HBV in Hamadan province (in west of Iran). This study aimed to determine the prevalence of HBV and HCV infection in families with a member who was confirmed to have HBV and HCV infection. In addition, we compared intrafamilial transmission of HCV with HBV infection.
Materials and MethodsThis analytic cross-sectional study was conducted during a one year period (2006) on 200 families of 200 index cases with HBV and HCV infection (130 and 70 families, respectively) that referred to hepatitis clinic in Hamadan Province.
After taking the approval of hepatitis clinic and health authorities of the city, patients who were known cases of HBV and HCV infections and had registered in clinics were enrolled into study. For HBV infection, HBsAg positive, anti-HBc positive, both HBsAg and anti-HBc positive were selected.
For detecting HCV infection, we just measured HCV-Ab and positive cases for HCV-Ab were entered in our study. The selected patients were contacted at their residence and after given description of the study, they were asked to encourage their families to participate in the study.
After signing the consent forms by the family members, they were referred to Blood Transfusion Center. The virologic markers of HBV (HBsAg, HBsAb, HBcAb) and HCV (HCV-Ab) were assessed.
A questionnaire including demographic data, marital status of patients and their household contacts was developed. After completion of laboratory tests, subjects were referred to clinic and interviewers filled the questionnaires.
HBsAg detection was performed by Diasorin kit through sandwiched ELISA. HBsAb and HBcAb levels were measured by Diasorin kit through sandwiched non competitive ELISA and Diasorin kit through competitive ELISA, respectively. Antibodies to HCV were detected employing a commercially available second-generation enzyme immunoassay (EIA, Abbott).
The data were analyzed with SPSS, version 10. Comparison was made using chi-square test. P< 0.05 was considered statistically significant.
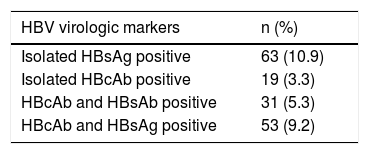
ResultsFive hundred and seventy five family members of HBV index cases were enrolled into study. Table 1 shows distribution of hepatitis B virologic markers in family members of index cases.
Total rate of infection was 28.7% in the population (HBV infection was defined as participants with HBsAg positive/anti-HBc positive/both HBsAg and anti-HBc/both HBsAb and HBcAb positive). Of 76 family members of HCV index cases 1.3% was HCV Ab positive.
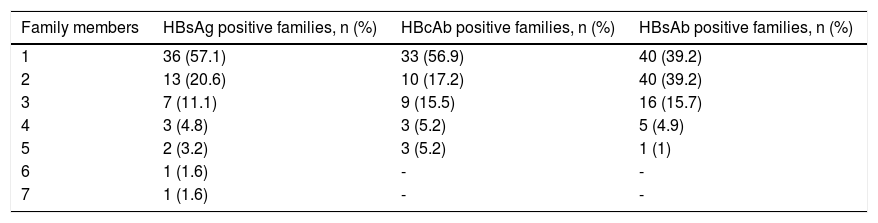
Of 170 HBV index case families, 63 families (37.1%) were HBsAg positive, 58 families (34.1%)HBcAb positive and 102 families (60%) were HBsAb positive. Table 2 shows distribution of hepatitis B virologic markers based on number of family members in families of index cases.
Frequency distribution of hepatitis B virologic markers based on number of family members in familiesof index cases.
| Family members | HBsAg positive families, n (%) | HBcAb positive families, n (%) | HBsAb positive families, n (%) |
|---|---|---|---|
| 1 | 36 (57.1) | 33 (56.9) | 40 (39.2) |
| 2 | 13 (20.6) | 10 (17.2) | 40 (39.2) |
| 3 | 7 (11.1) | 9 (15.5) | 16 (15.7) |
| 4 | 3 (4.8) | 3 (5.2) | 5 (4.9) |
| 5 | 2 (3.2) | 3 (5.2) | 1 (1) |
| 6 | 1 (1.6) | - | - |
| 7 | 1 (1.6) | - | - |
Thirty seven families (53 family members) had active infection with HBV (including HBsAg and HBcAb positive members) and 32 families (36 family members) were immunized following infection with HBV (including HBsAb and HBcAb positive members). In overall, of 170 HBV index case families, 84 families (49.4%) were infected with HBV (families with HBsAg and HBcAb positive, isolated HBsAg positive, isolated HBcAb positive, HBcAb and HB-sAb positive). Of 30 HCV index case families, 1 family (3.3%) was HCVAb positive.
It should be mentioned that, of 130 spouses of HBV index cases enrolled into our study 50 spouses (32.3%) were infected with HBV. 12 spouses of HCV index cases were evaluated and only 1 spouse (8%) was infected with HCV.
At last, total rate of infection in family members of HBV index cases was significantly higher than family members of HCV index cases (p < 0.001).
DiscussionDistribution of HBV varies widely in different parts of the world. Iran has an intermediate prevalence of HBV. The relationship between chronic HBV infection and cirrhosis/hepatocellular carcinoma has been presented by many authors, giving this infection an important cause of morbimortality and of major concern to public health.15,16 HBV is the most common cause of hepatocellular carcinoma in Iran.
HCV infection, a world wide spread liver disease, may also be transmitted by the parenteral and other routes similar to that of HIV and HBV. Infection is often asymptomatic in adults. About 50-70% of mild infections progress to chronic phase. Long term observations of natural history of the disease have confirmed that HCV is a risk factor for cirrhosis and primary hepatocellular carcinoma. This problem shows the importance of the transmission of HBV and HCV infection through household contacts.
The results of our study suggest that prevalence of HBsAg is 20.1% in our study. This is obviously higher than HBsAg prevalence in a study of 246 family members of HBsAg positive subjects that was 6.5%. 90% of adults with HBV infection will completely resolve the infection and will not become chronic carriers. So, estimation of HBsAg is not alone complete indicator of disease burden. Prevalence of HBcAb, in addition to HBsAg can help to identify disease burden more reliably. Prevalence of HBcAb in above study was 22.6% which is obviously higher than 3.3% in our study. With considering these statistics, it seems the burden of HBV infection in two populations is similarly high.17
Our study estimated the overall rate of HBV infection 49.4% in families of HBV-seropositive index cases. A study on 78 families (506 members) of immigrating Ethiopian Jews to Israel reported the overall rate of infection, in families of HBV-seropositive index cases 67.8%.18 The overall rate of infection is lower in families of our study. It may be because of better socioeconomic status, appropriate vaccination of children, early detection of disease and lower amount of high risk behaviors in Iranian families in comparison to Ethiopian Jews families.
Results of a study between 2000-2001 in Turkey, showed the prevalence of HBsAg and HBV infection among the family members (29.6 and 43.8%, respectively), were higher than the control group (9.6 and 29.7%).19 Based on our findings, the prevalence of HBsAg and total rate of infection was 20.5 and 28.7%, respectively, which was lower than the Turkey study.
One of the most important routes of HBV infection transmission is between spouses. It is important to clarify role of this route because it is preventable by appropriate screening and immunization of high risk population. In our study, 12.3% of spouses were HBsAg positive. A same study in Nahavand of Hamadan province showed HBsAg is positive in 10% of spouses.6 Whereas prevalence of HBV infection is 2.3% in general population,20 it is obvious that seropositivity of HBV is HBV is high in spouses, so interspouses transmission may be an important route. It seems several factors are responsible for this difference. In Hamadan, there is high prevalence of IV drug abusers and co-addiction between spouses that support non sexual routes of transmission. Also, because of poor knowledge about HBV infection and routes of transmission, early detection of disease is difficult.
A Turkey study showed that 33.3% of spouses were HBsAg positive and HBV infection were 90% prevalent20 that is high in comparison to 12.3 and 32.3% in our study.
The higher prevalence of HBsAg infection among spouses may be due to sexual transmission in menstrual period in other countries. In Iran, because of cultural and religious aspects, this way of intrafamilial seropositivity has a low prevalence. Length of marriage is also important in seropositivity and in our study most of spouses were newly-wed. Besides, in developed countries, HBV screening is performed before marriage to early diagnose the disease.
This study estimated 1.31% HCV seroprevalence among the household contacts of HCV-seropositive index cases, which is approximately similar to a study performed in southern Iran.12 Our results differ from those studies reporting a 16 and 20% rate of HCV infection in family members of adult patients with chronic hepatitis C.21,22 This difference could be explained by some limitations, i.e., we did not perform recombinant immunoblot assay (RIBA) to confirm HCV exposure, or polymerase chain reaction (PCR) to detect HCV infected individuals. Low titer infectivity of HCV in blood and variable sensitivity of the hepatitis C radioimmunoassay used for detecting HCV infection are other probable causes.23
Our results demonstrate that spouses of anti-HCV positive patients were more likely to be infected with HCV than other family members and the infection rate was 8%. A study on 263 cases of acute hepatitis C showed 13% of cases had sexual exposure as a risk factor for infection with HCV. Also, serum samples of seven of 24 positive partners evaluated and 5 of them had genotype concordance with identity in the genomic sequence of 97.8 to 99.3%. this finding supports sexual contacts as a route of HCV transmission.24 Other authors reported that spouses of seropositive patients have the highest risk of HCV infection that is concurrent with our findings.12,25 The prevalence of positive anti-HCV in spouses is different and may be a consequence of many factors such as sexual behavior and duration of marriage.26,27
Our data suggest that risk of HBV intrafamilial seropositivity through sexual and non sexual contacts is lower than that of HCV. It indicates that HBV is more prevalent in our population and transmit through more routes of transmission.
Our study had some limitations; first, we did not carry out PCR or RIBA to confirm HBV and HCV exposure. Second, positive Anti-HCV increases in spouses with their length of marriage but we did not consider it in our study. At last, in investigation of intrafamilial transmission of HBV, sequence analysis and amino-acid variation of the HBV core gene is the only way to confirm HBV intra-familial transmission, but due to lack of sufficient resources in present study, this procedure was not possible.28
ConclusionIntrafamilial seropositivity of HBV is higher than HCV in our studied population. More attention should be paid to screening especially in prisoners, IV drug abusers and those who wants to get married. If immunization performs in first months of marriage, protecting level of antibodies will not be detectable for months and seropositivity occurs in 15% of cases despite enough immunization. Therefore, adequate information should be given. In addition, families should become aware of other routes of hepatitis transmission as well as common routes e.g. sexual and blood-contaminated equipment.
Financial SupportsNone.
AcknowledgmentThe authors would like to thank Farzan Institute for Research and Technology for technicalassistance.