Hepatitis E virus produces an emerging health problem, knowledge about epidemiology of hepatitis E virus infections in the USA and Latin America is still limited. The wide-ranging clinical manifestations lead to an extensive underestimation of the global seroprevalence. Clinical and diagnostic accuracy are critical to improve patient management.
Hepatitis E virus produces an emerging health problem, the World Health Organization (WHO) estimates 20 million of infections by Hepatitis E virus (HEV), over 3 million symptomatic cases and 70,000 HEV-related deaths each year. HEV is the major cause of enterically transmitted hepatitis world wide, and is not limited to countries with low sanitary standards. HEV has been detected in environmental samples (water) in several countries from Europe and Asia, representing a risk factor for waterborne infection. While hepatitis E virus infections are relevant in Europe, knowledge about epidemiology of hepatitis E virus infections in the USA and Latin America is still limited [1].
The HEV is classified in the genus Orthohepevirus, with four species that affect different hosts (A–D). The specie with the highest rank of hosts is Orthohepevirus A, which includes 7 reported genotypes that infect humans (1, 2, 3, 4 and 7), pigs (3 and 4), rabbits (3), wild boar (3, 4, 5 and 6), mongooses (3), deer (3), yaks (4) and camels (7) [2]. Genotypes 1 and 2 are responsible for epidemics outbreaks, mainly in developing countries, and have been isolated from humans exclusively, zoonotic transmission due to contact with infected animals and consumption of contaminated undercooked or raw meat has been identified as an important risk factor, especially in industrialized countries [3].
HEV affects mainly young and middle aged adults, mainly between 15 and 40 years of age, however, cases of chronic infection of HEV have been reported in immunosuppressed people, as in people with chronic liver disease, organ transplantation or people infected with the human immunodeficiency virus in which the disease rapidly evolves to liver cirrhosis, loss of the transplanted organ and death. HEV (genotype 3) seroprevalence was higher in livertransplant recipients compromised by cirrhosis [4].
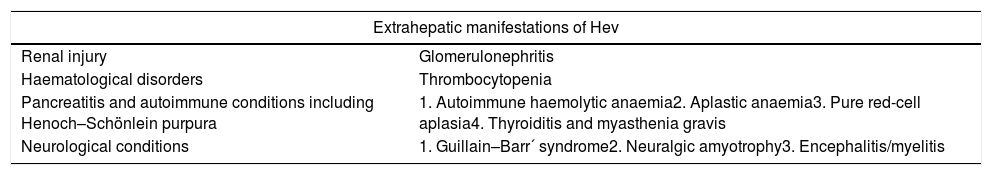
HEV genotypes 1 and 2 are known as a cause of acute hepatitis and fulminant hepatic failure in pregnant women during large waterborne outbreaks in developing countries, transmitted vertically and resulting in water-borne sporadic cases or large epidemics [5]. HEV is also recognized as transfusion transmitted virus. Extrahepatic manifestations of HEV infection have been reported in both acute and chronic cases Table 1[3].
Extrahepatic manifestations of HEV [3].
| Extrahepatic manifestations of Hev | |
|---|---|
| Renal injury | Glomerulonephritis |
| Haematological disorders | Thrombocytopenia |
| Pancreatitis and autoimmune conditions including Henoch–Schönlein purpura | 1. Autoimmune haemolytic anaemia2. Aplastic anaemia3. Pure red-cell aplasia4. Thyroiditis and myasthenia gravis |
| Neurological conditions | 1. Guillain–Barr´ syndrome2. Neuralgic amyotrophy3. Encephalitis/myelitis |
Recently, it has been reported that the seroprevalence in Latin America was significantly smaller than USA. Patients in the USA had a more than doubled estimated seroprevalence (up to 9%) than those in Brazil (up to 4.2%) and Mixed Caribbean (up to 1%). A comparison with published data from Europe demonstrated that anti-hepatitis E virus seroprevalence in the USA and Europe did not differ significantly (OR: 1.33 (0.81–2.19), P=.25), while rate in South America was significantly lower than that in Europe (OR: 0.67 (0.45–0.98), P=.04). HEV infection has been reported in several Latin American countries. The highest seroprevalence has been reported in Nicaragua and Chile (12%), however the anti-HEV seroprevalence rate has continuously increased over time between 1995 and 2015 [6]. HEV genotype 3 being the most frequent genotype in the region, identified both in humans and pigs. Cases of viral hepatitis reported in Mexico are typically identified as hepatitis A, B and C. However, unspecified cases are reported annually. In Mexico, HEV genotype 2 is considered endemic, though it's the prevalence is not well known, prevalence reported in adults 10–36% [7] and the information on the prevalence of HEV in paediatric patients is scarce, our working group has found a seroprevalence of 3%, unpublished data.
ConclusionsKnowledge about epidemiology of hepatitis E virus infections in the USA and Latin America is still limited, it is likely to represent a massive underestimatation of the true global burden of disease, epidemiologically the HEV incidence is low in humans but serological data show a high proportion of subclinical infections. Clinical and diagnostic accuracy are critical to improve patient management and reduce the burden of HEV infection worldwide. Also, developing specific tests with high sensitivity and specificity for detecting viral RNA or anti-HEV antibodies is important.