Background and aims. Despite effective vaccine available, hepatitis A remains a significant cause of morbidity and mortality worldwide including acute liver failure, transplantation and death. Vaccination rates for hepatitis A in the general population are low. Rates of hepatitis A vaccination in healthcare personnel (HCP) are unknown. We studied vaccination rate to hepatitis A in a cohort of HCP at a large US academic center.
Material and methods. An anonymous survey was circulated between 499 HCP at-risk of hepatitis A exposure at our Institution. Results were corrected for non-response rate and compared with the general US population using the 2007 CDC-National Immunization Survey. Rate of hepatitis A vaccination was compared with Institutional rate of vaccination for the Influenza 2009-2010 season.
Results. Rate of vaccination for hepatitis A in HCP was 28.8% (response rate 41.4%; 207/499), with 58.9% having completed the full series and 24.7% being tested for post-vaccination immunity. Acceptance rate among non-vaccinated subjects was 70.7%. HCP hepatitis A vaccination rate was statistically greater than the national general population (28.8 vs. 12.1%, p ≤ 0.031). A statistically significant greater vaccination rate was found among US-born responders vs. foreign-born HCP (34.3 vs. 19.3%, p = 0.0324). Vaccination for hepatitis A was statistically inferior to that of Influenza (28.8 vs. 90%; P = 0.01). Conclusions. HCP have statistically higher vaccination rate for hepatitis A than the general population, but overall protection remains suboptimal with vaccination rate below those for mandatory vaccines. Further studies to determine whether hepatitis A vaccine is cost-effective in HCP are recommended.
Hepatitis A is a significant cause of morbidity and mortality worldwide despite availability of vaccines that are both safe and effective. Epidemiology of hepatitis A, once a typical disease of childhood, has changed dramatically in the last decades leaving a significant number of adults unprotected from the infection. Adults affected from hepatitis A may miss up to 33 days from work.1 Though most patients with hepatitis A recover without chronic sequelae, the infection can be fatal in some patients and in the United States it is estimated that 100 patients die each year from liver failure due to hepatitis A.2 Overall case-fatality for hepatitis A is 0.6% in adults and reaches up to 1.5% in patients older than 60 years of age.3
Although the vaccine for hepatitis A is easily available it is not required by current guidelines for HCP. This is in contrast with the higher risk of contracting the infection in those departments where HCP handle body fluids, such as endoscopy, transplantation division, emergency room or operating room. At least 26 hospital outbreaks of hepatitis A have been published.4 Therefore unprotected HCP may pose a significant risk to patients in the event of such an outbreak, in particular in those areas of the world with suboptimal hospital infection control precautions. We performed a single center cross-sectional study assessing immune protection from hepatitis A in healthcare personnel by distributing a survey to HCP at risk of exposure to the disease.
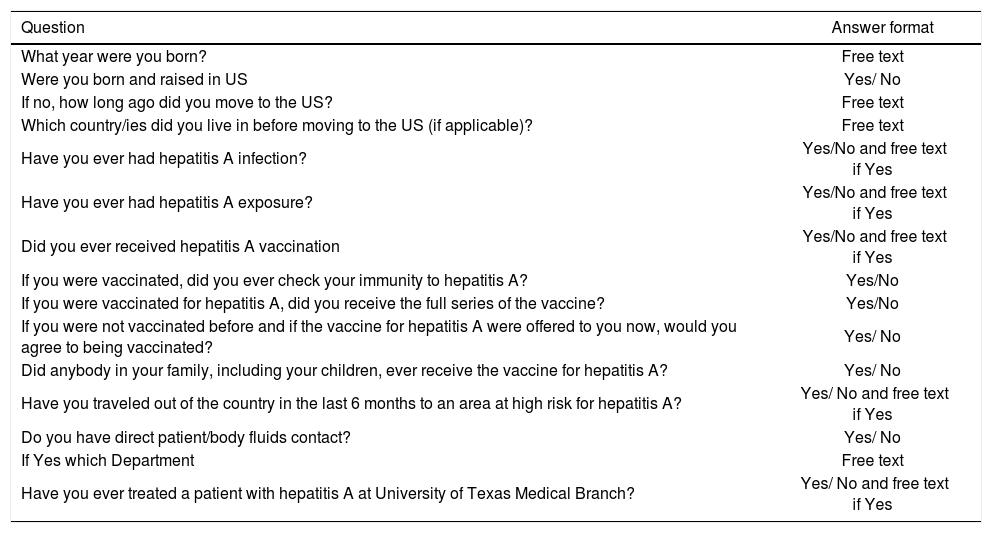
Material An MethodsAn anonymous survey (Table 1) was circulated between 499 HCP at risk of hepatitis A exposure in our Institution, University of Texas Medical Branch (UTMB), Galveston, Texas, United States of America. The institutional review board committee approved protocol of the study and informed consent was obtained from each participant. The following departments were surveyed: emergency department, operating rooms, Intensive care unit, Obstetrics and neonatology services, endoscopy, pathology, transplant clinic, medicine/surgery floors and clinics. Results were corrected for non-response rate. Comparison was performed with the 2007 CDC-Na-tional Immunization Survey. Data of annual vaccination rate for Influenza season 2009-2010 at our Institution were obtained by analysis of the University of Texas Medical Branch epidemiology department database. Statistical analysis was performed by Wald test and Pearson chi-square.
| Question | Answer format |
|---|---|
| What year were you born? | Free text |
| Were you born and raised in US | Yes/ No |
| If no, how long ago did you move to the US? | Free text |
| Which country/ies did you live in before moving to the US (if applicable)? | Free text |
| Have you ever had hepatitis A infection? | Yes/No and free text if Yes |
| Have you ever had hepatitis A exposure? | Yes/No and free text if Yes |
| Did you ever received hepatitis A vaccination | Yes/No and free text if Yes |
| If you were vaccinated, did you ever check your immunity to hepatitis A? | Yes/No |
| If you were vaccinated for hepatitis A, did you receive the full series of the vaccine? | Yes/No |
| If you were not vaccinated before and if the vaccine for hepatitis A were offered to you now, would you agree to being vaccinated? | Yes/ No |
| Did anybody in your family, including your children, ever receive the vaccine for hepatitis A? | Yes/ No |
| Have you traveled out of the country in the last 6 months to an area at high risk for hepatitis A? | Yes/ No and free text if Yes |
| Do you have direct patient/body fluids contact? | Yes/ No |
| If Yes which Department | Free text |
| Have you ever treated a patient with hepatitis A at University of Texas Medical Branch? | Yes/ No and free text if Yes |
US: United States.
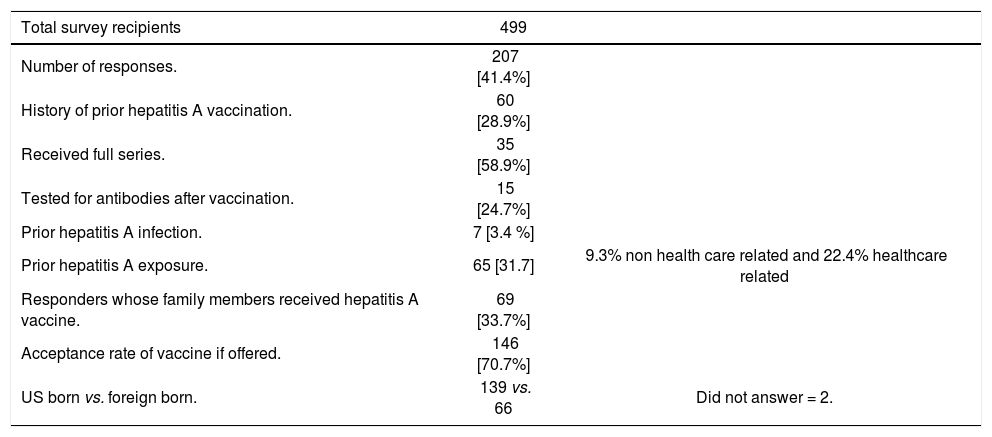
207 subjects at risk of exposure returned the surveys (response rate 41.4%). Rate of vaccination for hepatitis A was 28.9%. Among the subjects who were vaccinated 58.9% received the full series and 24.7% were eventually tested for post-vaccination immunity. Prior hepatitis A infection was reported in 3.4%. Prior exposure to hepatitis A was reported in 31.7% (9.3% non-healthcare related, 22.4% healthcare related). 33.7% of responders had family members who had received hepatitis A vaccination, including children. Acceptance rate (non vaccinated subjects who would accept receiving the vaccine now) was 70.7%. Results are summarized in table 2.
| Total survey recipients | 499 | |
|---|---|---|
| Number of responses. | 207 [41.4%] | |
| History of prior hepatitis A vaccination. | 60 [28.9%] | |
| Received full series. | 35 [58.9%] | |
| Tested for antibodies after vaccination. | 15 [24.7%] | |
| Prior hepatitis A infection. | 7 [3.4 %] | |
| Prior hepatitis A exposure. | 65 [31.7] | 9.3% non health care related and 22.4% healthcare related |
| Responders whose family members received hepatitis A vaccine. | 69 [33.7%] | |
| Acceptance rate of vaccine if offered. | 146 [70.7%] | |
| US born vs. foreign born. | 139 vs. 66 | Did not answer = 2. |
US: United States.
HCP hepatitis A vaccination rate was statistically greater than the national general population (28.8 vs. 12.1%, p ≤ 0.031, Wald chi-square, CASRO res-ponse rate 41 vs. 31%). On multivariate analysis a statistically significant higher vaccination rate was found among US-born responders when compared to foreign-born (34.3 vs. 19.3%, p = 0.0324 Pearson chi-square). There was no statistical difference in vaccination rates of younger (< 35 year of age) vs. older responders. No difference was found in vaccination rate among different departments.
DiscussionAn average of 28,000 cases of hepatitis A were (range 23,112-35,821) reported every year in United States in the decade 1987 to 1997. The incidence has been decreasing over the last decade with an incidence rate of 1.0/100,000 and estimated 2,979 new cases reported in 2007. This decline is mainly attributed to increased vaccination of children as suggested by the Advisory Committee on Immunization Practices.5 Although rates have been declining in the last two decades, hepatitis A remains a significant public health concern as sporadic outbreaks of food borne hepatitis A have caused significant morbidity and mortality including acute liver failure, transplantation and death. Hospital outbreaks of hepatitis A have also been reported in the past but nosocomial transmission of hepatitis A is now considered rare and HCP don't have increased prevalence of the disease.5 For these reasons hepatitis A is not a mandatory vaccination for HCP in the US. The Advisory Committee on Immunization Practices recommends the vaccine only to those individuals who have additional risk factors, either by life-style or occupation. The current guidelines are approved by the American Academy of Family Physicians, American College of Obstetricians and Gynecologists, and American College of Physicians.6
Vaccination rate for hepatitis A in the general US population, according to the 2007 National Immunization Survey vaccination coverage for hepatitis A among adults between 18 and 49 years of age, is 12.1%.7 We found a significant higher rate of vaccination in HCP when compared to the general population. However a high percentage of responders did not follow up with complete vaccine series and follow up serology monitoring. Attitude towards hepatitis A vaccination was also low in HCP, with a third of non-vaccinated responders not interested in the vaccine. This may be due to the consideration that hepatitis A incidence is declining in the community or that universal precautions are sufficient in preventing transmission of the disease in the hospital setting. The CDC does not even recommend passive immunization when a patient with hepatitis A is admitted to a hospital, where “staff should not routinely be administered Immunoglobulin; instead, careful hygienic practices should be emphasized”.
Current recommendations from Advisory Committee on Immunization Practices may also play a role in undermining the importance of hepatitis A vaccination in HCP. On the other hand we expected an increased awareness toward hepatitis A since our Institution serves an area in South Texas and the border region with Mexico, and is at higher risk for hepatitis A infection according to the Texas Department of State Health. Prior exposure to the disease was reported in 31% of the subjects to our survey. Overall these data indicate an increased but still su-boptimal rate of vaccination for hepatitis A in HCP. Whether this lower rate reflects general attitude toward non-mandatory vaccinations or is specific to hepatitis A is to be determined. The Advisory Committee on Immunization Practices recommends health care workers, including students, to be vaccinated for measles, mumps, rubella, hepatitis B, varicella, influenza, and pertussis. A recent article published in Annals of Internal Medicine found rates for mandatory vaccinations in U.S. medical colleges and nursing schools to range between 90 and 66%.8 Similarly vaccination rate for influenza in HCP at our Institution, where Flu vaccine was mandatory in the 2010/2011 season was 90%.
Though the incidence of hepatitis A is expected to decline from now on, it will also lead to declining prevalence of antibodies to hepatitis A in the community leading to an adult population with limited immunity to the virus. This is reflected by the fact that only 431 of the 2,979 cases reported in 2007 were children under 15 years of age.9 Hepatitis A infections in adults tend to be more severe and would lead to increased costs, mortality and morbidity.10 This needs to be taken into consideration while discussing the cost effectiveness of hepatitis A vaccine.
Since Hepatitis B is a mandatory vaccination at most healthcare facilities it could be cost effective to give a combination vaccine with both hepatitis A and B as suggested by Jacobs, et al.11 Another strategy that could be cost effective was suggested by Rajan, et al., where vaccination would be offered in populations when the prevalence for hepatitis A immunity is < 45%, while when immunity is > 45% screening followed by vaccination could be offered.12
ConclusionsHealth Care Personnel have statistically higher vaccination rate for hepatitis A than the general population, but overall protection for hepatitis A appears to be suboptimal with vaccination rate well below compared to mandatory vaccines. Further studies to determine whether hepatitis A vaccine is necessary and cost-effective in Health Care Personnel are needed.
Abbreviations- •
HCP: Health care personnel.
- •
US: United States.
- •
CDC: Center for diseases control.
- •
CASRO: Council of American Research Organizations.
None.