Hepatic perforation is an unusual complication of woman pregnancy associated with a poor outcome. A comprehensive review of epidemiology, clinical spectrum, diagnostic methods and therapeutic options is presented in this short paper.
Spontaneous hepatic rupture is a very uncommon complication of pregnancy requiring special diagnostic accuracy and a precise timing and efficacy in therapeutic resource utilization to reduce its high mortality and to offer satisfactory results to both mother and newborn. The first clinical case of hepatic rupture was described by Abercrombie J, on 1844.1
Epidemiology and clinical presentationOnly 200 cases of hepatic rupture have been reported in the world literature. However, it is possible that some cases related to general perinatal mortality without further clarification may correspond to hepatic hemorrhage and therefore a sub-registration of real number of cases must be suspected. The most of the obstetricians haven’t had a personal experience with these cases because of the low incidence reaching about 1 case in 45,000-225,000 births.2,3 In a Chilean Obstetric Hospital (Santiago Oriente Hospital at the University of Chile) were detected 3 cases in 92,587 patients, indicating an incidence of one in 30,863 childbirths.4
The majority of affected women are multiparous, 3040 years old, with a clinical context of pre-eclampsia or severe eclampsia. This condition also can occur on the first pregnancy. The complication is frequently associated to HELLP Syndrome (Hemolysis, elevated liver enzymes, low platelet count) which appears during the advanced phase of pregnancy or immediate puerperium.5-7
The clinical presentation is a sudden onset of abdominal pain on right hypochondrio irradiated to right shoulder, arterial hypertension and clinical data of low heart flow. During the initial biochemical evaluation the most frequent laboratory findings are severe anemia and abnormalities on coagulation tests including thrombocytopenia, protrombine and tromboplastine tests prolongation, hipo-fibrinogenemia, and depending on severity other abnormalities of primary fibronolysis or consumption coagulopathy.8-10
Disease physiopathology. Based on few available histopathologic studies Rademaker4 has proposed different physiopathologic stages of this serious disease. A first hepatic ischemic stage has been identified probably related to previously present preeclampsia or eclampsia giving rise to small zones of liver infarction. This first phase is followed by a second phase of cicatrization, tissue remodeling and rising vascularization. Nevertheless, due to the poor tissue healing capacity associated to sustained intrahepatic hypertension and serious disorder of coagulation (in cases associated to HELLP syndrome) multiple micro-hemorrhages are induced giving rise eventually to a large hepatic hematoma (third phase). Finally, the persistent and growing hepatic hematoma perforate the capsule of Glisson causing peritoneal irritation and secondary hipovolemic shock (fourth stage).
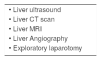
Diagnostic tests(Table I). Due to the seriousness of disease an agressive multidisciplinary approach is required. In standard cases, during an emergency caesarean operation intraperitoneal hemorrhage of diverse degrees of intensity is detected (100 to 450 mililiter of blood in cavity, have been reported). Sometimes only a great hepatic subcapsular hematoma is visualized. Using complementary imaging studies (ultrasound, tomography or resonance) it is generally possible to confirm the existence of large hepatic hematomas and by using selective angiography, identify an active site of hemorrhage.11-13
Differential diagnosis. In initial stages of diagnosis, amebian hepatic abscess have been suspected. Nevertheless once having all the diagnostic studies a clear hemorrhagic nature of the lesion is detected. An original diagnostic and therapeutic flow chart used in Santiago Oriente Hospital at the University of Chile proposes immediate interruption of pregnancy by caesarean operation. In some cases 10 mg i.v. of dexametasone every 12 hours has been administered aiming aim to improve platelet recovery and to contribute to shorten the evolution time of HELLP syndrome. Depending on the patient clinical evolution diverse diagnostic and therapeutic laparotomies will be necessary.5
Complications. The most frequent complications are septic shock, intravascular coagulation and acute renal failure. A case of hemolytic micro-angiopathic anemia has been reported. Additionally, diverse degrees of pulmonary affection including pleural effusion, and acute respiratory distress syndrome confirm the need for a multidisciplinary approach and management on an Intensive Care Unit.12,13
Treatment strategies(Table II). The most frequent treatment is surgical and of palliative nature since hepatic hematoma perforation is usually diagnosed as a medical finding done by the gynecologist in the course of an emergency caesarean operation. Compression with abdominal towels and in some cases positioning of polypropylenes meshes has been performed. When it is possible and appropriate suture of the tear and eventually tying of the hepatic artery must be done. Once identified the serious nature of the hemorrhage a careful support with blood transfusions, platelet, blood concentrates is mandatory. Activated factor VII,13 selective transarterial embolization,12 partial liver resection, Argon beam coagulation14 and even emergency liver transplantation15 have been performed with successful results. The right hepatic lobe, mainly the anterior and superior wall, is the most frequently affected, representing 75% of the cases.
Therapeutic strategies used in hepatic hemorrhage or hepatic rupture during pregnancy.
| • Observation |
| • Immediate interruption of the pregnancy |
| • Hepatic compression |
| • Hepatic artery tying |
| • Selective transarterial embolization |
| • Argon beam electrocoagulation |
| • Factor VIIa administration |
| • Liver resection |
| • Liver transplantation |
Maternal-fetal prognosis. Fetal mortality depends on prompt diagnosis and implementation of optimal therapeutic measures. In the oldest series, mortality fluctuated between 59 and 85 percent.12,13 Up to 35% of perinatal mortality and important hypoxic-ischemic encephalopathy cases have been reported. In one of the most recent Mexican series (4 cases of the Hospital Central Militar), Gonzalez-Martinez G et al, reported a 25% of maternal-fetal mortality.3 This remarkable decrease in mortality is explained by accuracy in diagnosis and effective therapeutic measures.
In relation to surgical prognosis and effectiveness it is important to differentiate between hepatic surgeries in acute trauma conditions in which liver tissue is healthy compared to a friable and congestive tissue found in the setting of pregnancy. For that reason, it is not easy to confront tissue planes and much less to compress satisfactorily when tieing or trying an effective surgical hemostasia. In some cases fibrinolysis or consumption coagulopathy may be induced which worsen enormously the prognosis of the disease.
In summary, the hepatic hemorrhage and hepatic rupture of pregnancy is a rare but catastrophic complication of pregnancy. A high index of suspicious and immediate recognition is fundamental to proper diagnosis. Finally, multidisciplinary approaches in medical and surgical therapeutic measures are fundamental to achieve excellent success and decrease the high mortality rates.