Background and aim: Abnormal liver function tests (LFTs) and gastrointestinal (GI) symptoms have been reported up to 50% in patients with COVID-19, and in 5% they can precede respiratory symptoms. The objective of this work is to describe the LFTs and GI symptoms of patients with COVID-19 and their association with admission to the intensive care unit (ICU) and mortality.
Material and Methods. We conducted a retrospective, cross sectional, descriptive study, using files from patients with a positive Gen Finder COVID-19 test, admitted to Medica Sur Clinic and Foundation between March 13th through May 14th, 2020. We performed descriptive analysis of data and its association with clinical outcomes.
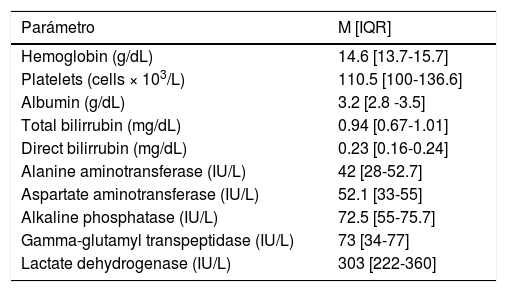
Results: A total of 108 patients with COVID-19 were identified; 68.5% (n=74) were men, the mean age was 53±14 years and the body mass index was 28.6±5.8kg/m2. The most frequent comorbidity was hypertension with 24% (n=26). The presence of comorbidities was associated with risk of ICU admission (OR 3.9 [95% CI 1.6-9.9], p=0.002). The most frequent symptoms were cough (72.2%, n=78), fever (69.4%, n=75) and dyspnea (48.1%, n=52). At least one abnormal LFT was present in 94% (n=103) of patients at admission, the most frequent was LDH (88.9%, n=96), AST and GGT (63%, n=65), which are summarized in Table 1. Patients presented abnormal LFTs and respiratory symptoms in 48.1% (n=52), while 16.6% (n=18) presented abnormal LFTs without respiratory symptoms. Among GI symptoms, 37% (n=4) reported at least one, including diarrhea (28.7%, n=31), hyporexia (9.3%, n=10), nausea (8.3%, n=9) or vomiting (4.6%, n=5). Of patients admitted to the ICU (n=39), 27.5% (n=10) presented at least one GI symptom. Mortality was 7.4% (n=8). No associations were found between abnormal LFTs, GI symptoms, and outcomes of mortality and ICU admission.
Initial liver function tests of patients with COVID-19 (n=108).
| Parámetro | M [IQR] |
|---|---|
| Hemoglobin (g/dL) | 14.6 [13.7-15.7] |
| Platelets (cells × 103/L) | 110.5 [100-136.6] |
| Albumin (g/dL) | 3.2 [2.8 -3.5] |
| Total bilirrubin (mg/dL) | 0.94 [0.67-1.01] |
| Direct bilirrubin (mg/dL) | 0.23 [0.16-0.24] |
| Alanine aminotransferase (IU/L) | 42 [28-52.7] |
| Aspartate aminotransferase (IU/L) | 52.1 [33-55] |
| Alkaline phosphatase (IU/L) | 72.5 [55-75.7] |
| Gamma-glutamyl transpeptidase (IU/L) | 73 [34-77] |
| Lactate dehydrogenase (IU/L) | 303 [222-360] |
Conclusions: In patients with COVID 19, the presence of metabolic comorbidities confers a higher risk of ICU admission, in contrast to abnormal LFTs and GI symptoms that were not associated with clinical outcomes.
Conflicts of interest: The authors have no conflicts of interest to declare.