A 45 year old female with a history of systemic lupus erythematosus on immunosuppression, presented to our center for evaluation of giant cavernous hepatic hemangiomas. She was first diagnosed with these at the time of her second child’s birth 12 years previously. While initially asymptomatic, she had gradually developed abdominal distension and progressive discomfort, back pain, early satiety and fatigue. At presentation, she was anemic, with a hemoglobin of 7.2 g/dL.
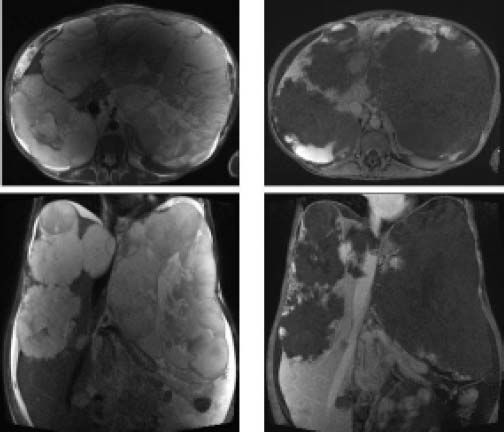
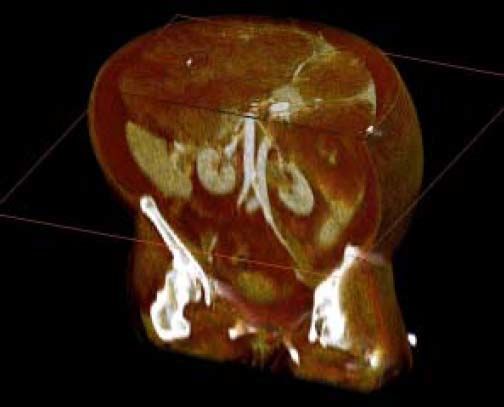
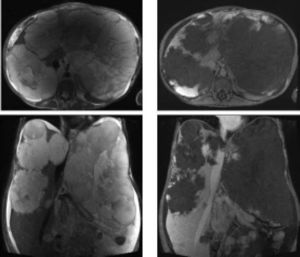
Magnetic resonance imaging of the abdomen showed multiple extremely large hepatic cavernous hemangiomas resulting in marked hepatomegaly (Figure 1). The liver completely occupied the upper abdomen with displacement of both kidneys and the spleen inferiorly. Despite significant mass effect, the pancreas and kidneys appear normal. The liver extended along the anterior margin of the stomach and displaced both the stomach and pancreas posteriorly and inferiorly. The right lobe of the liver extended into the right pelvis, with a few small hemangiomas measuring 2 to 3 cm in the inferior segments. The largest hemangioma replaced the left lobe of the liver and measured approximately 22 x 16 x 29 cm. Small hemangiomas were also present in the spleen.
There was significant hypertrophy of the hepatic arteries with an accessory left hepatic artery arising from the left gastric artery. The inferior vena cava was patent with a normal course and caliber. The right hepatic vein was patent, but the middle and left hepatic veins were indiscernable. There were patent accessory hepatic veins. The portal venous system was patent with a diminutive/compressed left portal vein.
DiscussionOur recommendations were to consider primary surgical resection because of symptomatic progression over an extended period of several years on watchful waiting. Given the potential risk of hepatic decompensation with surgical resection, we further recommended liver transplant evaluation prior to resection.
Hepatic hemangiomas are the most common benign liver tumors of mesenchymal origin, but most of these are small.1 Giant hemangiomas, greater than 5 cm in size are less common. These tumors are asymptomatic in the majority of cases. Unresected hemangiomas do not usually become symptomatic or significantly increase in size.2 MRI provides a highly sensitive and specific non-invasive test to confirm the diagnosis. If characteristic features are noted on MRI, a fine-needle aspiration biopsy may not be needed.3
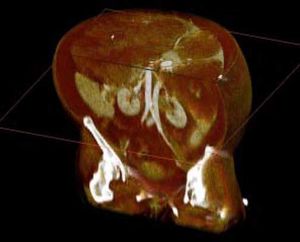
The approach to management of giant hepatic hemangiomas should be tailored on a case-by-case basis (Figure 2). A primary consideration is the presence of symptoms such as pain or abdominal distension. A conservative management is often warranted for asymptomatic tumors.2 However, in some cases, symptoms may be inappropriately attributed to these tumors. Intervention may be considered in the presence of disabling symptoms, liver dysfunction, Kasabach-Merritt syndrome or increasing size. The preferred approach remains undefined, with several options available. Indications for surgical resection include an atypical appearance suspicious for malignancy, or acute hemorrhage, thrombosis or rupture.4 Surgical resection has been suggested to be comparable to enucleation.5 Safe resection requires attention to vascular exclusion, and an assessment of vascular anatomy is essential. The risk of intraoperative blood loss is related to adjacency to major blood vessels. Other management approaches that may be considered for giant hepatic hemangiomata include hepatic artery embolization as a debulking therapy in cases with favorable vasculature,6,7 radiation therapy,8 or the use of interferon alpha-2a.9 The reported safety and efficacy of these approaches has been variable. Finally, liver transplantation is mandated in patients with unresectable giant or extensive multiple hemangiomas, or those with inadequate functional remnant after resection.10 Good outcomes have been reported in the literature.11