Aim. To evaluate the value of D-dimer and P-selectin in cirrhotic portal hypertension (PHT) patients for prediction of portal vein thrombosis (PVT) after devascularization.
Material and methods. 137 patients with cirrhotic PHT who undergone devascularization from January 2012 to April 2014 were retrospectively reviewed, all of them were divided into two groups (PVT group and non-PVT group) by Doppler ultrasonography (DU) examination. The level of D-dimer and P-selectin was tested during the peri-operative period.
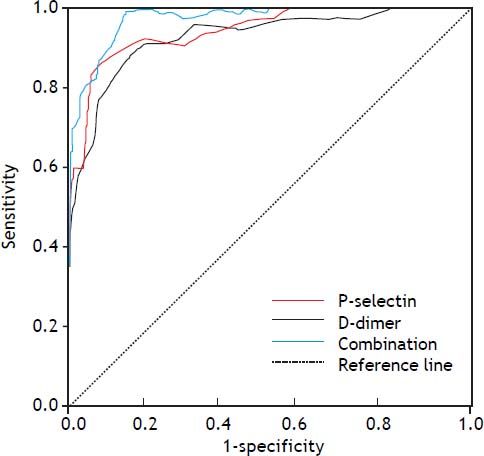
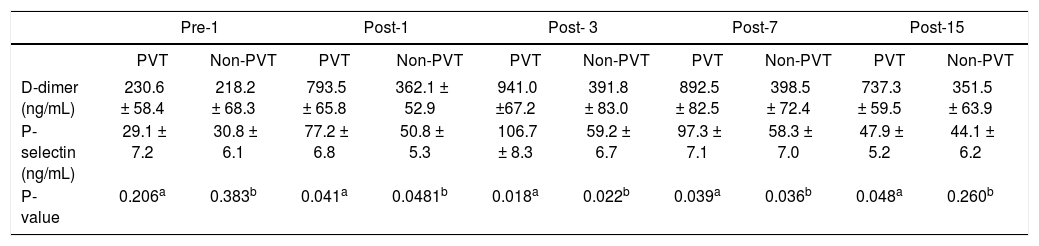
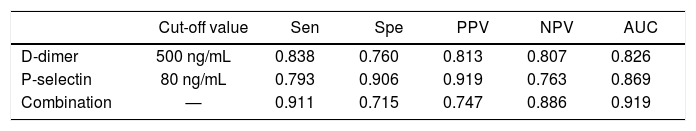
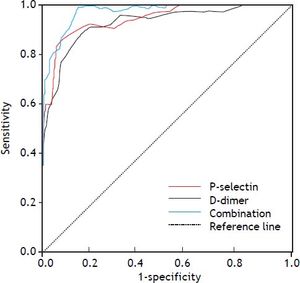
Results. 38 patients (27.7%) were found PVT by DU examination post-operatively. In contrast to the non-PVT group, the level of D-dimer and P-selectin in the PVT group was much higher significantly at 1, 3 and 7 days after devascularization (P < 0.05). However, in the 15 days after surgery, the difference of P-selectin between the two groups was not significant (P = 0.260). It was shown that the higher sensitivity of the two markers for PVT was D-dimer, the higher specificity belonged to P-selectin. The area under receiver operating characteristic (ROC) curve of P-selectin was the bigger of the two markers. When the two markers were combined to be used to diagnose PVT, the sensitivity was increased to 0.911, with a slight drop of specificity to 0.715, the area under ROC curve was 0.919.
Conclusion. The level of D-dimer and P-selectin might be good candidate predictive markers for PVT in patients with cirrhotic PHT after devascularization. The combined test of the two markers can increase the value of prediction.
Portal vein thrombosis (PVT) includes thrombosis in the portal vein, splenic vein and superior mesenteric vein or intrahepatic portal vein branches as they form an interactive vascular system without valves. PVT following devascularization occurs in 6.3 to 39.0% of patients and is mostly an unpredictable event.1,2 Complete or partial occlusion of the portal venous system in cirrhotic portal hypertension (PHT) patients may determine liver ischemia, with consequent deterioration of liver function, and a sudden increase in portal pressure. Some complications of liver cirrhosis such as variceal hemorrhage may develop and death eventually may occur.3–5 It is therefore important to identify markers that can predict and prevent the occurrence of PVT.
D-dimer is a kind of fibrin degradation fragment, and is the molecular marker in the fibrinolysis cycle.7 P-selectin is a cell adhesion molecule that is mainly produced by platelets and endothelial cells; it increases the activation of platelets and the adhesion of platelets to the endothelium.8 Recently, D-dimer and P-selectin have been shown to play an important role in diagnostic indicator for thrombotic diseases.9,10 In this study, we investigated whether D-dimer and P-selectin had a better predictive value to PVT after devascularization in patients with cirrhotic PHT.
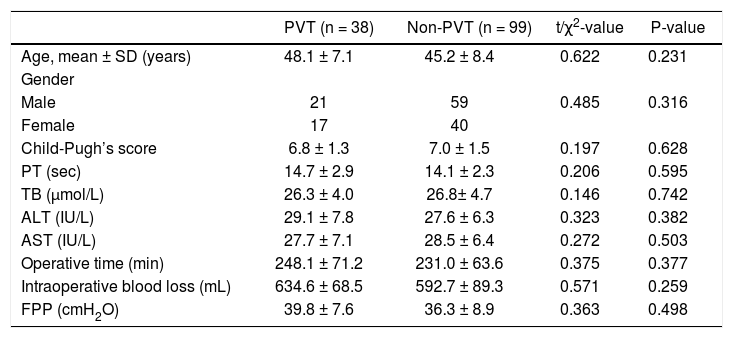
Material and MethodsPatients and study designTwo hundred sixty-seven consecutive patients who were diagnosed with hepatitis virus-related cirrhosis PHT between January 2012 to April 2014 in the 81st Hospital of PLA were included. The diagnoses of these patients were all confirmed by endoscopy and Doppler ultrasonography (DU). All of them underwent the surgery procedure. They accompanied with no serious cardiopulmonary diseases and concomitant chronic duodenal ulcers. Patients whose serum levels of D-dimer or P-selectin during the time of diagnosis and treatment were not available were excluded. Any patients who had been taking warfarin or Aspirin would have also been excluded. Accordingly, one hundred and thirty-seven patients were enrolled into this study, which was approved by our hospital. The characteristics of the patients including age, gender, Child-Pugh’s score, preoperative biochemical tests were summarized in table 1. Biochemical tests were examined within 1-3 days preoperatively.
Preoperative clinical characteristics of cirrhotic patients.
| PVT (n = 38) | Non-PVT (n = 99) | t/χ2-value | P-value | |
|---|---|---|---|---|
| Age, mean ± SD (years) | 48.1 ± 7.1 | 45.2 ± 8.4 | 0.622 | 0.231 |
| Gender | ||||
| Male | 21 | 59 | 0.485 | 0.316 |
| Female | 17 | 40 | ||
| Child-Pugh’s score | 6.8 ± 1.3 | 7.0 ± 1.5 | 0.197 | 0.628 |
| PT (sec) | 14.7 ± 2.9 | 14.1 ± 2.3 | 0.206 | 0.595 |
| TB (µmol/L) | 26.3 ± 4.0 | 26.8± 4.7 | 0.146 | 0.742 |
| ALT (IU/L) | 29.1 ± 7.8 | 27.6 ± 6.3 | 0.323 | 0.382 |
| AST (IU/L) | 27.7 ± 7.1 | 28.5 ± 6.4 | 0.272 | 0.503 |
| Operative time (min) | 248.1 ± 71.2 | 231.0 ± 63.6 | 0.375 | 0.377 |
| Intraoperative blood loss (mL) | 634.6 ± 68.5 | 592.7 ± 89.3 | 0.571 | 0.259 |
| FPP (cmH2O) | 39.8 ± 7.6 | 36.3 ± 8.9 | 0.363 | 0.498 |
PVT: portal venous thrombosis. PT: prothrombin time. TB: total bilirubin. Alb: albumin. ALT: alanine aminotransferase. AST: aspartate aminotransferase. FPP: free portal pressure.
The study protocol conformed to the guidelines by the institutional Ethical Committee. All patients gave their informed consent to be included in the study. The research was carried out according to the principles of The Declaration of Helsinki.
PVT diagnosisDU (ACUSÓN SequoiaTM 512, Color Doppler equipment) examination of the portal vein was performed pre-/post-operationally,11 and was performed in all cases by the same examiner to avoid interobserver variables. Spectral waveforms were obtained at measured angles of insonation of < 60°. The pre-operational examination was performed at three days before the surgery. The post-operational examination was performed at two, five, seven, fifteen, twenty-two and thirty days following the surgery. PVT was defined as the obstruction of more than 50% of the vascular lumen by a thrombus in the main portal vein, its large branches, or in the splenic vein. No patients had a diagnosed PVT prior to the operation. Then the samples were divided into two groups, including PVT group and non-PVT group.
D-dimer and P-selectin determinationsPeripheral venous blood sample (15 mL) was collected from each patient who had fasted for at least 12 h and mixed with 3.8% sodium citrate (ratio 9:1). Sample was centrifuged for 10 min at 2,000 g, and the supernatant was stored at -80°C until use. D-dimer and P-selectin were measured by automated latex enhanced immunoassay in citrated plasma on instrumentation Laboratory (Coagulation Systems ACL 9000) and quantified using enzyme linked immunosorbent assay kits (ZhongShan Biotech, Beijing, China). Both of the two biomarkers were tested one day before surgery, the second test was performed in one day postoperationally. Thereafter, in three days, seven days and fifteen days after surgery, the test was performed again.
Surgical techniqueThe surgical technique was applied as described by Zong, et al.12 The same operative setup and standardized technique were applied for all patients. Procedures were performed by the same team of specialists in gastrointestinal and hepatobiliary surgery.
Statistical analysisAll statistical analyses were performed using SPSS15.0 software (SPSS, Chicago, IL). Continuous data were expressed as mean values ± standard deviation (SD). Significant differences between groups were determined by chi-squared analysis and unpaired Student’s t test. Dichotomous variables were created out of continuous variables by using clinically important cutoff points. Receiver operating characteristic (ROC) curves, sensitivity (Sen), specificity (Spe), and positive and negative predictive values (PPV, NPV) were determined to assess the diagnostic value of D-dimer and P-selectin. P-values < 0.05 were considered statistically significant.
ResultsBaseline characteristicsDU examination showed thirty-eight patients developed PVT post-operatively (38/137, 27.7%), the occurrence of PVT was in 5.72 ± 1.73 days after devascularization, moreover, 86.8% PVT (33/ 38) occurred between day three and seven post-operationally.
There were no significant difference between the PVT group and the non-PVT group of the preoperative database including age, gender, Child-Pugh’s score, blood routine biochemical tests, mean operative time, intra-operative blood loss and intra-operative freedom portal vein pressure. The database also including the level of D-dimer and P-selectin (P > 0.05) (Table 2). The two groups were well balanced in the distribution of pre- and intraoperational characteristics.
The level of D-dimerand P-selectin pre/post-operation.
| Pre-1 | Post-1 | Post- 3 | Post-7 | Post-15 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PVT | Non-PVT | PVT | Non-PVT | PVT | Non-PVT | PVT | Non-PVT | PVT | Non-PVT | |
| D-dimer (ng/mL) | 230.6 ± 58.4 | 218.2 ± 68.3 | 793.5 ± 65.8 | 362.1 ± 52.9 | 941.0 ±67.2 | 391.8 ± 83.0 | 892.5 ± 82.5 | 398.5 ± 72.4 | 737.3 ± 59.5 | 351.5 ± 63.9 |
| P-selectin (ng/mL) | 29.1 ± 7.2 | 30.8 ± 6.1 | 77.2 ± 6.8 | 50.8 ± 5.3 | 106.7 ± 8.3 | 59.2 ± 6.7 | 97.3 ± 7.1 | 58.3 ± 7.0 | 47.9 ± 5.2 | 44.1 ± 6.2 |
| P-value | 0.206a | 0.383b | 0.041a | 0.0481b | 0.018a | 0.022b | 0.039a | 0.036b | 0.048a | 0.260b |
PVT: portal venous thrombosis. Pre: preoperation. Post: postoperation.
As shown in table 2, in contrast to the non-PVT group, the level of D-dimer in the PVT group was much higher significantly in one day, three days, one week and fifteen days after devascularization (P < 0.05). The similar situation could be found in the level of P-selectin. The significantly more altered was in the PVT group than in the non-PVT group postoperationally (P < 0.05). However, in the fifteen days after surgery, the difference of P-selectin between the two groups was not significant (P = 0.260).
Value of D-dimer and P-selectin on PVTBy using the change in D-dimer level and P-selectin level as the diagnostic standard for PVT in cirrhosis patients after devascularization, we achieved the Sen, Spe, PPV and NPV in predicting incidence of PVT (Table 3). It showed that the higher Sen of the two markers for PVT was D-dimer, the higher Spe belonged to P-selectin. Based on the different changes in D-dimer, P-selectin levels and the false positive rates and Sen rates in different D-dimer, P-selectin levels, a ROC curve was plotted. Using the ROC analysis, the area under the ROC curve were 0.826 and 0.869, respectively. When the two markers were combined to diagnose PVT, the Sen was increased to 0.911, with a slight drop of Spe to 0.715, the area under the ROC curve was 0.919 (Figure 1).
Evaluation the value for PVT of D-dimer and P-selectin.
| Cut-off value | Sen | Spe | PPV | NPV | AUC | |
|---|---|---|---|---|---|---|
| D-dimer | 500 ng/mL | 0.838 | 0.760 | 0.813 | 0.807 | 0.826 |
| P-selectin | 80 ng/mL | 0.793 | 0.906 | 0.919 | 0.763 | 0.869 |
| Combination | — | 0.911 | 0.715 | 0.747 | 0.886 | 0.919 |
Sen: sensitivity. Spe: specificity. PPV: positive predictive value. NPV: negative predictive value. AUC: area under the receiver operating characteristics curve. Combination, combined D-dimer, P-selection and platelet count.
The prevalence of PVT in cirrhotic PHT had been reported as values ranging from 0.6 to 2.1%.13 However, PVT has been recognized as a potential complication following devascularization for PHT, some literatures showed a frequency from 6.3 to 39.0%.1,2 In our study, the incidence of PVT after devascularization was 8.6%. PVT is often an occasional diagnosis in asymptomatic patients, but it may rapidly progress leading to massive thrombosis of intestinal veins, even fatal consequences.14 Therefore, early diagnosis of PVT may be useful to prevent uneventful outcome. The early predictive indicator of postoperative PVT may be the most focus.
At present, some methods were performed to prevent the occurrence of PVT.
- •
Systemic or topical injection heparin for prophylaxis intraoperatively or immediate postoperatively.15 But not all patients may occur PVT or accept the treatment of injection heparin.
- •
Anticoagulant therapy base on the testing platelet count, since this method reflects only the number of platelets, ignores the function of platelet count. Some reports showed that the level of platelet count was not more than the level of 500 x 109/L until portal vein thrombosis formation.16
- •
Imaging examination especially DU can provide information on the thromboses via echo analysis, detect the presence of post-stenotic dilatation, as well as flow defects and turbulence.
Although PVT can be accurately diagnosed by DU, the formation of thrombosis was a dynamic process, only when the appearance of PVT, the ultrasound can play a valuable role, so it can’t predict thrombosis.
D-dimer is a small peptide fragments of early thrombosis in the role of fibrinogen degradation of plasmin formation, the presence of secondary fiber in vivo dissolved and specific marker of thrombosis.17 Risch thought that D-dimer could be used as a diagnostic specificity of acute deep vein thrombosis indicators.18 Palareti found the change of D-dimer level after anticoagulation therapy for patients may predict the risk of thrombosis recurrence.19 In recent years, some studies have shown that D-dimer level as sensitive indicator for coagulation system and fibrinolytic system could predict the formation of PVT.20 Our study showed that the specificity of D-dimer was 77.3% in predicting PVT incidence, the sensitivity was 84.6%, and it may be regarded as a stable and good indicator. Increased D-dimer after operation suggested that activation of coagulation in vivo and hepatic clearance of tissue plasminogen activator were related to the reduction of fibrinolysis inhibitor protein synthesis.
The study on deep venous thrombosis showed that P-selectin involved in platelet/endothelial cell adhesion and inflammation in vascular wall, which may lead to a new pathogenesis of venous thrombosis.21 Blenn, et al. found that soluble P-selectin level in patients with deep vein thrombosis was significantly higher, which may be related to excessive platelet activation.22 Myers’s experiment showed that P-selectin could enlarge the effect of vein wall inflammation caused by thrombotic stimuli and promoting venous thrombosis. The higher level P-selectin, the more inflammatory cells in vein wall, the bigger intravenous clot generated simultaneously in model mice.23 Therefore, as an indicator of the degree or function of platelet activation, P-selectin can be regarded as a marker to evaluate the prothrombotic state, coagulation tendency and formation of thrombosis in vivo. Our study showed that compared with non-PVT group, the level of P-selectin was higher in PVT group post-operationally, especially in three days after surgery. When 80 ng/mL was set as a cut-off point, P-selectin had an 87% sensitivity and specificity for PVT.
As a dynamic process, the formation of thrombosis was monitored by our DU continuously. And the two indicators including D-dimer and P-selectin were tested continuously for assessing the predictive ability. DU examination showed the occurrence of PVT was 5.72 ± 1.73 days (2-7 days) after devascularization. The two indicators showed significant difference between PVT group and non-PVT group in one, three and seven days after operation (P < 0.05), however the differences could not be found in the fifteen days post-operatively. By this token, the best prediction PVT critical point should be set as early as possible, and should be lasted three days at least. From the ROC curve figure, the area under curve of P-selectin was the bigger. When the two indicators were combined together, the area may be up to 0.919, the value of early prediction can be improved. Then clinical interventions can be performed in time and safely.
ConclusionThe level of D-dimer and P-selectin might be good candidate predictive markers for PVT in patients with cirrhotic PHT after devascularization. The combined test of the two markers can increase the value of prediction.
Abbreviations- •
DU: Doppler ultrasonography.
- •
NPV: negative predictive values.
- •
PHT: portal hypertension.
- •
PPV: positive predictive values.
- •
PVT: portal vein thrombosis.
- •
ROC: receiver operating characteristic.
The authors declare no conflict of interest.