Background. Italy has recently become a land of immigration. Two hundred and fifty thousand carriers are immigrants and chronic HBV infection is the prevalent form. Considering the elevated number of foreigners resident in our province and the potential risk of transmission to local people, we retrospectively investigated the patterns of chronic hepatitis B (CHB) in 154 patients (76 foreigners, 78 Italians) observed in our Institution, with regard to demographic and clinical/laboratory characteristics.
Results. The immigrants were younger (mean age 31 years) compared to Italians (51.5) and mainly came from East Europe. Regarding exposure to HBV, the intra-familial risk factor was most frequently observed in foreigners, compared to Italians (p = 0.03). Foreigners also showed a higher prevalence of HBeAg positive forms, HDV co-infection (7.9%) and abnormal ALT and/or HBV-DNA values, compared to Italians. HBeAg positivity was more associated with increased ALT (OR = 36.6, p = 0.001) than with elevated HBV viremia (OR = 6.5, p = 0.049); age was a protective factor (OR = 0.1; p = 0.014). No significant association was found between increased ALT and foreign nationality. The simultaneous presence of increased ALT and viremia was more frequent among foreigners, (OR = 7.6, p = 0,014) and increased with age (OR = 1.06, p = 0.013). Antiviral therapy was given in 7.8% of foreign citizens.
Conclusion. Immigrants constitute a vulnerable population subgroup that would benefit from a more active approach regarding doctor-patient relationship for early recognition of HBV and treatment programmes.
The epidemiology of hepatitis B in Italy has undergone significant changes over the past 25 years.1 During the decade 1970-1980, Italy was a medium level endemic country, with wide geographical variations in prevalence of chronic carriers of HBsAg (the prevalence in the general population was equal to 2-8% with the highest levels found in southern areas and the islands). Intra-familial transmission was the most common mode of virus spread, the majority of chronic carriers were HBeAg positive, a high percentage of subjects with chronic liver disease were HBsAg positive, and infection by virus Delta was frequently found.
After thirty years, the picture has completely changed: Italy is a country with low endemicity (the percentage of chronic carriers in the general population is probably less than 1%); geographic variations in the prevalence of chronic carriers no longer exist; sexual transmission is the most common mode of infection acquisition; most chronic carriers are anti-HBeAg positive. Finally, the introduction of increasingly effective serological (HBsAg) and bio molecular tests (Nucleic Acid Technology, HBV-NAT) for the identification of risk donors has made the HBV transmission by transfusion a rare event in our country.
The question is whether people coming from endemic areas for HBV can change the epidemiological future of our country.
In migrant populations viral hepatitis is the third most infectious disease observed, CHB being the prevalent form. Of the six hundred thousand carriers of the virus in Italy, two hundred and fifty thousand are immigrants.2-3 An increasing number of patients come from countries in Eastern Europe (EU), Asia, North and Sub-Saharan Africa, where the HBsAg-positive prevalence is intermediate/high due to a lack of vaccination campaigns, poor health conditions and life-threatening habits.4 Despite the continuous immigration of subjects from endemic countries, a recent study found overall prevalence of HBV infection unchanged.5 However, as immigration from non-EU countries continues to grow, the integration of HBsAg positive immigrants into the local social context might lead to the spread of HBV infection among the unvaccinated resident population, increasing the number of new adult infections through risky life-style habits (i.e. promiscuous sexual contacts, drug addiction, etc.) or professional accident (i.e. needle prick in non-immune health care workers) that in some way can contribute to changing the epidemiology of HBV infection in Italy.
In Ferrara, a city in the north of Italy, there are 22,000 prevalently young resident foreigners, most of whom come from Morocco, Romania, Albania, Ukraine, Moldavia and Pakistan, all areas considered to be intermediate-high endemic for HBV infection.6
Early diagnosis in these populations is very important either to prevent serious complications such as cirrhosis and hepatocellular carcinoma to the health of patients, or to reduce the spread of infection in the general population.
Considering that immigrants often present demographic, clinical and virological characteristics different from those of Italian patients and expecting a change in the scenario of HBV-related disease in our area, we carried out a retrospective analysis of the demographic and clinical/laboratory characteristics of chronic HBV infection in migrant patients observed in our Institution from 1997 to 2009, which we then compared with Italian patients.
Material and MethodsEpidemiologic surveyWe studied a total of 154 patients, including 76 foreigners (45 M, 31 F), and 78 Italians (54 M, 24 F) as either outpatients or inpatients observed at Program of Infectious, Tropical and Migrant’s Diseases of University of Ferrara from 1997 to 2009. After a medical check-up, all subjects consecutively enrolled gave their informed consent to join the study and were interviewed by a member of the medical staff in accordance with Italian law on privacy. All patients were given a questionnaire regarding information on demographic data, risk factors for acquiring HBV infection (in particular the presence of previous parenteral exposure and any medical history positive for acute hepatitis), and laboratory data other than the clinical condition (i.e. co-infections) at diagnosis. According to the source of exposure and before undertaking the statistical analysis, risk factors were grouped, based on current epidemiological concepts, into “classic” (blood transfusion/blood products, sex, history of intravenous drug abuse), “intra-familial” (mother to child perinatal transmission or belonging to a household of HBsAg-positive persons) and “inapparent” (tattoos, piercings, previous use of non-disposable syringes, dental care).
Informed consent in writing was obtained from each patient. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Laboratory examinationsThe laboratory data were hepatitis B serum markers (HBsAg, HBeAg, anti-HBe, HBV-DNA), HBV genotype and markers of any co-infection (HIV, HCV, HDV). HBsAg, HBeAg, anti-HBe and anti-HDV antibodies were determined by commercial immunoassays (Abbott Laboratories, Chicago, IL, USA). Quantitation of serum HBV DNA viral loads was assessed by the commercial COBAS TaqMan HBV test (CTM HBV test; Roche Diagnostics, Meylan, France) polymerase chain reaction (PCR) based on TaqMan PCR chemistry which uses three amplification primers and an internal quantitation standard (QS) (a non-infectious DNA construct, containing fragments of HBV sequences with primer binding regions identical to those of the HBV target sequence) according to Hochberger.7 The COBAS TaqMan Analyser calculates the HBV concentration in the test specimens by comparing the HBV signal to the HBV QS signal for each specimen and control (IU/ml). The viremia was considered significant if ≥ 2000 IU/mL for HBeAg-negative forms and ≥ 20,000 IU/mL for HBeAg positive forms. Serum alanine aminotransferase (ALT) were quantified by ultraviolet enzymatic-assay (normal range 0-40 IU/L). These were considered significantly increased if ≥ 2 times the normal value (20 IU/l for women and 30 IU/l for men). Antibodies to hepatitis C virus (anti-HCV) were detected by third-generation commercial immunoenzymatic assays.
For the determination of HBV genotypes (seventeen cases), HBV-DNA was extracted from 100 μL serum samples using the High Pure PCR Template Preparation kit (Boehringer Mannheim) essentially as described by Stuvyer.8 The extracted DNA was amplified over two rounds of nested PCR using biotinylated PCR primers according a previous described procedure.9 HBV genotypes were determined by the INNO-LiPA HBV Genotyping (Innogenetics NV, Gent, Belgium). The correct HBV genotype was determined by consulting an interpretation chart showing probe reactivity patterns for each HBV genotype. Chronic hepatitis was diagnosed by liver histology10 or, for patients without liver biopsy, on the basis of a persistent abnormality in ALT serum level and of an HBV-DNA titre > 2000 IU/mL for at least 6 months, in the absence of clinical, biochemical and ultrasound markers of liver cirrhosis.11
Liver cirrhosis was diagnosed by examination of a liver biopsy sample or by the presence of unequivocal clinical, biochemical, and ultrasound signs.12 Hepatocellular carcinoma diagnosis was based on histology, imaging techniques, or biochemical parameters (α1-feto protein level, 1,400 ng/mL).13
Statistical analysisThe demographic profile, medical history and laboratory data of the patients were described using proportions, means with standard deviation (or range if asymmetrical distribution), median with interquartile range (IQR), and compared using χ2 test or Mann-Whitney test or two-tail t-test as appropriate. In order to compare immigrants to Italian patients, we also evaluated possible associations between foreign nationality and specific risk factors such as HBeAg positivity as major disease activity and indication to treatment with antiviral drugs. Dichotomous data were included as independent variable (ethnicity) or dependent variables (risk factors, HbeAg positivity) in logistic regression models. The odds ratio (OR) described the strength of association whereas the confidence interval (C.I.) gave information on the certainty of estimates and the amount of unexplained variability. For OR estimates the reference category was considered the Italian patients. A significance threshold of p < 0.05 was accepted. Analyses were performed using STATA software, release 11.0 (Stata Corp. College Station, Tex., USA).
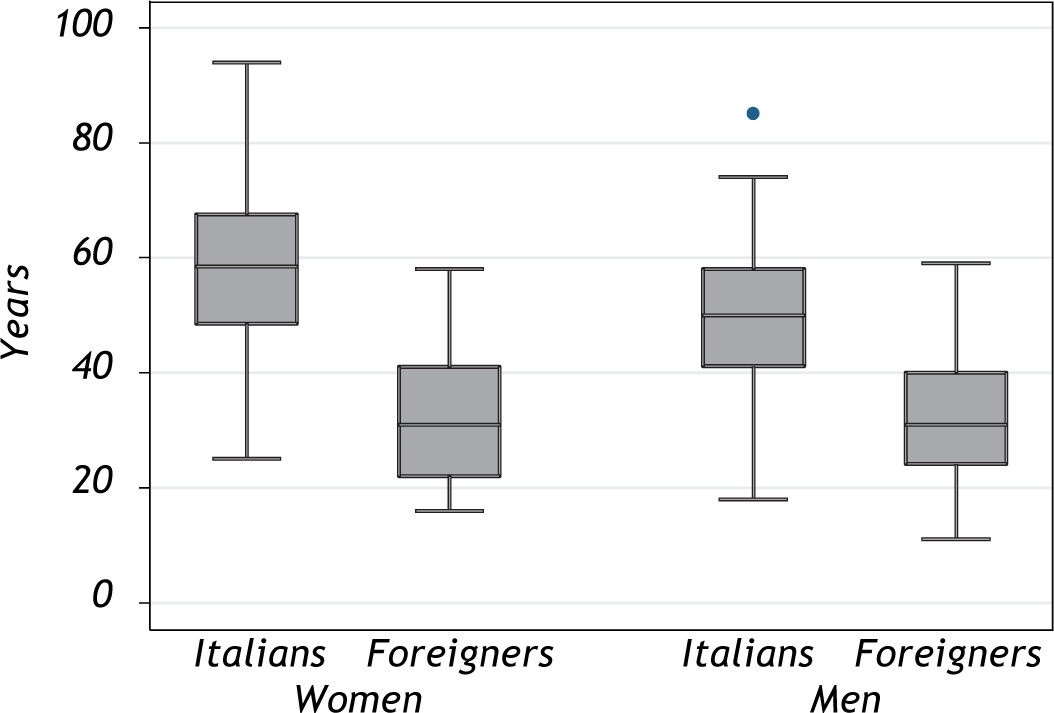
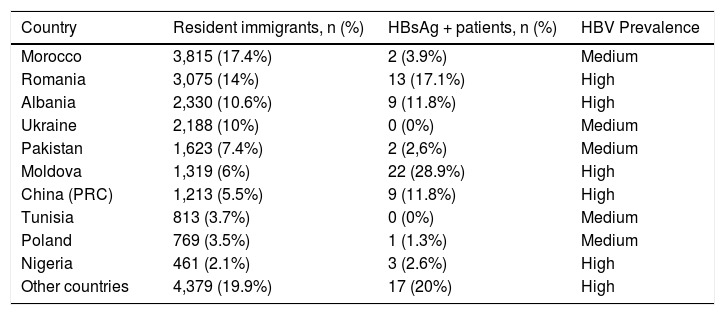
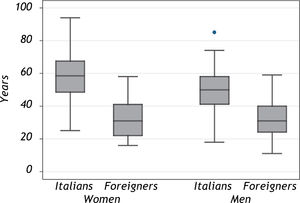
ResultsEpidemiologyWhole data on the geographical origin of immigrants, the number of HBsAg positive patients and the mean age distribution of all patients, by country and gender are shown in table 1 and figure 1.
Origin of immigrants living in Ferrara and HBsAg-positive patients investigated.
| Country | Resident immigrants, n (%) | HBsAg + patients, n (%) | HBV Prevalence |
|---|---|---|---|
| Morocco | 3,815 (17.4%) | 2 (3.9%) | Medium |
| Romania | 3,075 (14%) | 13 (17.1%) | High |
| Albania | 2,330 (10.6%) | 9 (11.8%) | High |
| Ukraine | 2,188 (10%) | 0 (0%) | Medium |
| Pakistan | 1,623 (7.4%) | 2 (2,6%) | Medium |
| Moldova | 1,319 (6%) | 22 (28.9%) | High |
| China (PRC) | 1,213 (5.5%) | 9 (11.8%) | High |
| Tunisia | 813 (3.7%) | 0 (0%) | Medium |
| Poland | 769 (3.5%) | 1 (1.3%) | Medium |
| Nigeria | 461 (2.1%) | 3 (2.6%) | High |
| Other countries | 4,379 (19.9%) | 17 (20%) | High |
Patient’s age distribution by country and gender. Overall, there are no differences by age between total women (n = 55; mean value: 42.9 years) and total men (n = 99; mean value: 41.9). Mean age values are higher in Italian women (56.6 years) than in foreign women (32.2 years; p < 0.001) and also in Italian men (49.8 years) than in foreign men (32.2 years; p < 0.001). The box represents the 25th-75th quartile divided by median, the whiskers represent the range. The dot is an outlier (Italian men).
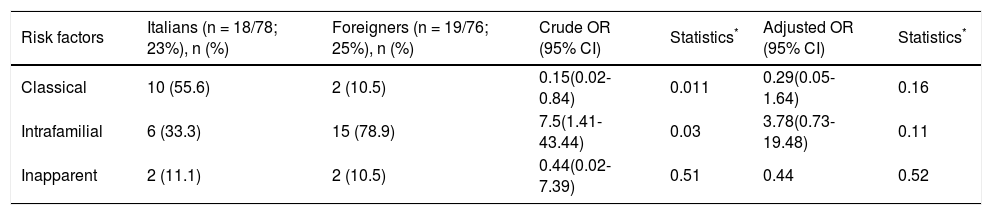
The countries of origin most represented were Morocco, Romania, Albania, Ukraine, Pakistan and Moldova, while the majority of HBsAg positive patients were from Moldova, Romania, China and Albania. People from these countries come to Italy principally for jobs as carers of the elderly. The median age of foreign patients was 31 years (range 11-59), compared to Italian patients which was significantly higher (median 51.5, range 18-94). Table 2 summarizes the association of risk factors for HBV infection in the cohort of patients examined. Risk factors were documented in 23% of Italian patients (18/78) compared to 25% of foreign patients (19/76). The classical factors were present in a significantly lower rate in the medical history of foreign patients than Italians (crude OR = 0.15, p = 0,011). The presence of the intrafamilial factor was instead more frequently associated with foreign citizens than with Italians (p = 0.03). When adjusted with age, the association of this risk factor with nationality was lower (family factor: OR = 3, 8; p = 0.11; classical factors: OR = 0, 29; p = 0.16). For the inapparent factors, the small sample size studied did not allow us to report any significant data (OR = 0.44; p = 0.52).
Distribution of risk factors for HBV infection. Estimated crude OR by univariate analysis (Foreigners vs. Italians) and adjusted estimated OR by model with age.
| Risk factors | Italians (n = 18/78; 23%), n (%) | Foreigners (n = 19/76; 25%), n (%) | Crude OR (95% CI) | Statistics* | Adjusted OR (95% CI) | Statistics* |
|---|---|---|---|---|---|---|
| Classical | 10 (55.6) | 2 (10.5) | 0.15(0.02-0.84) | 0.011 | 0.29(0.05-1.64) | 0.16 |
| Intrafamilial | 6 (33.3) | 15 (78.9) | 7.5(1.41-43.44) | 0.03 | 3.78(0.73-19.48) | 0.11 |
| Inapparent | 2 (11.1) | 2 (10.5) | 0.44(0.02-7.39) | 0.51 | 0.44 | 0.52 |
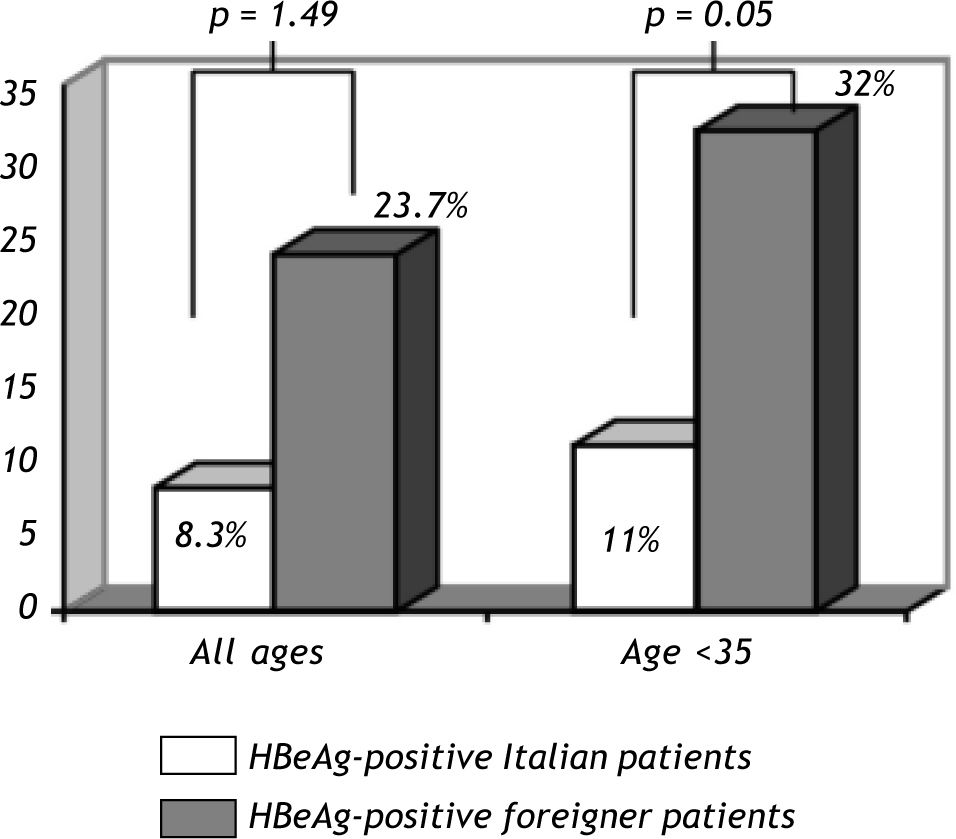
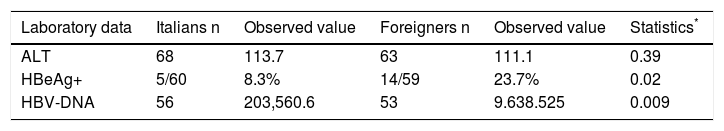
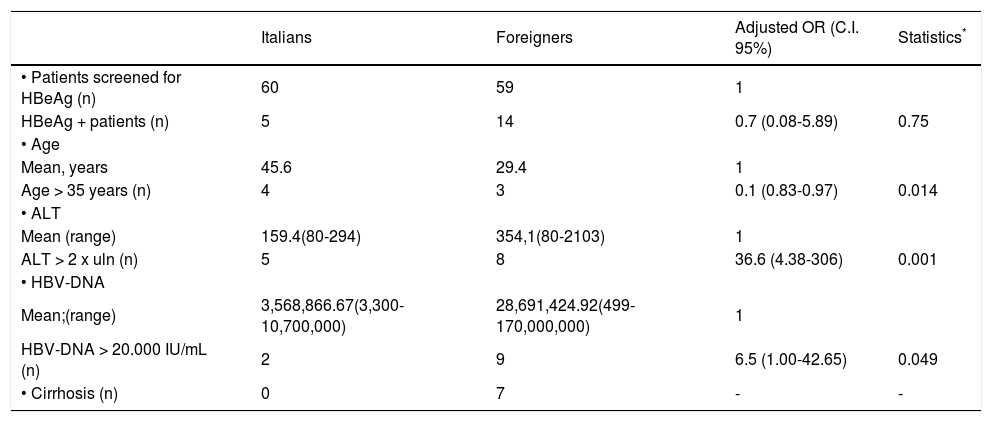
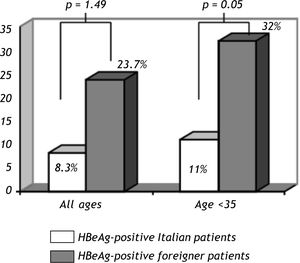
The main results of laboratory investigations are summarized in table 3. There was no significant association between increased ALT and foreign nationality (p = 0.39). The percentage of HBeAg forms was significantly higher in foreigners compared to Italians (23.7% vs. 8.3%; p = 0.02); moreover, HBV viremia was significantly more frequently elevated in foreigners than Italians (p = 0.009). When adjusted with age, the simultaneous presence of increased ALT and viremia was also significantly more elevated among foreigners (OR = 7.6; p = 0,014). In table 4 are shown the principal HBeAg positive patient’s characteristics according to age, ALT and viremia. In the multivariate model, adjusted with age, viremia and ALT levels, nationality was no longer a discriminating factor (p = 0.75). A stronger association was found between HBeAg positivity and elevated ALT (OR = 36.6; p = 0.001) compared to that observed between HBeAg and elevated viremia (OR = 6.5; p = 0.049). In our data, the age was a protective factor (OR = 0.1; p = 0.014). In general, ALT and HBV viremia showed significantly higher mean values among foreigners compared to Italians. Figure 2 shows the age distribution of HBeAg positive patients in relation to nationality. Foreigners under 35 years (32%) were more frequently associated to HBeAg positive forms compared to Italians (11%); p = 0.012.
Main laboratory characteristics of all patients examined.
| Laboratory data | Italians n | Observed value | Foreigners n | Observed value | Statistics* |
|---|---|---|---|---|---|
| ALT | 68 | 113.7 | 63 | 111.1 | 0.39 |
| HBeAg+ | 5/60 | 8.3% | 14/59 | 23.7% | 0.02 |
| HBV-DNA | 56 | 203,560.6 | 53 | 9.638.525 | 0.009 |
Characteristics of HBeAg + patients. Estimated OR adjusted by model with the other variables examined (except cirrhosis, not included in model).
| Italians | Foreigners | Adjusted OR (C.I. 95%) | Statistics* | |
|---|---|---|---|---|
| • Patients screened for HBeAg (n) | 60 | 59 | 1 | |
| HBeAg + patients (n) | 5 | 14 | 0.7 (0.08-5.89) | 0.75 |
| • Age | ||||
| Mean, years | 45.6 | 29.4 | 1 | |
| Age > 35 years (n) | 4 | 3 | 0.1 (0.83-0.97) | 0.014 |
| • ALT | ||||
| Mean (range) | 159.4(80-294) | 354,1(80-2103) | 1 | |
| ALT > 2 x uln (n) | 5 | 8 | 36.6 (4.38-306) | 0.001 |
| • HBV-DNA | ||||
| Mean;(range) | 3,568,866.67(3,300-10,700,000) | 28,691,424.92(499-170,000,000) | 1 | |
| HBV-DNA > 20.000 IU/mL (n) | 2 | 9 | 6.5 (1.00-42.65) | 0.049 |
| • Cirrhosis (n) | 0 | 7 | - | - |
Age distribution of HBeAg+ Italian and foreign patients. The bars indicate the ratio of HBeAg+ patients with respect to the total number for each category. Considering all ages, the differences between HBeAg+ Italian and foreign patients are not statistically significant (p = 0.49). In the younger age (< 35 years), HBeAg + forms are more frequent among foreigners than Italians (p = 0.012).
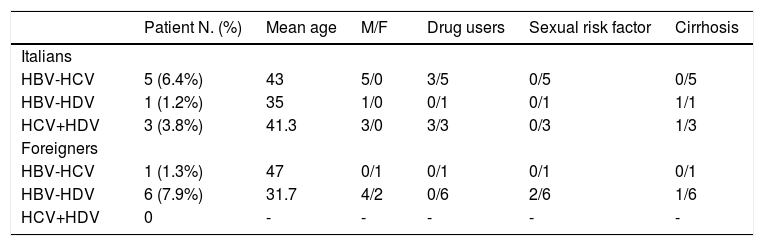
Regarding coinfections, a higher prevalence of HDV co-infection was found in 6 foreigners (7.9%), compared to Italian patients (Table 5). This was related to unsafe sexual intercourse (2 cases) and was associated to cirrhosis in one case (16.6%). Among the most common co-infections found in Italian patients, HCV was present in 5 (6.4%) cases, HDV in one (1.2%), HCV and HDV in three (3.8%).
Rate of HBV coinfection in Italian and foreign patients.
| Patient N. (%) | Mean age | M/F | Drug users | Sexual risk factor | Cirrhosis | |
|---|---|---|---|---|---|---|
| Italians | ||||||
| HBV-HCV | 5 (6.4%) | 43 | 5/0 | 3/5 | 0/5 | 0/5 |
| HBV-HDV | 1 (1.2%) | 35 | 1/0 | 0/1 | 0/1 | 1/1 |
| HCV+HDV | 3 (3.8%) | 41.3 | 3/0 | 3/3 | 0/3 | 1/3 |
| Foreigners | ||||||
| HBV-HCV | 1 (1.3%) | 47 | 0/1 | 0/1 | 0/1 | 0/1 |
| HBV-HDV | 6 (7.9%) | 31.7 | 4/2 | 0/6 | 2/6 | 1/6 |
| HCV+HDV | 0 | - | - | - | - | - |
The genotype was determined in 17 patients (one Italian, sixteen foreigners) with virological activity of infection (detectable serum HBV-DNA). Of these, 15 had non-D genotype (2 E, 10 C, 3 A), 4 of whom with HBeAg-positivity and HBV-DNA > 110 million IU/mL.
Antiviral therapy was given in 16 patients only (10.3%) of whom 6 were foreigners (7.8%, median age, 41 years). This consisted, in three cases, of pegylated interferon (Peg-IFN) or nucleos(t)ide analogues (NUCs): telbivudine (one), entecavir plus tenofovir (one) tenofovir (one). Two foreign patients were unable to undergo any follow-up because they migrated to another country.
ConclusionsItaly is one of the European countries with the largest number of immigrants coming from endemic areas for infectious diseases, including HBV and HCV hepatitis.3,14-15 Considering the elevated number of foreigners resident in our province and the potential risk of transmission to local people, we sought to investigate some peculiar epidemiologic, clinical and laboratory features of immigrants with CHB that make this population worthy of attention.
Firstly, most foreign residents in our province come from Eastern EU countries, sub-Saharan Africa and Asia considered to be areas at medium-high risk endemicity for HBV infection, and have lived in Italy for less than 2 years. In our series there were not ethnic groups such as Ukrainians and Tunisians, who, although present in significant numbers in the territory of Ferrara, probably have very little or no knowledge of transmission of HBV infection and its complications. This lack underlines the need to target certain groups in future information campaigns, screening programmes and vaccination.
Secondly, analysis of risk factors identified in the medical history of foreigners showed that the intrafamilial factor was more frequent and statistically significant compared to the expected classic sexual and parenteral (including intravenous drug use) mode of HBV transmission of patients from Eastern EU and North Africa and also in part identified in Italian patients especially those ≥ 42 years, but not in Chinese people, in whom the main transmission route of HBV is mainly vertical and the secondary way is by blood products. These different modes of transmission could have affected the clinical, serological and virological profile found in foreigners compared to Italians and likely related other to environmental and host factors, also to predominant genotype which can in some way contribute to the change or duration of the natural history of CHB infection.15-16
Thirdly, our study highlighted that HBV infection among immigrants in Ferrara occurred early in their lives, in general accordance with the lowest average age of the foreign population, as previously reported.17-18 The occurrence of this infection in foreign younger people supports the observation of a consistent and significant higher number of HBeAg-positive forms in immigrants as compared to the Italian people, reflecting an earlier stage of infection and hence a long history of persistently high viral replication and progressive liver injury.19 Our preliminary data did not allow us to determine whether or not these forms were associated except in a few cases, with advanced liver disease. This is a limitation of our study. However, a recent Italian multicenter study found no significant differences regarding the progression of disease among HBsAg-positive Italians and immigrants.2 Another limit of our study was the limited number of foreigners recruited. This was in part because of lack of compliance to diagnosis and treatment. In particular, among these, we have had more difficulty in testing or re-testing women, since, as it is known, in African communities, they are afraid to know their eventual disease especially infectious diseases that can be a social discriminating factor.18
Fourthly, foreigner patients also showed either a higher prevalence of ALT or serum HBV-DNA values significantly more often above the limit value, compared to Italian patients. This finding is extremely important since these patients could be recruited in a health care programme aimed at antiviral therapy, which in our series was administered in few cases and initiated later compared to Italians. This was mainly because of lack of compliance of immigrants to regular treatment compared to Italians. Cultural and linguistic barriers, lack of a stable job or fear of therapy side effects have led in general to a lower adherence to medical recommendations, especially in immigrants from sub-Saharan Africa and China, compared to those fro Eastern EU, including medical checks required during the pre-assessment treatment. In general, the combination of these factors reduced the number of antiviral treatments, when compared with the native Italian population.
In this context, although the criteria of choice between interferon and NUC were those suggested by the international guidelines,20 young migrants, especially those from Eastern EU, who are well-integrated into the local society, without hepatic decompensation and reluctant to commit a long duration with treatment, were more willing to undertake treatment with INF-therapy. Older migrants such as some African or Chinese people with contraindications to IFN, and willing to commit to long durations of treatment, underwent NUC administration as the initial therapy. Follow-up data would be desirable fro these patients to increase the strength of our study.
Regarding co-infections, these were mainly associated with HDV and were found in 7.9% non intravenous young foreign drug users and HIV-negative compared to Italians. This rate agrees with other recent Italian results which found that non-EU patients are significantly younger and have a higher prevalence of HBeAg-positive infection and HDV co-infection than patients of Italian origin.21 The circulation of the virus delta in Italy has decreased exponentially in the last ten years. The relatively recent HDV infections migrating to Europe now represent a pool which is refreshing the circulation of HDV in proportion to the local number of migrants from endemic areas. HDV infection is now more prevalent in the older HBsAg carriers with liver diseases than in younger people.22 In young age, HDV infections are still found in co-infected subjects with HIV, whose risk factor is the use of drugs by vein. Unprotected sexual practices are possibly the main cause of re-emergence of HDV in our patient population.
Finally, regarding the HBV genotypes, in our series the non-D HBV genotype was found in the majority of patients. In particular, of the 10 patients with genotype C (present in Asia only), nine were from China and Belarus, one was from Italy; three patients with genotype A (widely distributed in Northwest Europe, North America and Central Africa) came from Moldova and Cameroon, while one patient with genotype E (prevalently found in sub-Saharan Africa) was from Niger. Three patients with D genotype (found worldwide with overall predominance in the Mediterranean area) were, as expected, from Italy, where most acute and chronic HBV patients (about 95%) present genotype D.16,23 An indirect demonstration of the potential redistribution of HBV genotypes comes from the Italian patient with genotype C which is not diffused in our country, but in Asia only. This demonstrates how this genotype can be spread in the Italian population through sexual transmission.16
These findings underline the importance of careful monitoring of the diffusion of different genotypes in the immigrants infected by HBV especially among individuals from areas with strong migratory pressure and high endemicity, in particular Eastern EU, North and Sub Saharan Africa and China, as they may require a different clinical and therapeutic approach as compared to genotype D.16-17
In this setting, to successfully manage migrant patients with CHB is fundamental an extensive information campaign which ensures and facilitates the systematic access to the Italian Health System in order to optimize the screening of hepatitis markers aimed at preventing their spread and extending the lives of CHB-infected patients.
Migrants are in fact a vulnerable population subgroup in whom an implementation of strategies is required to improve either their adherence to diagnostic and therapeutic programmes (outpatient clinics providing intercultural mediation), or doctor awareness for a focused approach in the management of HBV infection in this population.
In this study, in fact, there was only about 25% of the immigrants at their first diagnosis of hepatitis B vs. 32% of Italians, suggesting that educational or screening programs are warranted to identify new HBV carriers. This is especially true for economically disadvantaged groups, such as illegal immigrants, with a low educational level and less awareness of their rights, who represent categories needing more attention.
Abbreviations- •
CHB: chronic hepatitis B.
- •
EU: Europe
- •
HBV: hepatitis B virus.
- •
HDV: hepatitis delta virus.
- •
Anti-HCV: antibodies to hepatitis C virus.
- •
OR: odds ratio.
- •
IQR: interquartile range.
- •
CI: confidence interval.
- •
Peg-IFN: pegylated interferon.
- •
NUCs: nucleos(t)ide analogues.
We thank Dr. Elisabeth Jenkins for her help with the manuscript.