Aim. Liver biopsy (LB) is often essential for the diagnosis and staging of chronic viral hepatitis. The aim of our paper was to establish if the size of the biopsy needle influences the number of portal tracts obtained through LB.
Material and methods. We conducted a retrospective study on 596 echoassisted percutaneous LBs performed in the Department of Gastroenterology and Hepatology Timisoara during a 4 years period. We included only those biopsy results that had mentioned both the type of needle and the number of portal tracts. All LBs were echoassisted and performed with Menghini modified needles 1.4 and 1.6 mm in diameter (technique with two passages into the liver). The liver fragments were analyzed by a senior pathologist and Knodell score was used to describe necroinflammatory activity as well as fibrosis. We compared the number of portal tracts obtained with 1.4 vs. 1.6 Menghini needles.
Results. Type 1.4 mm Menghini needles were used for 80 LBs, while 1.6 mm type were used in 516 LBs. Liver fragments obtained with 1.6 mm Menghini needles had a significantly higher mean number of portal tracts as compared to those obtained with 1.4 needles (24.5 ± 10.6 vs. 20.8 ± 8.6, p = 0.003).
Conclusion. The 1.6 mm Menghini needles provide better liver biopsy specimens, with higher number of portal tracts, as compared to 1.4 mm Menghini needles.
Liver biopsy (LB) is still considered as the gold standard method for the evaluation of hepatic involvement in chronic hepatitis, despite the fact that non-invasive methods (serological markers and elastographic methods) are used more and more in daily practice.
To remain the gold standard method, LB must be accurate enough in regard to the size and number of portal tracts of the tissue fragments. Liver samples 14 cm in length are obtained by LB (preferably at least 1.5 cm).1 Usually, a liver specimen is considered to be adequate for pathological exam if it is longer than 25 mm and if it includes more than 8 portal tracts2 or more than 11 portal tracts, in the opinion of other authors.3 Colloredo, et al.4 showed that the shorter the liver sample obtained by LB is, the greater is the chance to underestimate the severity of fibrosis and of necroinflammatory lesions. In a mathematical model created by Bedossa,5 an estimate bioptic liver fragment 25 mm long, can lead to an error rate of 25% and the optimal size of specimen is 40 mm.
Several studies showed that, in daily practice, the liver fragments obtained by LB are not long enough for a correct histological evaluation. A multicentre study performed in France showed that the median length of the fragment obtained by LB was 15 mm,6 and another French study6 showed that from 323 LB analyzed, 49 (15.2%) were considered as uninterpretable by the pathologist. In another study performed on 1,257 LB6, in 132 cases (10.5%), the fragments were considered uninterpretable by the pathologist. Thus, considering the estimation from the mathematical model of Bedossa and the reality from these French studies, the rate of diagnostic error can rise to 30-40% and this is unacceptable for a gold standard method.
The aim of our study was to establish if the size of the needle (1.4 vs. 1.6 mm) influences the number of portal tracts obtained through LB.
Material and MethodsWe conducted a retrospective study on 596 echoassisted percutaneous LBs performed in our Department during a 4 years period (2006-2009) for the evaluation of chronic diffuse liver diseases. We in-cluded only those biopsy results that had mentioned both the type of needle and the number of portal tracts. All LBs from this study were echoassisted and performed with Menghini modified needles 1.4 and 1.6 mm in diameter (technique with two passages into the liver), with the patient laying on the left side the place of the biopsy is chosen by means of the ultrasound, usually on the axillary anterior or middle line, so that the costo-phrenic sinus or other structures should be avoided (gall-bladder, colon, intrahepatic vessels, cysts and haemangiomas - when present). The place of the biopsy was marked and after i.v. sedation the liver biopsy was performed randomly with modified Menghini needles of either 1.4 or 1.6 mm (Hepafix; B Braun Melsungen AG, Germany) with 2 passages, with a very short intrahepatic time. Whenever liver cirrhosis was suspected, the 1.6 mm needle was used in order to avoid tissue fragmentation. The 1.6 mm needle was more frequently used as compared to the 1.4 mm needle. An informed consent was signed by all the patients before performing LB.
The liver fragments were analyzed by a senior pathologist, the number of portal tracts was assessed (including only the complete, intact portal tracts) and Knodell score was used to describe necroinflammatory activity as well as fibrosis. Fibrosis was staged on a 0-4 scale: F0-no fibrosis, F1-fibrous portal expansion, F3-bridging fibrosis (portal-portal or portal-central linkage) and F4-cirrhosis.
The statistical analysis was performed using the WINK SDA Software, 7th. Edition (Texasoft, Cedar Hill, Texas, USA) and MedCalc Software (MedCalc program, Belgium). In case of numerical variables (mean number of portal tracts, age), mean value and standard deviation were calculated. Differences between numerical variables were analyzed by nonparametric tests (Mann-Whitney or Kruskal-Wallis tests). The Chi-square (2) test (with Yates, correction for continuity) was used for the comparison of two proportions expressed as a percentage (n designates the total number of patients included in a particular subgroup). 95% confidence intervals were calculated for each predictive test. A p-value < 0.05 was regarded as significant for each statistic test.
ResultsType 1.4 Menghini needles were used for 80 LBs, while 1.6 type was used in 516 LBs. The main characteristics of the patients in whom liver biopsy was performed with the 2 types of needles are presented in the table 1.
The main patients, characteristics in both study groups, in which LB was performed with 1.4 or 1.6 mm Menghini needles.
| 1.4 Menghini needle | 1.6 Menghini needle | p | |
|---|---|---|---|
| Number of LB performed | 80 | 516 | |
| Mean age (years) | 48.1 ± 10.8 | 46.7 ± 12.2 | 0.33 |
| Gender | |||
| Male | n = 31(38.7%) | n = 204 (39.5%) | 0.98 |
| Women | n = 49 (61.3°%) | n = 312 (60.5%) | 0.98 |
| Distribution of fibrosis | F0: n = 12 (15%) | F0: n = 26 (5.1%) | 0.001 |
| (according to the | F1 : n = 47 (58.8%) | F1 : n = 314 (60.8%) | 0.82 |
| Knodell score system) | F3: n = 20 (25%) | F3: n = 167 (32.4%) | 0.23 |
| F4: n = 1 (1.2%) | F4: n = 9 (1.7%) | 0.88 | |
| Etiology of chronic | Chronic hepatitis B: n = 14 (17.5%) | Chronic hepatitis B: n = 134 (25.9%) | 0.13 |
| liver disease | Chronic hepatitis C: n = 61 (76.3%) | Chronic hepatitis C: n = 347 (67.3%) | 0.13 |
| Coinfection: n = 1 (1.2%) | Coinfection: n = 14 (2.7%) | 0.67 | |
| Nonviral: n = 4 (5%) | Nonviral: n = 21 (4.1%) | 0.94 |
The mean number of portal tracts obtained with 1.6 mm Menghini was significantly higher than that obtained with 1.4 mm needles: 24.6 ± 10.6 vs. 20.8 ± 8.6, p = 0.003.
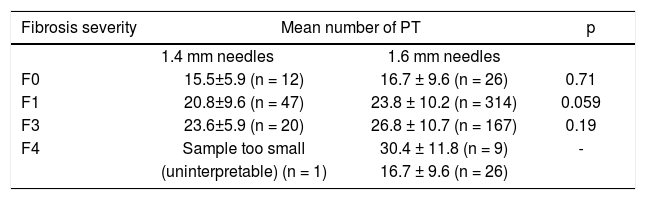
When we considered different stages of fibrosis, the mean number of portal tracts obtained with 1.6 needles vs. 1.4 mm needles was higher in patients with F0, F1 and F3, but the difference did not reach statistical significance (Table 2). When liver cirrhosis was suspected, in almost all cases the 1.6 mm Menghini needles were used, as it can be seen in table 1. All these may explain why the number of portal tracts obtained with 1.6 mm Menghini needles was significantly higher although there was no significant difference between the mean number of portal tracts obtained with 1.4 and 1.6 mm needles in patients with F0, F1and F3 stage.
The mean number of portal tracts obtained with 1.4 and 1.6 mm Menghini needles according to the fibrosis stage.
| Fibrosis severity | Mean number of PT | p | |
|---|---|---|---|
| 1.4 mm needles | 1.6 mm needles | ||
| F0 | 15.5±5.9 (n = 12) | 16.7 ± 9.6 (n = 26) | 0.71 |
| F1 | 20.8±9.6 (n = 47) | 23.8 ± 10.2 (n = 314) | 0.059 |
| F3 | 23.6±5.9 (n = 20) | 26.8 ± 10.7 (n = 167) | 0.19 |
| F4 | Sample too small | 30.4 ± 11.8 (n = 9) | - |
| (uninterpretable) (n = 1) | 16.7 ± 9.6 (n = 26) | ||
No complications or fatalities in relationship with percutaneous liver biopsy were recorded during the study period.
Another target of our study was to see how often we did not obtain enough histological material at liver biopsy using Menghini needle (less than 8 portal tracts). The proportion of LB's specimens with less than 8 portal tracts was similar for both 1.4 and 1.6 mm needles: 8 cases (3.7%) vs. 14 cases (2.7%) (p = 0.87). This is probably not related to the biopsy needle used but to other patient related factors (i.e. obesity).
DiscussionsMainly two types of biopsy needles are used for performing LB: cutting needles (Tru-Cut, Vim-Silverman) and suction needles (Menghini, Klatzkin, Jamshidi), either using a free-hand technique or an automatic (gun) biopsy device. There are only a few published studies which tried to find out if the type of needle used for LB (suction vs. cutting needle) had any influence on the quality of the liver sample.
In a Dutch study7 that compared standard Tru-Cut needle with a new automatic biopsy gun (Ace-cut), the performance of the automatic needle was superior and more consistent with respect to tissue yield, but post-biopsy pain and post-biopsy use of analgesics was observed after automatic biopsy gun.
Thus, the authors concluded that the automatic Tru-Cut needle (gun) offers an advantage, particularly for physicians with no or limited experience in performing LB.
Sherman, et al.8 evaluated the quality of LB specimens in 923 LB in patients with hepatitis C virus infection and advanced liver fibrosis or cirrhosis, according to the type of needle used for LB. In this study automated cutting needles were significantly more likely to provide adequate specimens for eva-luation than aspiration needles and also fewer cases with tissue fragmentation (p < 0.005).
With the Menghini modified needle, due to its construction and to the biopsy technique (one or two passes into the liver in a very short time-described by Menghini in 1958), one or two fragments (each 2 cm long) can be obtained (so that the final liver specimen can be 4 cm long). On the other hand Tru Cut needles for automatic devices are user-friendly, after passing through the abdominal wall and reaching the surface of the liver, only a push of a button is needed in order to obtain a liver fragment, usually 20 mm long.
The Menghini technique requires some experience of the physician performing it, since the time the needle is in the liver must be very short and because usually two passages are performed (best approach). In a Romanian multicentre prospective study9 concerning the influence of the needle type and of the technique used on the sample size, we found that the best LB tissue samples were obtained with Menghini needles, using two intrahepatic passages (this technique is not used in all the Romanian centers). For this type of needle, with two intrahepatic passages, the mean LB fragment was 3.2 ± 1.2 cm long, in comparison with the sample obtained with the same needle, but with only one intrahepatic passage (1.6 ± 1.2 cm) (p < 0.001).
Concerning the safety of different needle types (the risk of complications) there are only very few published papers. In a retrospective study performed long time ago by Piccinino, et al.,10 it was showed that there is a correlation between the complication rate and the needle type used for biopsy: 3.5%c for Tru-Cut needles and 1%c for Menghini needles.10 This rather old study was performed with the old type of Tru-Cut needles, without using the gun device. So, probably, at this moment there are no argu-ments for a higher safety profile of one or another type of needle.
In a systematic review regarding the quality of LB specimens, Cholongitas, et al.,11 found that there were no significant differences in length or number of portal tracts according to needle diameter. On the other hand, Rocken, et al.12 compared the 20-21 gauge Menghini needle with the conventional 17 gauge Menghini needle in a study on 343 liver biopsies and found that tissue specimens in the 20 gauge group were longer as compared to those in the 17 gauge group (29.8 vs. 25.3 mm, p < 0.05), but contained fewer portal tracts (6.7 vs. 9.7). Even so, the authors concluded that the 20-21 gauges Menghini needle could be a reliable alternative for patients with diffuse liver disease and contraindication for large-needle percutaneous LB. Similarly, in a study that compared 59 LBs with 20 gauge (0.9 mm) Menghini needles to 41 LBs with 17 gauge (1.4 mm) Menghini needles, Petz, et al.13 found no significant differences on grading and staging between tissue samples, but in thin-needle specimens, severe fibrosis as well as cirrhosis tended to be underestimated. Contrary to these studies, in a study performed on paired thin-needle (0.8 mm) and large-needle (1.2 mm) biopsy specimens obtained through the same puncture site from 149 consecutive patients with chronic hepatitis C, Brunetti, et al.14 concluded that thin-needle biopsy should be avoided for grading and staging.
But, why must we have very good liver specimens? Poynard, et al.15 demonstrated that LB is not the gold standard for the evaluation of the liver diseases, at least due to the insufficient length of the specimen obtained by LB or to the specimen's fragmentation. In another study of the same author,16 in which LB was compared to FibroTest, the discordance between these two methods (in 18% of cases) was generated especially by biopsy failure (mostly due to small fragment length). Thus, in order to keep LB as a gold standard, we must obtain good specimens in every liver biopsy. Otherwise, noninvasive modalities for the evaluation of liver fibrosis or activity can become more accurate than LB, not being operator dependent.17
In previous studies we tried to find how to improve the performance of LB.18-20 We can speculate that a good personal experience with this type of biopsy is needed (more than 50 or maybe 100 biopsies); that echoguidance should be used; and that the best approach is the one that uses Menghini needles, with two intrahepatic passages, since liver fragments 4 cm long can be obtained by this technique.
Concerning the size of the needle used in the Menghini technique, our study demonstrated that although using 1.4 mm needles with two liver passages is enough to obtain a reliable number of portal tracts (mean 20.8 ± 8.6), better fragments are obtained using the 1.6 mm needles. In cases in which liver cirrhosis is suspected (clinical signs or following elastographic evaluation), 1.6 mm needles can be used to significantly increase the number of portal tracts (24.5 ± 10.6), with a better assessment accuracy. Concerning the risk of complications in correlation with the size of the needle, only one study performed in animals showed that increasing the size of the needle increases the risk of bleeding.21 In our study we did not have any complications or fatalities following LB.
ConclusionThe 1.6 mm Menghini needles provide better liver biopsy specimens, with significant higher number of portal tracts, as compared to 1.4 mm Menghini needles.
Abbreviations- •
LB: liver biopsy.
- •
F: fibrosis.
- •
n: the total number of patients included in a particular subgroup.
None.