As in many areas in medicine, database mining is in vogue in transplant hepatology. Large datasets, such as that of the United Network for Organ Sharing (UNOS), have indeed generated many high impact outcome studies that have advanced the specialty on several fronts, particularly concerning our understanding of recipient mortality. Mortality of the recipient is indeed the single most important clinical outcome when assessing the safety, efficacy, and cost-effectiveness of liver transplant surgery. UNOS and similar databases provide a wealth of knowledge on overall recipient mortality, and enable multivariable analyses of clinico-demographic variables in both donors and recipients to identify risk-or protective factors for recipient mortality.
Unfortunately, long-term (> 3 years) recipient survival has not had the impressive incremental improvements which we have witnessed in short-term recipient survival. Furthermore, outcome studies in liver transplantation have failed to translate into any meaningful improvement in long-term recipient survival. The questions then become: Have long-term recipient survival rates after liver transplantation reached their plateau, or is there room to improve further? And can the study of specific causes of death, rather than all-cause mortality, provide clinical insight and improve patient outcomes?
To answer these important questions, the liver transplant community must make a concerted effort to collect and analyze data on causes of death after liver transplantation. Such an analysis might allow us to determine to what degree recipient deaths are related to chronic immunosuppression, and this in turn might allow us to develop individualized post-transplant care pathways to improve long-term mortality and morbidity. Liver transplant programs face challenges in collecting recipient mortality statistics, and databases fall short in providing this level of detail. Liver transplant programs usually serve large regional catchment areas, and this geography inherently hinders follow-up care and data accrual. Moreover, issues such as patient privacy, and lack of centralized computer-based health records, impose further barriers to mortality data acquisition.
Our center, located in a medium-sized Canadian city, is fortunate to maintain exceptional long-term follow-up data. We postulate that the reason for this is the relative shortage of subspecialized care available in our largely rural catchment area, as well as patient and referring provider preference that recipients continue to receive indefinite long-term care at our institution. As such, our program is able to capture data on cause of death where databases, and indeed many centers, cannot.
Herein, we present mortality data for 134 consecutive deaths which we tracked from 2005 to 2010. From 2000 to 2010, our center had 1-, 3-, 5-and 10-year mortality rates of 8.8, 13.5, 14.8, and 16.4%, respectively. For this study, causes of death were ascertained from patient charts, autopsies (where performed), and from next-of-kin. Stata 11.0 was used for descriptive statistics. Categorical variables were reported as frequencies with percentages, and continuous variables were reported as means with standard deviation (SD).
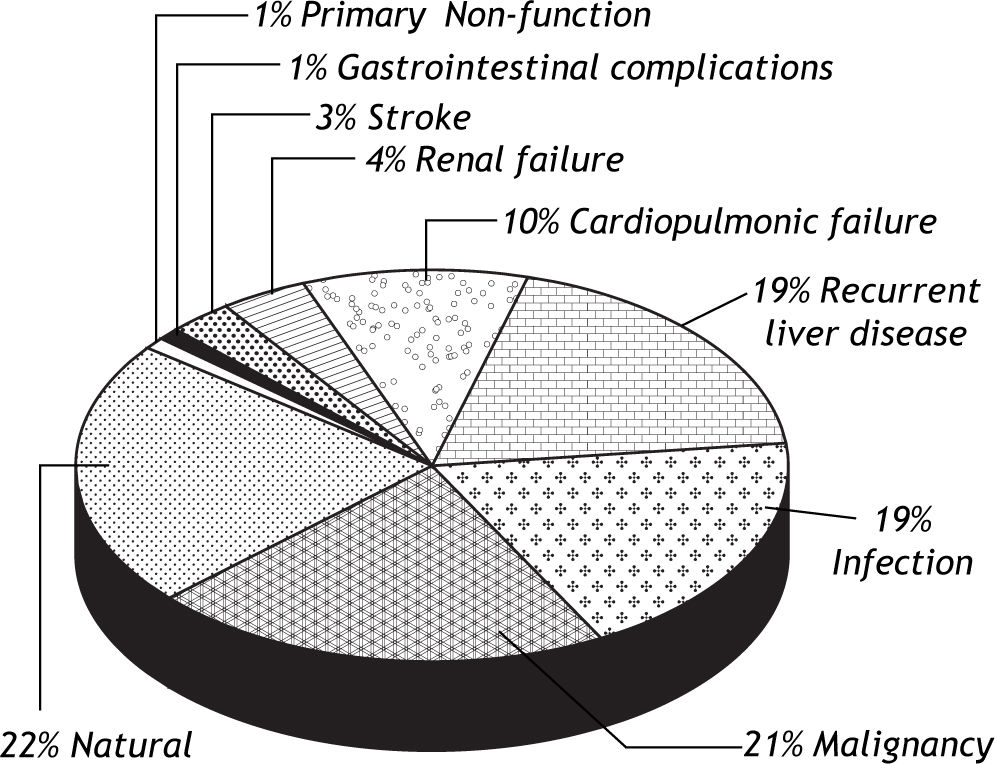
The mean ages of the study cohort at the time of transplant and at the time of death were 51.1 years (SD 10.6) and 54.6 years (SD 11.3), respectively, and 102 subjects (76.1%) were male. The mean time from transplantation to death was 3.5 years (SD 4.2). The most common underlying etiologies of liver disease were alcohol in 42 subjects (31.3%), hepatitis C virus in 40 (29.9%), autoimmune liver disease in 18 subjects (13.4%), and non-alcoholic fatty liver disease in 15 subjects (11.2%). 19 patients (14.1%) had underlying hepatocellular carcinoma (HCC). The causes of death are summarized in figure 1. The 4 most frequent causes of death were natural causes in 29 patients (21.6%), malignancy in 28 (20.9%), infection in 25 (18.7%), and recurrent liver disease in 25 (18.7%). Among the subjects with recurrent liver disease, hepatitis C virus was the most common, occurring in 20 patients (80.0%). In this series, we estimated that 103 deaths (76.9%) were associated with immunosuppression from transplantation (all deaths from malignancy, infection, cardiopulmonic or renal failure, stroke, and primary non-function).
This descriptive study sheds light on the causes of death after LT in a small series from a single-center. Such detail is non-existent in large transplant databases that generate significant outcomes research on liver transplant recipients. From these results, we conclude that mortality is frequently associated with immunosuppression among LT recipients-an assertion well-supported in the literature.1-3 In our series, the majority of patients with death from recurrent disease had hepatitis C, corroborating with prior publications and underscoring the magnitude of this problem in the post-transplant set-ting.4,5 Our analysis also highlights the importance of developing new, individualized strategies in the long-term management of liver transplant recipients to minimize overall immunosuppression exposure given high rates of post-transplant malignancy and complications from metabolic syndrome – both of which have strong associations with immunosu-ppression.6,7
There are serious limitations to our analysis. First, our sample size was relatively small and from a single center, thereby limiting the external validity of our findings. Second, while we can describe the causes of death, a case series cannot assess/quantify the risk of immunosuppression in recipient mortality as there is no matched control without immunosu-ppression. Third, subgroups of patients classified by cause of death were too small to perform any meaningful risk estimates. Lastly, although our program has excellent long-term follow-up care, we cannot be absolutely certain that some subjects who died during the data accruement period were missed, in particular for the minority of subjects who reside outside of our province. This latter limitation introduces a possible selection bias in our study population.
However, despite the numerous shortcomings, our descriptive study on causes of death after liver transplantation serves an important purpose to illustrate that studying detailed mortality statistics is a vital exercise in transplant hepatology, and there are surprisingly no multicentered robust studies in this area. Additionally, our case series affirms the limitations of the current state of outcomes research in transplant hepatology, and emphasizes the importance of prospective, multicentered data collection on causes of death in liver transplant recipients. A better understanding of mortality might impact on recipient selection criteria and medical management of the post-transplant recipient. Blind acceptance of the stagnant rates of long-term recipient mortality after liver transplantation without carefully studying the causes of death, and without efforts to assess strategies to reduce the risk of death, is a disservice to our patients.
Conflicts of interest and disclosuresNone for both authors.