In Budd Chiari Syndrome (BCS), a rare cause of hepatic failure, hepatic outflow is impaired through thrombosis or stenosis. Decreased sinusoidal blood flow and centrilobular ischemia results in subsequent tissue necrosis.1 Later, fibrotic remodelling occurs predominantly in the centrilobular area, leading to portal hypertension with eventually the development of ascites and esophageal varices.2
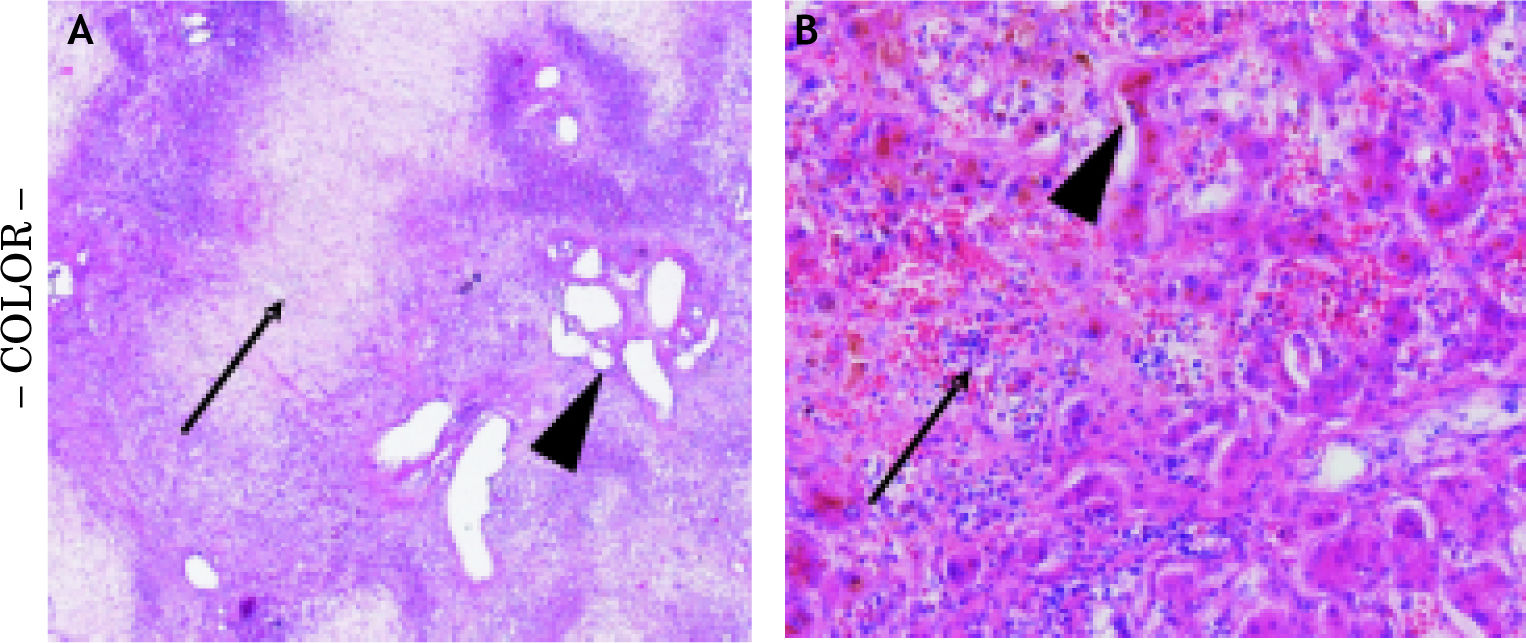
Here, we report the case of a 56-year-old female patient who was referred to our hospital for acute hepatic failure of unknown origin. On admission, typical clinical signs of a BCS such as jaundice, ascites and peripheral edema were present for 5 weeks. The patient reported an episode of abdominal discomfort eight months prior to admission to our hospital. The arterial phase of a CT scan of the abdomen at this time had shown a patchy appearance of the liver, the portal-venous phase was without pathological findings (Figure 1, Panel A, B). Being self-limited, the complaints and the findings from the CT scan were not pursued further. The past medical history revealed no additional diseases and the patient did not take any medication. She did not consume any alcohol but smoked cigarettes for 30 years.
Arterial phase (A) and portal venous phase (B) of a CT scan 8 months prior to admission. The arterial phase displays a patchy appearance of the liver, suspicious for perfusion deficiency. No thrombosis in the venous outflow tract could be identified. C. Portal venous phase of a CT scan on admission shows a marked hepatomegaly and dysmorphic features of the liver. The patchy aspects have disappeared. Neither thrombosis nor stenosis of the hepatic outflow tract were identified.
On admission, physical examination revealed a distended liver and peripheral edema. Laboratory results were as follows: alanine aminotransferase 60 U/L, aspartate aminotransferase 54 U/L, gamma glutamyl transferase 132, choline esterase 2700 U/L, bilirubin 15.4 mg/dL, INR 1.77.
Antinuclear-antibodies, anti-cardiolipin and anti-β2 Glycoprotein antibodies were not detectable and immunoglobins and IgG were within normal limits rendering anti-phospholipid syndrome and autoimmune hepatitis unlikely. In addition, infectious hepatitis, Wilson’s disease and alphal-antitrypsin deficiency were excluded serologically and by laboratory testing. Gastroscopy revealed 1st degree esophageal varices. A CT scan showed an enlarged and dysmorphic liver indicating a chronic or acute-on-chronic liver damage (Figure 1, Panel C). No thrombosis or outflow obstruction was identified in this CT scan and on ultrasound. The patchy appearance of the liver that was described eight months earlier was not present anymore.
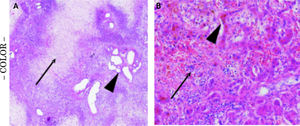
Laparoscopic liver biopsy showed sequelae of a marked perfusion deficiency with a destruction of the centrilobular parenchyma and canalicular cholestasis (Figure 2). However, no vascular obliterations were identified (Figure 2). The patients state and liver function deteriorated rapidly and high urgency orthotopic liver transplantation was performed. Histological work-up of the explanted liver did not show alterations of the large hepatic veins but changes that were compatible with a BCS. There was no evidence for liver injury of any other cause. Unfortunately, the patient never fully recovered and died from sepsis due to enterococcus 2 months later. An autopsy was not performed.
Microscopic specimen in low (A). 50x and high (B). 200x, magnitude amplification obtained by laparascopic liver puncture. Biopsy specimen revealed vanishing hepatocytes in the central parenchyma (Panel A, arrow) and portal fields with ecstatic lymph vessels (Panel A, arrowhead) compatible with severe perfusion disturbances. Higher magnification displayed bile duct proliferation (Panel B, arrow) and atrophic hepatocytes (Panel B, arrowhead). There is no relevant inflammation and no indication for liver vein thrombosis.
The question remained what had caused this striking and fatal course in a patient with no prior illnesses. The patient presented to our hospital with liver failure and the clinical signs and histological alterations typical of a BCS.3 However, no thrombosis or obstruction of the hepatic outflow tract were identified neither on ultrasound, nor on CT scan or histologically. BCS is defined as a liver disease secondary to an obstruction of the hepatic venous outflow tract.4 Therefore, the question arises whether this case represents a BCS. Taking into consideration the CT scan eight months prior to admission, we postulate that the onset of the disease really occurred 8 months earlier and we speculate that thrombolysis and spontaneous re-canalisation of the hepatic outflow tract occurred secondary to the deterioration of hepatic function.
This case dramatically illustrates that the onset of a BCS may happen a long time prior to presentation of an apparent acute liver failure and that in certain instances a recanalization of an obstructed hepatic outflow tract may occur during the course of the disease. In this scenario, a diagnosis of BCS should be taken into consideration even if imaging does not identify hepatic outflow obstruction and this has possible implications for treatment as prophylaxis by means of anticoagulation. In conclusion, our case indicates that BCS might account for a number of apparent acute liver failures of unknown origin, especially if the liver displays a marked dysmorphic appearance, typical for BCS.1
Abbreviations- •
BCS: Budd Chiari Syndrome
- •
INR: International Normalized Ration
- •
CT: Computer Tomography