Abstracts of the 2025 Annual Meeting of the ALEH
More infoTo evaluate the accuracy of an artificial intelligence (AI) model, based on routine clinical and laboratory data, in predicting the risk of developing hepatocellular carcinoma (HCC) in patients with Metabolically Associated Steatotic Liver Disease (MASLD). Our aim was to create and validate a tool to support risk stratification and facilitate early surveillance of high-risk individuals.
Materials and MethodsThis was a retrospective case-control study including 306 MASLD patients divided into an HCC group (129 patients), with diagnosis confirmed by histopathological criteria or LI-RADS classification, and a control group (177 patients). Collected variables included age, body mass index, comorbidities (diabetes mellitus, dyslipidemia, presence of portal hypertension), and serum laboratory parameters: aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, creatinine, platelets, cholesterol (HDL, LDL, and triglycerides), and non-invasive indices: neutrophil-to-lymphocyte ratio (NLR), FIB-4, and AST/ALT ratio. The XGBoost (Extreme Gradient Boosting) AI algorithm was implemented, and the dataset was randomly split into a training cohort (80%) and an internal validation cohort (20%) to develop and assess the model’s performance.
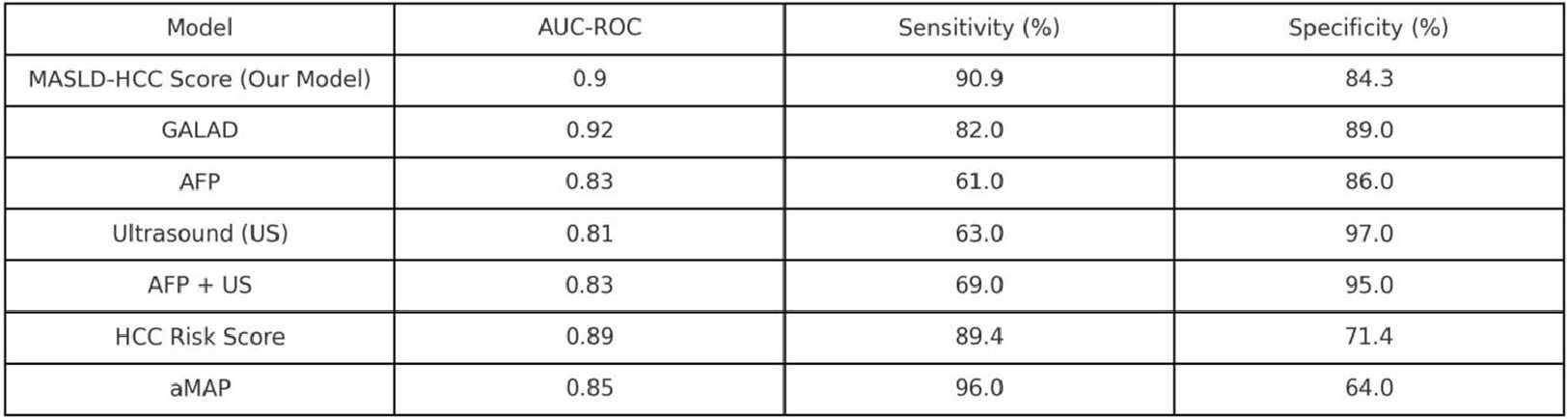
ResultsThe AI model demonstrated high discriminative ability for HCC, achieving an area under the ROC curve (AUC-ROC) of 0.9, with a sensitivity of 90.9% and specificity of 84.3%. The strongest predictors of HCC were serum creatinine, followed by the presence of portal hypertension, elevated NLR, and LDL levels.
ConclusionsThe AI-driven model, developed using widely available clinical and laboratory parameters, demonstrated excellent performance in identifying MASLD patients at high risk of developing hepatocellular carcinoma. By enabling early and cost-effective risk stratification, this tool may support targeted surveillance strategies and improve clinical decision-making in real-world hepatology practice.