Gyromitra esculenta, also known as “false morel” is one of the most poisonous mushrooms. This species is found all over the world, growing in coniferous forest in early spring time. Common manifestation of poisoning includes gastrointestinal symptoms which include varied degrees of liver impairment.
We describe three cases: acute liver injury, acute liver failure and acute-on-chronic liver failure due to G. esculenta poisoning. At admission patients presented with encephalopathy and features of liver failure. Two of them recovered completely following supportive management while the remaining patient who also had preexisting liver disease developed multiorgan failure and subsequently died.
Although a rare occurrence, G. esculenta poisoning should be considered in the differential diagnosis of acute liver failure.
Among thousands of mushroom species that are found all over the world, approximately one hundred are poisonous to humans. Most of them cause mild symptoms, such as gastrointestinal disturbances like nausea, vomiting, diarrhea, or other manifestations like fever, muscle pain and a headache. Poisonous mushroom ingestion could also result in severe, life-threatening toxicity [1].
Acute liver failure (ALF) manifests with abnormal liver functions with impaired coagulation (INR >1.5) and signs of encephalopathy, and manifestations of the latter could be up to 24 weeks from onset of illness in a patient with no previous history of liver disease. Whereas the term of acute liver injury (ALI) refers to patients with coagulopathy and no signs of encephalopathy [2,3]. Its occurrence following Amanita phalloides mushroom poisoning is well known with the associated morbidity, mortality and often the need for liver transplantation in a significant proportion of cases. However, ALF due to Gyromitra esculenta mushrooms ingestion is less well reported.
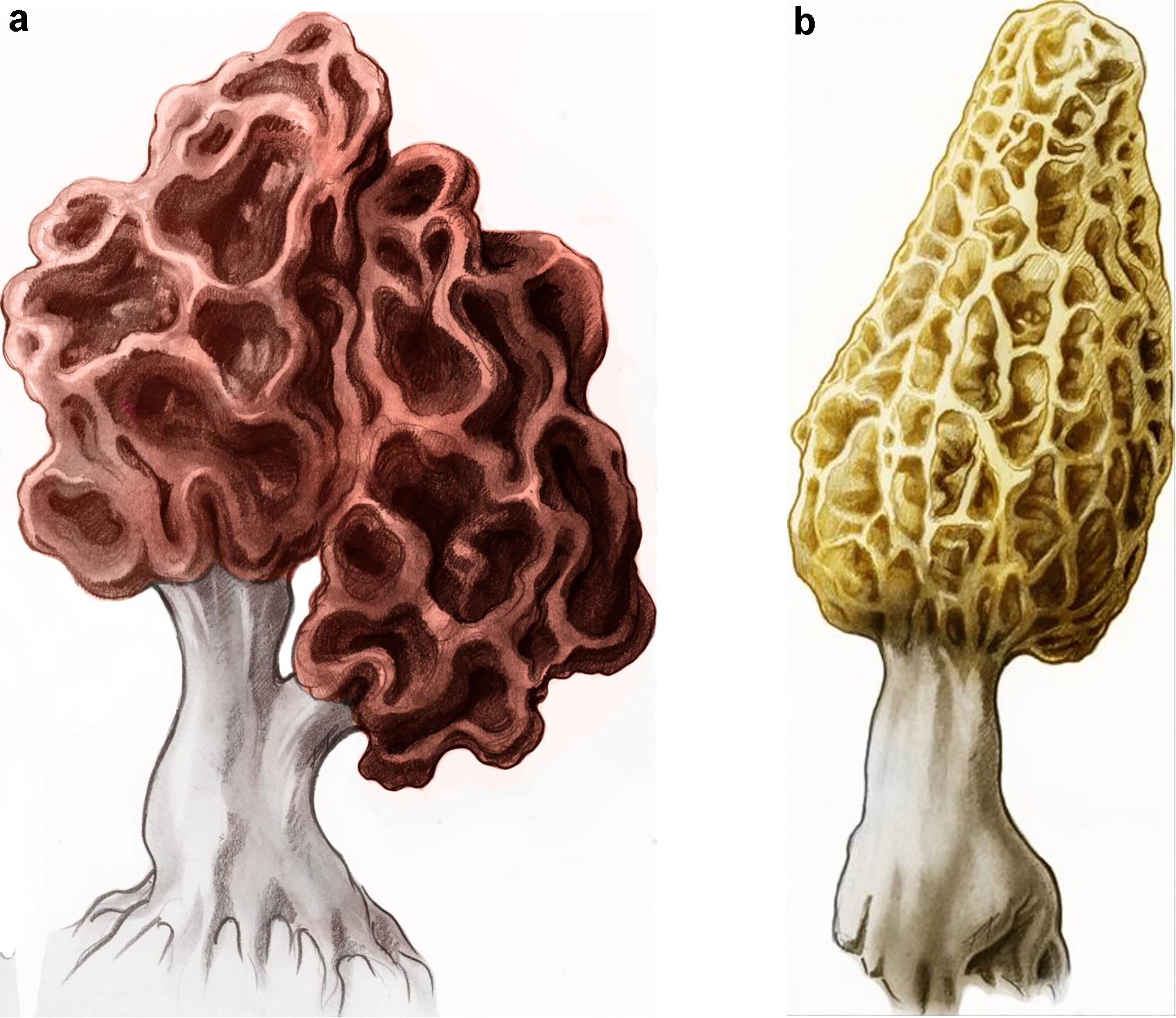
G. esculenta, also known as a “false morel” (Fig. 1a), is well documented as one of the most poisonous mushrooms. This species grow all over the world mostly in coniferous forests in early spring time. The mushroom is of medium size (5 up to 16cm) with a typical irregular ‘brain-shaped’ cap (Fig. 1a). Unfortunately, “false morel” is easily confused with Morchella esculenta (Fig. 1b), which is known as a “true morel” and an exclusive culinary product [4].
Herein, we describe a case of acute liver injury, a case of ALF and an additional case of acute-on-chronic liver failure (ACLF) due to G. esculenta poisoning. Two patients recovered following typical medical treatment while a patient with acute-on-chronic liver failure died.
2Case 1 – acute liver injuryA 61-year-old male patient was admitted to our unit in April 2014, two days after eating “brain-like” mushrooms. The patient experienced abdominal pain two days after the mushroom ingestion and this was associated with vomiting, intense watery diarrhea, and on admission was jaundiced. There were no signs of encephalopathy. Laboratory tests confirmed ALI (Table 1). Abdominal ultrasound showed signs of minor liver enlargement. Following supportive medical treatment the liver functions improved. The patient was discharged home 9 days after admission.
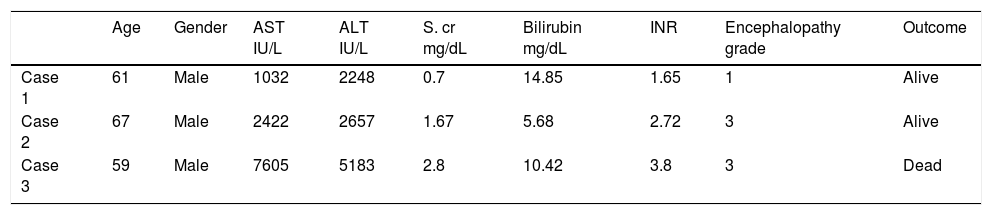
A comparison of laboratory features at admission between three cases after Gyromitra esculenta poisoning.
| Age | Gender | AST IU/L | ALT IU/L | S. cr mg/dL | Bilirubin mg/dL | INR | Encephalopathy grade | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 61 | Male | 1032 | 2248 | 0.7 | 14.85 | 1.65 | 1 | Alive |
| Case 2 | 67 | Male | 2422 | 2657 | 1.67 | 5.68 | 2.72 | 3 | Alive |
| Case 3 | 59 | Male | 7605 | 5183 | 2.8 | 10.42 | 3.8 | 3 | Dead |
Normal ranges: AST 5–40U/L; ALT 7–56U/L; INR 0.9–1.3; total bilirubin 0.2–1.2mg/dL; serum creatinine 0.6–1.2mg/dL; encephalopathy grade West Heaven 0–4.
Abbreviations: ALT, alanine transaminase; AST, aspartate aminotransferase; S.cr, serum creatine; INR, international normalized ratio.
A 67-year-old male patient was admitted to our Unit in April 2016 with signs of abdominal pain, fever, headache and jaundice that were followed by altered mentation. This occurred three days after ingestion of mushrooms, which the patient described as being very similar to “true morels”. The patient was irritable, mildly confused and found to be jaundiced with a tender right upper quadrant of abdomen. Laboratory blood tests confirmed acute liver failure (Table 1) and the patient had signs of encephalopathy grade 3 according to West Haven Criteria [5]. The patient continued to deteriorate despite supportive care and required listing for a liver transplantation. The decision for liver transplantation was based primarily on rapidity and severity of deterioration even though the patient did not fulfill all of the Kings College criteria [6] for listing in fulminant hepatic failure. The clinical picture however stabilized and there was improvement noted in the 48h that followed resulting in the patient being taken off the waiting list for a transplant. After eleven days of continued medical treatment, the patient improved to be discharged home with liver function tests normalized.
4Case 3 – acute-on-chronic liver failureA 59-year-old man with a history of HCV hepatitis (untreated, diagnosed in 2002) and diabetes presented in April 2016, three days after eating mushrooms, which his family described as a “false morel”. A few hours after ingestion symptoms including muscle pain with vomiting and diarrhea were observed. At admission he had grade 3 encephalopathy. The patient rapidly developed multi-organ failure requiring inotrope support, invasive ventilator support and hemodialysis (Table 1). He also required glucose infusion to maintain normoglycemia. He received a standard treatment with intravenous colloids, crystalloids and glucose. His encephalopathy was treated with intravenous l-ornithine l-aspartate. The abdominal ultrasound revealed enlarged and heterogenous liver parenchyma with no signs of portal hypertension and normal spleen. The patient did not however fulfill the Kings College criteria [6]. Despite signs of continued deterioration of liver function the option of liver transplantation was not considered feasible due to established multi-organ failure. The patient died 5 days following mushroom ingestion.
5DiscussionThere are various types of wild mushrooms growing in forests, which are often eaten by foragers. Only about 2% (out of more than 5000 species that are found worldwide) are poisonous. This includes G. esculenta, so called “false morel” [7]. Herein, we describe the clinical course of three patients to emphasize variable symptoms of poisoning.
The poisoning with G. esculenta should be considered and differentiated from other causes of toxic liver failure which occur in the spring time, as opposed to A. phalloides occurring in autumn. It is also not typically shaped with a stem and a cap [8,9].
The manifestations of poisoning following ingestion of G. esculenta usually occur around 12h following ingestion with gastrointestinal symptoms followed by jaundice within 2–3 days and significant increase of AST, ALT and INR with a degree of encephalopathy. There is a paucity of reported publications of poisoning following ingestion of G. esculenta, limited to a few case reports [10,11]. In these too most patients described failed to fulfill criteria for ALF or even ALI, with moderate transaminitis being the main feature. However, fatal cases have also been reported [12]. The toxin gyromytrin, chemically identified as an N-methyl-N-formylhydrazone is a water soluble compound that evaporates easily at normal temperatures [13]. The toxin could be therefore partially deactivated or even eliminated by cooking or drying. However partial cooking could lead to hydrolyzation which could also be caused by the acidity of the stomach following ingestion, to the direct toxin-monomethylhydrazine (MMH). Metabolic intermediates of gyromytrin toxin-free methyl radical and an unstable diazonium compound, which arises after oxidation from MMH damage hepatocytes, causing their necrosis and interfere with cytochrome enzymes (mainly P450), aminooxidases and glutathione pathways [14]. This may be combined with a degree of neurotoxicity by modulating pyridoxine dependent coenzymes, therefore having influence on gamma-aminobutyric acid (GABA) levels [15].
The three patients described developed liver disfunction of varied severity following G. esculenta poisoning. Our report highlights the possibility G. esculenta ingestion may cause an acute liver failure. It is likely that in subjects with underlying or preexistent liver dysfunction the course may be very aggressive with death a likely outcome.
Described cases show limited utility of widely used criteria selecting patient with urgent need of transplantation [6]. This reinforces the need to develop new prognostic or diagnostic tests of high sensitivity and specificity that would allow adequate placing patients on high urgency waiting list for liver transplantation.
The clinical indications for emergency liver transplantation are commonly based on the King's College Hospital Criteria or Clichy criteria [6]. However, their sensitivity and specificity in patients with ALF due to some rare causes are not clearly specified. The utility of Kings College criteria has previously been evaluated in case of A. phalloides poisoning. Interestingly, the sensitivity of only 25% with 80% specificity of predicting poor outcome in case of amatoxin induced ALF have been reported [16]. This contradicts with a series reported by Escudie et al. [17] who reported Kings College sensitivity and specificity of 100% each in case of A. phalloides poisoning. According to Ganzert et al. [18], the combination of serum creatinine above 106μmol/L and PT index less than 25% strongly suggests the urgent need for liver transplantation [18].
Some parameters may also be helpful in predicting prognosis, among them proven factors of poor outcome are: encephalopathy and kidney impairment [17], lactic acidosis, especially when observed with coexisting hepatic encephalopathy [19], time interval shorter than 8h between eating mushrooms and the occurrence of first symptoms (such as vomiting or diarrhea [16]. Nevertheless, majority of prognostic factors following mushroom intoxication refer to A. phalloides poisoning. In comparison however there is less known about G. esculenta poisoning to help with prognostication.
In summary, G. esculenta poisoning represents a rare but potentially dangerous clinical scenario that should always be considered in the spring time in regions it is found. Given the limited sensitivity and specificity of currently available prognostic criteria, such patients should preferably be transferred to liver transplant and hepatology units early. Efforts should be made to develop more precise and sensitive prognostic criteria that could help clinicians in selecting the patients for liver transplantation.AbbreviationsACLF acute-on-chronic liver failure acute liver failure acute liver failure international normalized ratio gamma-aminobutyric acid monomethylhydrazine
Nothing to declare.