Introduction. The aim of this study is to investigate large volume therapeutic paracentesis using either a z-tract or axial (coxial) technique in a randomized controlled trial.
Materials and methods. In this randomized, single blind study, patients with cirrhosis undergoing outpatient therapeutic paracentesis were randomized to the z-tract or the modified angular (coaxial) needle insertion technique. Subject and procedure characteristics were compared between the groups with ascites leakage as quantified by need for dressing changes with standardized sized gauze pads as a primary endpoint and subject procedural discomfort, operator preference, and procedure complications as secondary endpoints.
Results. 72 paracenteses were performed during the study period: 34 to the z-tract and 38 to the coaxial insertion technique. Following exclusions, a total of 61 paracenteses were analyzed: 30 using the z-tract technique and 31 using the coaxial technique. There were equal rates of post-procedural leakage of ascites between groups (13% in both groups, p = 1.00). Using the visual analog scale (0 - 100), there was a statistically significant increase in the subject reported pain score with the z-tract compared with the coaxial method [26.4 (95% CI 18.7 - 34.1) vs. 17.2 (95% CI 10.6 - 23.8), p = 0.04]. Mean physician rated procedure difficulty (1 - 5) was significantly higher for the z-tract vs. the coaxial technique [2.1 (95% CI 1.6 - 2.6) vs. 1.5 (95% CI 1.2 - 1.8), p = 0.04].
Conclusion. When compared to the z-tract technique, the coaxial insertion technique is superior during large volume paracentesis in cirrhosis patients.
Ascites is the most common complication of cirrhosis and affects nearly half of all patients within the first 10 years of diagnosis.1 Paracentesis is a diagnostic and therapeutic procedure used to treat ascites. Reports describing paracen-tesis date as far back as Hippocrates in ancient Greece, but Talma reported its first modern application in 1889.2 However, its consistent and successful use is a more recent phenomenon owing partially to the concomitant administration of albumin with removal of large volumes of ascites. In the 1950’s, paracentesis fell out of favor coinciding with the advent of medicinal diuretics, implementation of dietary sodium restriction, and development of surgical alternatives.3 It was not until the mid-1980’s that paracentesis began to fall back into favor for the treatment of medically refractory as-cites following the performance of randomized, controlled trials comparing diuretics to paracentesis.3,4
Although large-volume paracentesis is now routinely performed, there has not been a systematic study addressing the optimal method of needle insertion during large volume paracentesis. Without evidence, practitioners rely on anecdotal experience based on personal preference usually passed down from prior training.5,6 The New England Journal of Medicine published a didactic video and accompanying instructional article on the performance of paracentesis in 2006.7 This video describes two accepted techniques: z-tract technique and the angular insertion technique. Both techniques are designed to minimize post-procedural ascitic fluid leakage with current rates of leakage estimated to be 5%.8 To determine the optimal method for needle insertion during paracentesis, we aimed to compare the z-tract technique to the modified angular technique used at the University of Virginia Hospital, commonly called the coaxial technique.
Material and MethodsSubjects with cirrhosis previously scheduled for outpatient paracentesis at the University of Virginia were recruited between August 2013 and April 2014. Inclusion criteria included age 18 years and older, diagnosis of cirrhosis (as confirmed by liver biopsy or clinical and imaging findings), and the ability to reliably be contacted by phone in 24 h. Exclusion criteria included subjects with a contraindication to paracentesis, removal of less than 5 liters of ascites (as to only include large volume paracente-sis), malignant ascites, or inability or unwillingness to give informed consent.
After written informed consent was obtained and demographic data were collected, subjects were randomized to the z-tract or to the coaxial needle insertion technique using blinded allocation. Per institutional review board regulations, no screening failure log was kept. A computerized random number generator allocated subjects in a 1:1 fashion in blocks of one. The subjects, but by necessity not the operators, were blinded to the technique used for paracentesis. Subjects were allowed to re-enter the study on subsequent paracenteses and were re-randomized on each subsequent entry. All procedures were performed by Gastroenterology and Hepatology fellows (PGY4-6) in the outpatient gastrointestinal procedure unit at the study site under the supervision of Hepatology faculty. Additionally, all fellows were previously credentialed to perform para-centesis independently.
The subject was placed in a supine position with the head of the bed elevated to approximate a 30-degree incline. The left lower quadrant was preferentially used and the preferred needle insertion site was two finger breadths cephlad and two finger breadths medial to the anterior superior iliac spine. Bedside ultrasound was performed to locate and confirm presence of an adequate pocket of as-cites for drainage. Paracentesis was performed using the Halyard/Kimberly-Clark Quick-Tap Paracentesis Tray (Roswell, Georgia). This includes a Caldwell needle/can-nula (15 gauge x 8.26 cm) and two needles used to administer lidocaine 1% anesthetic (22 gauge x 3.81 cm and 25 gauge x 2.54 cm). The subject was prepped in a sterile manner and lidocaine was injected into superficial and deeper tissues along the tract to be used during insertion of the drainage needle/cannula. A #11 scalpel was used to make an incision adequate to allow for easy passage of the needle/cannula. Needle/cannula insertion was then performed as determined by the randomization protocol. For the z-tract technique, the cutaneous tissues were pulled 2 cm caudad before the needle/cannula was inserted and advanced. This prevented direct overlap of the cutaneous insertion site and peritoneal insertion site when the needle/ cannula were withdrawn. For the coaxial insertion technique, the needle/cannula was directly inserted and advanced to minimize the distance between the cutaneous tissues, peritoneum and ascites. To standardize needle insertion, all physicians performing the procedure were trained using the NEJM paracentesis teaching video7 and under the guidance and observation of study personnel in addition to performing directly supervised procedures using both techniques prior to involvement in the study. After needle/cannula insertion in either technique, the inner needle was removed and the cannula was connected via sterile tubing to suction. After drainage of ascites, the cannula was removed and a standardized gauze pad [Smith & Nephew Primapore 7.2 cm x 5 cm (Hull HU3 2BN, United Kingdom)] was applied to the insertion site. Those subjects who drained 5 liters of ascites or more were included in the study and given 25 g/100 mL albumin intravenously at a dose of 6 - 8 g per liter of ascites removed.
Immediately following the paracentesis, subjects were asked to rate their pain during the procedure using the visual analog scale. The visual analog scale is a continuous pain scale measured by having the subject place a line perpendicular to a horizontal 100 mm pain measurement line.9 This was measured to provide a range of pain scores from 0 - 100. Additionally, the operator was asked to rate the overall procedure difficulty on a scale of 1 - 5. The subject was then given 10 numbered bandages and instructions on applying the bandages to the paracentesis site in the case of leakage. Subjects were contacted by telephone approximately 24 h following their paracentesis to ask if they had ascites leakage (yes/no). This was defined as needing to change their bandage at least once due to saturation with ascites fluid. Subjects were asked how many bandages were needed to be used secondary to leakage and if any delayed complications occurred related to their procedure. The primary endpoint of the study was the rate of leakage from the paracentesis site after discharge from the procedure suite within 24 h. Secondary endpoints were perceived pain experienced by the subject during the procedure and operator rated difficulty of performing the procedure. This study was approved by the University of Virginia Institutional Review Board (16842) and the trial was registered with ClinicalTrials.gov (NCT02310165). The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the University of Virginia Institutional Review Board.
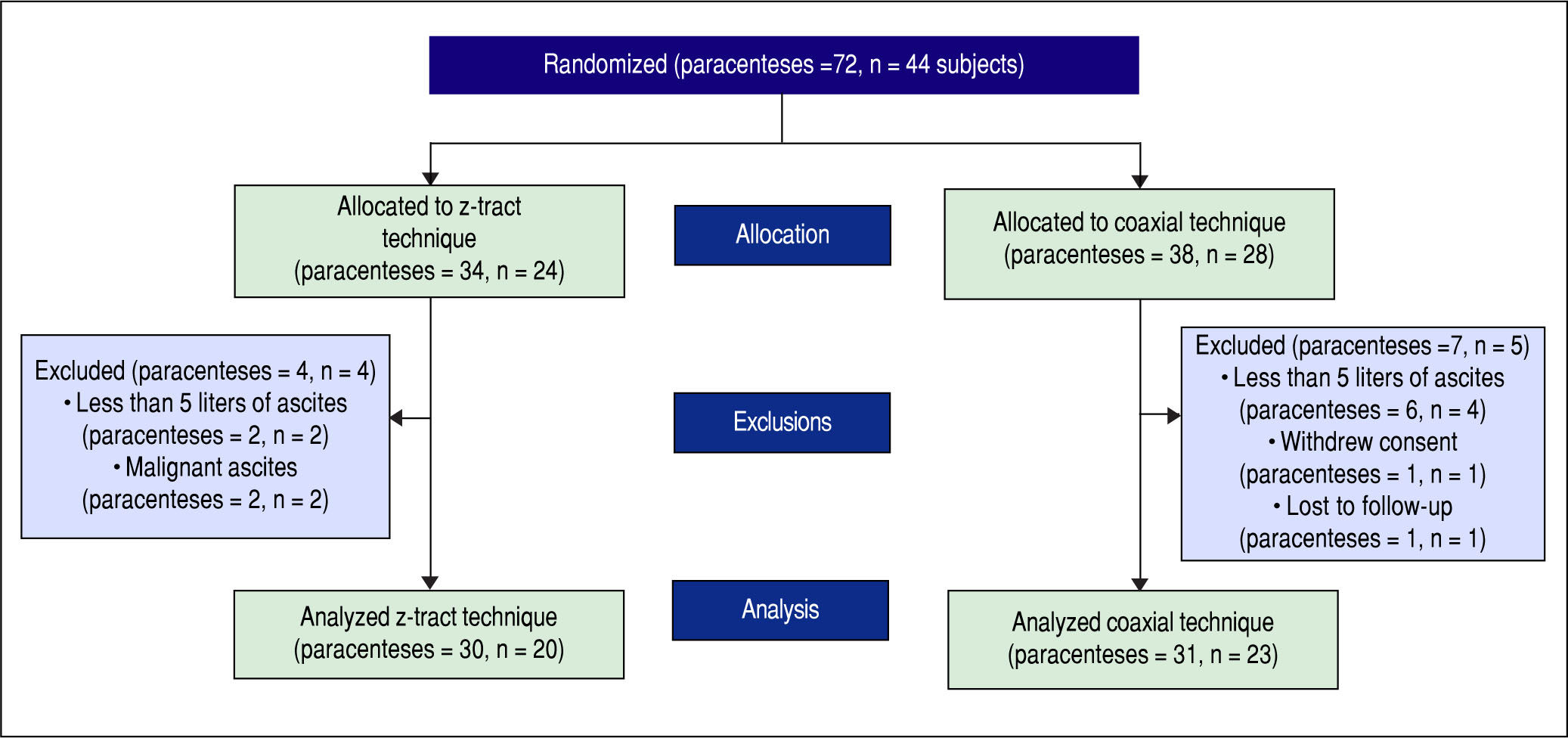
Subject enrollment in the protocol is illustrated in Figure 1. All subjects who signed informed consent were randomized. As per exclusion criteria, those paracenteses with less than 5 liters of ascites withdrawn (8), were later found to be done for malignant ascites (2), or the subject withdrew informed consent (1) were excluded from the analysis. The remaining paracenteses were analyzed in an intention to treat analysis. Demographics, subject characteristics, and endpoints were analyzed between groups using the χ2 or Fisher exact test where appropriate for categorical variables and the Student t-test or Wilcoxon signed rank test where appropriate for continuous variables. Adjusted analyses using multivariate models were performed using logistic regression and the log-rank test. All comparisons were two-sided and an alpha ≤ 0.05 was considered statistically significant. Dataset manipulation and statistical analysis were performed using SAS (Cary, NC) version 9.2. Using historical ascites leakage rates of 10% and the assumption of a ± 200% difference in leakage rates between techniques, assuming 0.80 power, we predicted a total sample size needed to show a difference in primary endpoints of 62 in each group. A pre-determined interim analysis was performed at the halfway point of enrollment to assess for a difference in side effects or complications between groups. As part of this interim analysis, a statistically significant difference in procedural pain between groups was found. At this point, the study team decided to stop further enrollment due to the potential safety difference between groups.
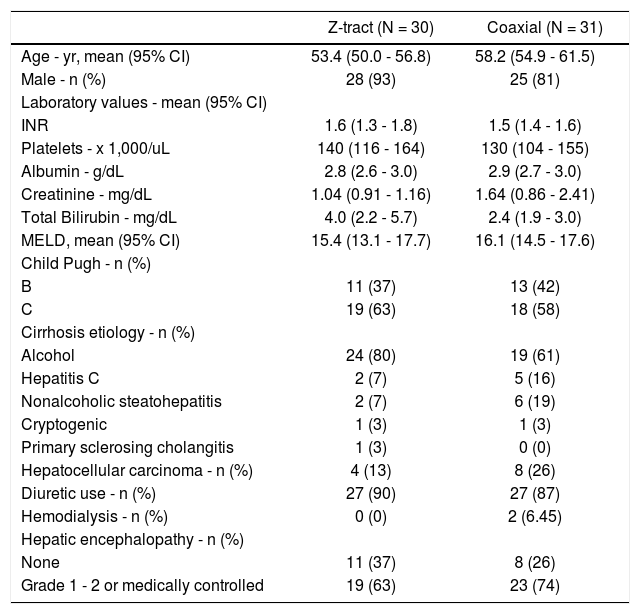
RESULTSFrom August 2013 to April 2014 a total of 44 subjects were enrolled for 72 consecutive paracenteses. The procedures were randomized to the z-tract (34) or to the coaxial insertion technique (38). Following exclusion of 11 para-centeses (delineated in Enrollment and Statistical Analysis), the final analyzed data included 30 paracenteses using the z-tract technique and 31 paracenteses using coaxial technique (Figure 1). Baseline characteristics, presented in table 1, were equal between the groups except for the mean age [53.4 yr (95% CI 50.0 - 56.8) in the z-tract group vs. 58.2 yr (95% CI 54.9 - 61.5) in the coaxial group, P = 0.04]. Additionally, procedural factors including lidocaine use, number of needle passes, liters of ascites removed, and albumin administration post-procedure did not differ (Table 2).
Baseline characteristics of the study participants at enrollment.*
| Z-tract (N = 30) | Coaxial (N = 31) | |
|---|---|---|
| Age - yr, mean (95% CI) | 53.4 (50.0 - 56.8) | 58.2 (54.9 - 61.5) |
| Male - n (%) | 28 (93) | 25 (81) |
| Laboratory values - mean (95% CI) | ||
| INR | 1.6 (1.3 - 1.8) | 1.5 (1.4 - 1.6) |
| Platelets - x 1,000/uL | 140 (116 - 164) | 130 (104 - 155) |
| Albumin - g/dL | 2.8 (2.6 - 3.0) | 2.9 (2.7 - 3.0) |
| Creatinine - mg/dL | 1.04 (0.91 - 1.16) | 1.64 (0.86 - 2.41) |
| Total Bilirubin - mg/dL | 4.0 (2.2 - 5.7) | 2.4 (1.9 - 3.0) |
| MELD, mean (95% CI) | 15.4 (13.1 - 17.7) | 16.1 (14.5 - 17.6) |
| Child Pugh - n (%) | ||
| B | 11 (37) | 13 (42) |
| C | 19 (63) | 18 (58) |
| Cirrhosis etiology - n (%) | ||
| Alcohol | 24 (80) | 19 (61) |
| Hepatitis C | 2 (7) | 5 (16) |
| Nonalcoholic steatohepatitis | 2 (7) | 6 (19) |
| Cryptogenic | 1 (3) | 1 (3) |
| Primary sclerosing cholangitis | 1 (3) | 0 (0) |
| Hepatocellular carcinoma - n (%) | 4 (13) | 8 (26) |
| Diuretic use - n (%) | 27 (90) | 27 (87) |
| Hemodialysis - n (%) | 0 (0) | 2 (6.45) |
| Hepatic encephalopathy - n (%) | ||
| None | 11 (37) | 8 (26) |
| Grade 1 - 2 or medically controlled | 19 (63) | 23 (74) |
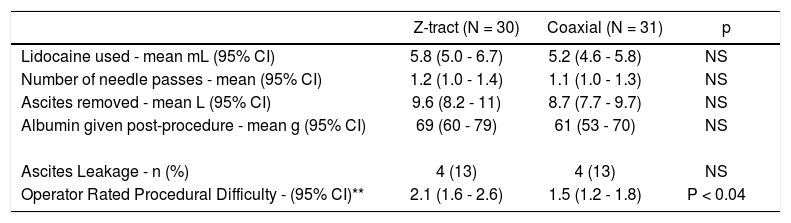
Procedural factors.
| Z-tract (N = 30) | Coaxial (N = 31) | p | |
|---|---|---|---|
| Lidocaine used - mean mL (95% CI) | 5.8 (5.0 - 6.7) | 5.2 (4.6 - 5.8) | NS |
| Number of needle passes - mean (95% CI) | 1.2 (1.0 - 1.4) | 1.1 (1.0 - 1.3) | NS |
| Ascites removed - mean L (95% CI) | 9.6 (8.2 - 11) | 8.7 (7.7 - 9.7) | NS |
| Albumin given post-procedure - mean g (95% CI) | 69 (60 - 79) | 61 (53 - 70) | NS |
| Ascites Leakage - n (%) | 4 (13) | 4 (13) | NS |
| Operator Rated Procedural Difficulty - (95% CI)** | 2.1 (1.6 - 2.6) | 1.5 (1.2 - 1.8) | P < 0.04 |
The primary endpoint of ascites leakage was equal between the groups, four paracenteses in the z-tract group (13%) and four paracenteses in the coaxial group (13%), P = 1.00. The degree of leakage reported varied. Two procedures in each group were reported as having more significant leakage requiring greater than two bandage changes. The eight paracenteses with leakage were in eight individual subjects. Four of the eight subjects with leakage were randomized in our study more than once. However, none of these subjects had leakage on subsequent or prior paracenteses. Secondary endpoints included procedural pain and operator rating of procedure difficulty. Procedural pain measured from 0 - 100 mm on a visual analog scale was significantly higher in the z-tract group [26.4 mm (95% CI 18.7 - 34.1) vs. 17.2 mm (95% CI 10.6 - 23.8) in the coaxial group, P = 0.04]. Additionally, operator rated difficulty of the overall procedure rated from 1 -5 was significantly higher in the z-tract group [2.1 (95% CI 1.6 - 2.6) vs. 1.5 (95% CI 1.2 - 1.8) in the coaxial group, P = 0.04). Analysis of the procedural pain and/or operators’ rating of procedure difficulty did not offer different findings when analyzed by operator or between methods by operator. Other complications were equally reported in both groups. These complications included post-procedural abdominal pain (3), admission within the week following paracentesis for non-procedurally related symptoms/diseases (4), and superficial bleeding (3). Of note, no significant bleeding was reported on follow-up questioning of any subjects. Aside from procedural pain and expected risks of paracentesis, no direct harm was attributed to randomization to either z-tract or coaxial insertion technique.
DiscussionWhile the exact origins of the z-tract technique are vague, to our knowledge the term first entered into the medical literature in the late 1970’s.10 It is postulated that this method was born in the era when avoidance of large volume paracentesis was advocated because it was deemed too hazardous. Since then, the z-tract has become accepted as common practice and is taught under the assumption that it will lead to less leakage of ascites following large volume paracentesis. In theory, the z-tract technique prevents alignment of the puncture sites of the peritoneum and the more superficial cutaneous tissue reducing the formation of a conduit for ascites to leak. However, this benefit has never been proven, nor has the z-tract technique ever been compared to the coaxial technique systematically. In our study, we were not able to show a difference in post-procedural ascites leakage between the two techniques. In fact, the rates of leakage were numerically equal between groups. Additionally, procedures in which the z-tract technique was utilized were reported by subjects to be more painful and by clinicians to be more difficult. To our knowledge, this is the first prospective randomized trial to compare needle insertion techniques during the now widely accepted procedure of large volume paracentesis.
There are limitations to our study. In our patient population, the reported leakage rate of ascites following para-centesis was higher than reported in prior studies (13% vs. 5%). There are a number of possible reasons for this difference including differences in procedural technique, equipment used, patient population, definition of post-procedural leakage, or unintentional incomplete drainage of ascites. In our study, the necessity to change one or more bandages after saturation by ascites was counted as leakage. Significant leakage requiring multiple (> 2) bandage changes occurred in only 4 procedures: 2 in the z-tract group and 2 in the coaxial group. The leakage rate of this subset is 6.5%, which more closely approximates prior reported leakage rates. Our procedural technique includes use of a scalpel to make an incision through the epidermis to facilitate paracentesis needle insertion. It is possible that this could facilitate leakage. Additionally, the Cald-well needle/cannula is 15 gauge which is a larger bore than some needle/cannula sets used in other studies. Of note, in a prior study comparing the Caldwell needle/cannula to an angiocath needle of similar size (14 gauge) there was no significant difference in leakage rates.11 Our results show that the rate of leakage still remained equal in both the coaxial and z-tract groups, suggesting that the needle insertion technique is not the key factor affecting leakage rate. We saw no leakage difference in the type of ascites: chy-lous vs. serous. We also excluded patients with malignant ascites and this could explain some of the leakage rate differences between our study and previously published reports. Because enrollment was stopped early due to procedural pain differences, it is possible that a type two error prevented detection of a difference in leakage rates between techniques. However, this difference would likely be small and the increased pain in the z-tract group did not justify study continuation.
Another possible criticism of this study is that some subjects were enrolled more than once. This is in part a result of the local practice allowing open access to patients needing paracentesis due to recurrent ascites who are not eligible or are awaiting other measures such as TIPS or liver transplantation. We felt that because each subject was randomized and blinded to the technique being used, this should not skew study results and may in fact strengthen the study in cases where some subjects were randomized to both techniques (7 subjects). In the seven subjects that were re-enrolled, the trend persisted for more discomfort in the procedures involving the z-tract technique regardless of which technique was used on the prior procedure.
The secondary endpoints in our study including subject pain rating and operator rating of procedure difficulty are subjective endpoints. Although these parameters were measured using validated assessment tools, the variability in both subject pain tolerance and operator skill may skew results. Additionally, while local anesthetic use was equal between groups and injected along the expected needle insertion site, the inherent challenge in reliably predicting the needle insertion tract during z-tract may account for the increased subject reported pain.
In conclusion, while the z-tract and coaxial insertion technique are both widely used during paracentesis, we found the coaxial insertion technique to be associated with less subject discomfort and easier procedure performance without any added risk of ascites leakage. The z-tract technique lacks a solid evidence based foundation and should therefore be considered a second-line technique for needle insertion during paracentesis.
AcknowledgementsWe would like to thank the fellows who performed the paracenteses: Amy Doran, Darius Jahann, Charles Orton, and Jonathan Stine; the Hepatology faculty who assisted in supervision: Neeral Shah and Curtis Argo; and our endos-copy nurse: Margie Danner-Roth. Preliminary data and other portions of this research were presented in brief abstract format at the 79th Annual Scientific Meeting of the American College of Gastroenterology in October 2014, Philadelphia, Pennsylvania, USA.
Trial RegistrationU.S. National Institutes of Health (ClincalTrials.gov) #NCT02310165, University of Virginia Institutional Review Board for Health Sciences Research #16842.
Conflict of Interest / Study Support / Other Study Information And StatementsGuarantor of the article: Patrick G. Northup, M.D.
Specific author contributions:
Shriver: Initiated and developed protocol, performed study procedures, wrote and edited manuscript.
Rudnick: Performed study procedures, enrolled patients, reviewed and edited final manuscript
Intagliata: Helped with conception of project, reviewed and edited final manuscript
Wang: Aided in manuscript composition, reviewed and edited final manuscript
Caldwell: Advised with study planning and execution, helped with project conceptualization, reviewed and edited final manuscript
Northup: Conceived project, aided with initiating and writing protocol, conceived and wrote manuscript, final editorial oversight and approval
Financial Support: There was no external financial support for this study and it was funded entirely through personal or institutional funds.
Potential Competing Interests: Dr. Caldwell receives royalties from Kimberly-Clark/Halyard for the development of the paracentesis needle-cannula and kit that is used at the institution in all paracenteses. No study funding was received from Kimberly-Clark/Halyard. None of the other authors have any potential competing interests.
The study was reviewed and approved by the University of Virginia Institutional Review Board. All involved persons (subjects) gave their informed consent (written) prior to study inclusion.
Technical appendix, statistical code, and dataset available from the corresponding author at pgn5qs@virginia.edu.