Gallbladder duplication can present a clinical challenge primarily due to difficulties with diagnosis and identification. Recognition of this anomaly and its various types is important since it can complicate a gallbladder disease or a simple hepatobiliary surgical procedure. The case report of a 63-year-old woman who presented with cholangitis and underwent a successful laparoscopic management of symptomatic gallbladder duplication is described, emphasizing several important considerations. Using ERCP, MRCP and 3D reconstructions the two cystic ducts with one common bile duct were identified. A review of the literature in referral of this variant, its anatomical classifications and significance to clinical and surgical practice is included. In conclusion, gallbladder anomalies should be anticipated in the presence of a cystic lesion reported around the gallbladder when evaluating radiologic studies. In case of surgery, preoperative diagnosis is essential to prevent possible biliary injuries or reoperation if accessory gallbladder has been overlooked during initial surgery. Laparoscopic cholecystectomy remains feasible for intervention can be safely done and awareness is necessary to avoid complications or multiple procedures.
Congenital malformations and anatomical variations of the gallbladder can present a clinical challenge due to difficulties with diagnosis and identification. They can be classified mainly as duplicated gallbladder (split-primordium) or accessory gallbladder, based on the number of associated cystic ducts and how the corresponding cystic duct connects to the common bile duct. The prevalence is relatively equal between the two genders, however due to higher occurrence of gallbladder disease in women the reported cases of duplication are higher in females than in males, 1.7:1.1,2
A duplicated gallbladder is a rarely reported diagnosis and it is also not often considered in symptomatic patients with gallbladder disease. Clinical symptoms are not different or more specific than in single gallbladder pathology and in many cases duplicated gallbladders are found intraoperative or at the time of a reoperation. With an incidence of 1 in 3800-5000 these rare congenital anatomical variants of the hepatobiliary system are considered one of the most important predisposing factors for iatrogenic bile duct injuries during cholecystectomy.
Thus, clinical consideration of a duplicated gallbladder in a symptomatic patient plays a crucial role in planning surgery and to prevent possible surgical complications and repeated laparotomies.3,4 This is a case of a patient with a gallbladder disease presented with cholangitis who was found to have a duplicated gallbladder after having been worked up.
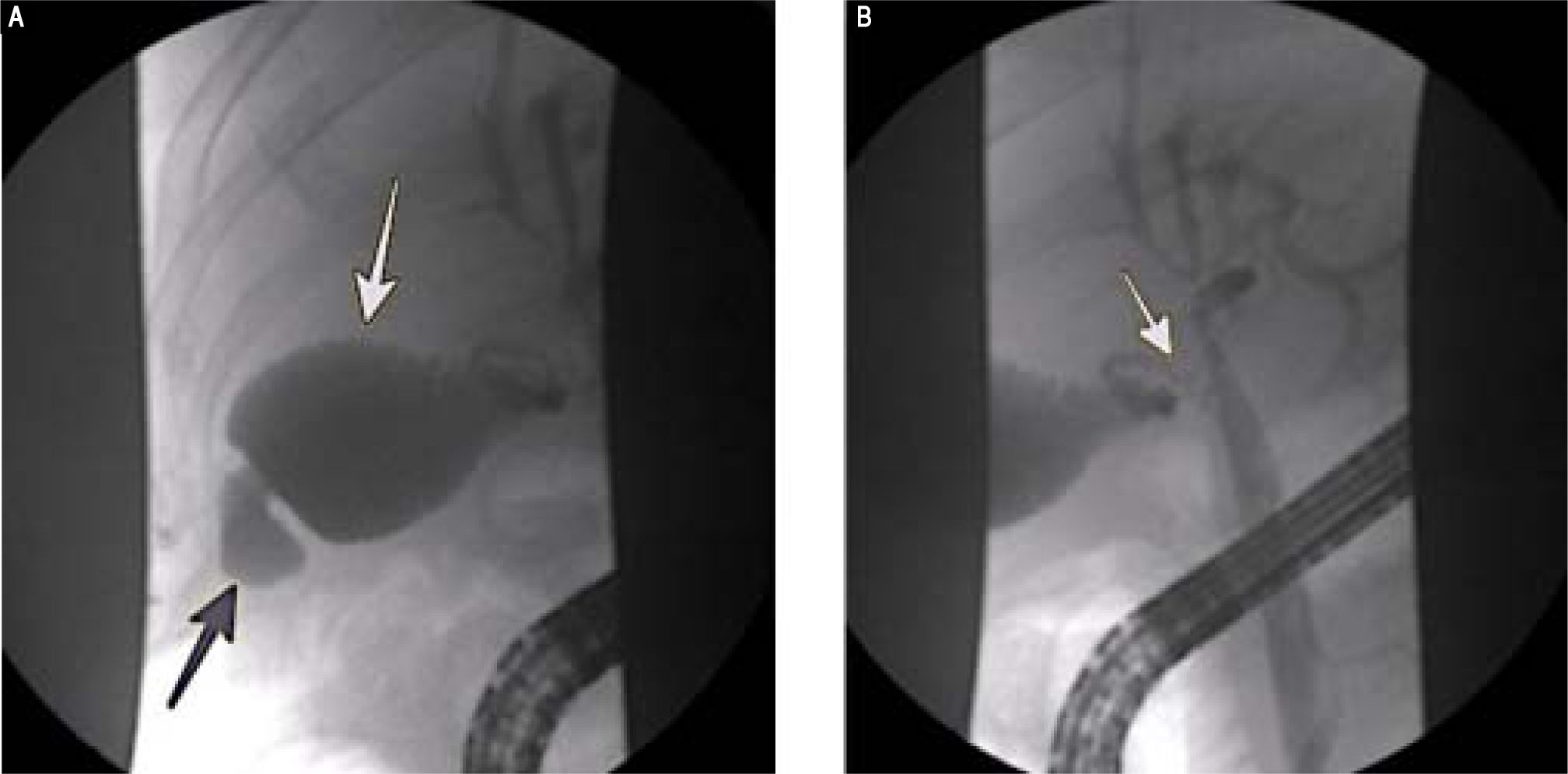
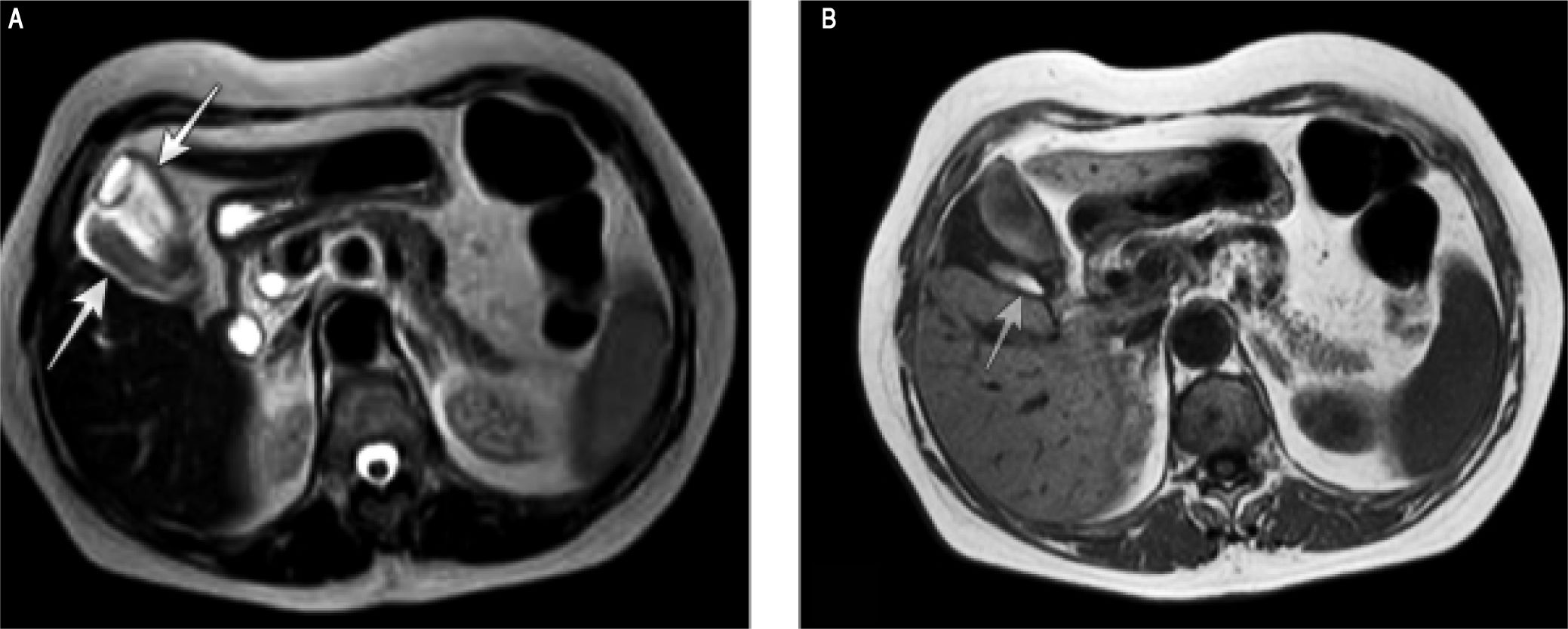
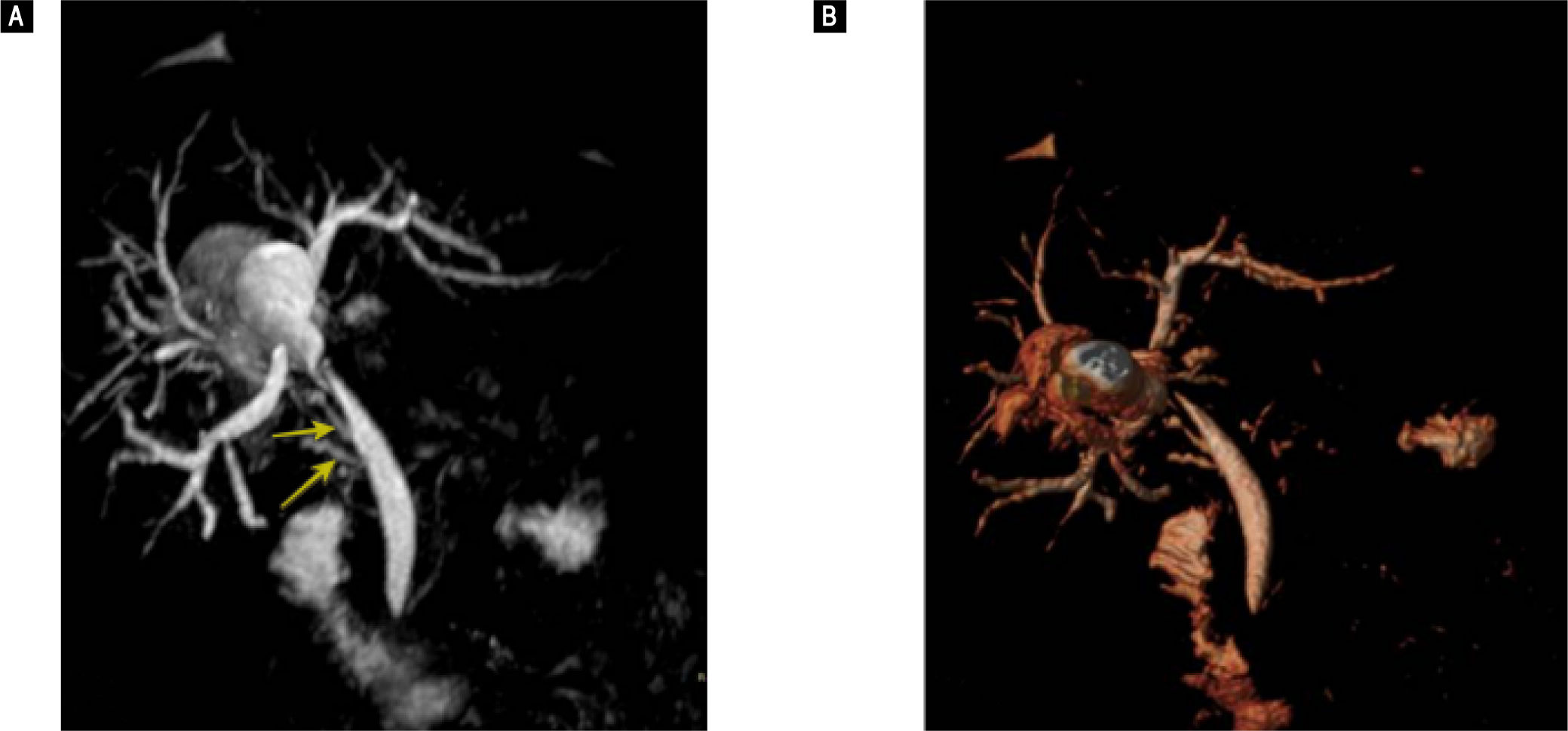
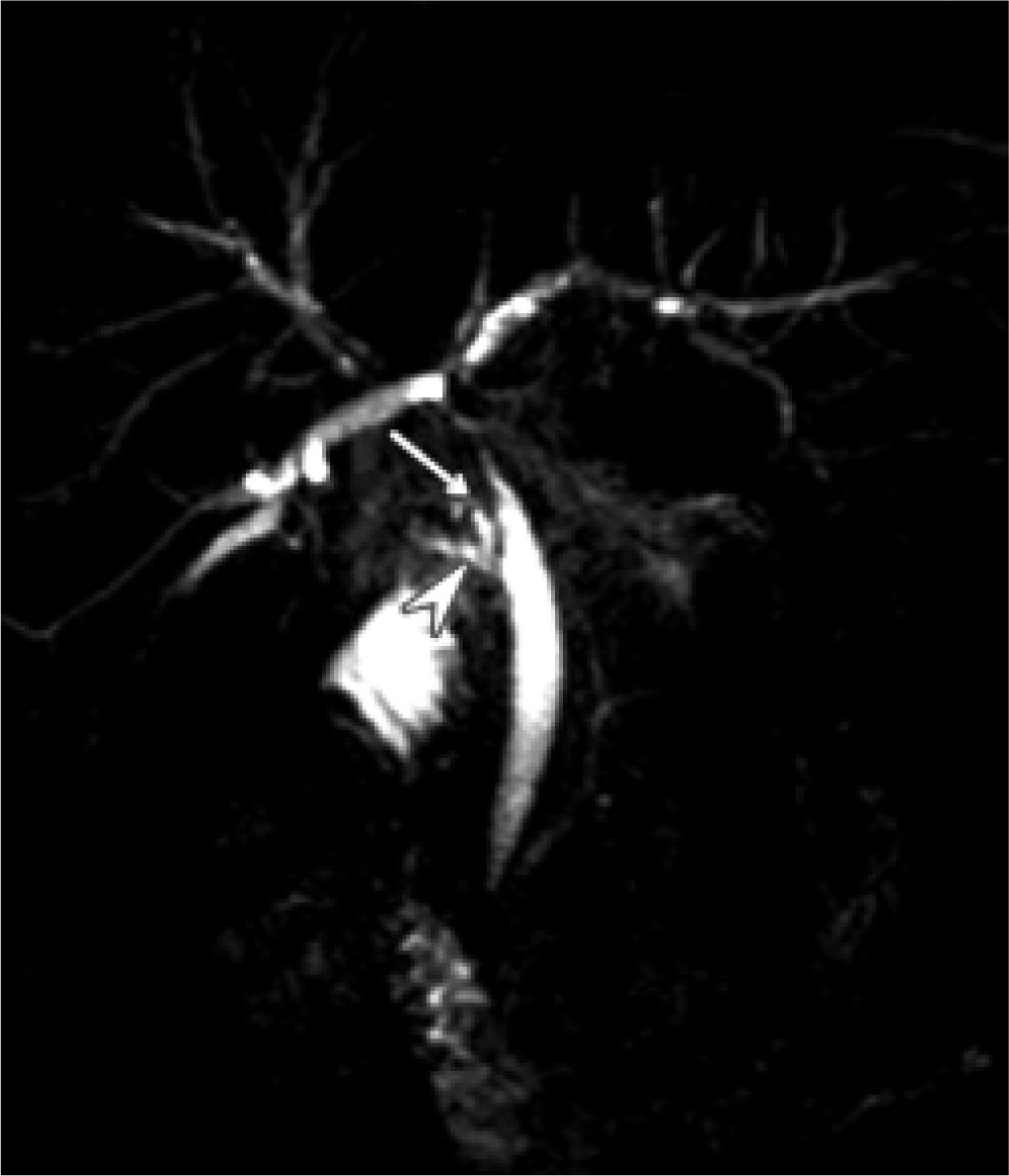
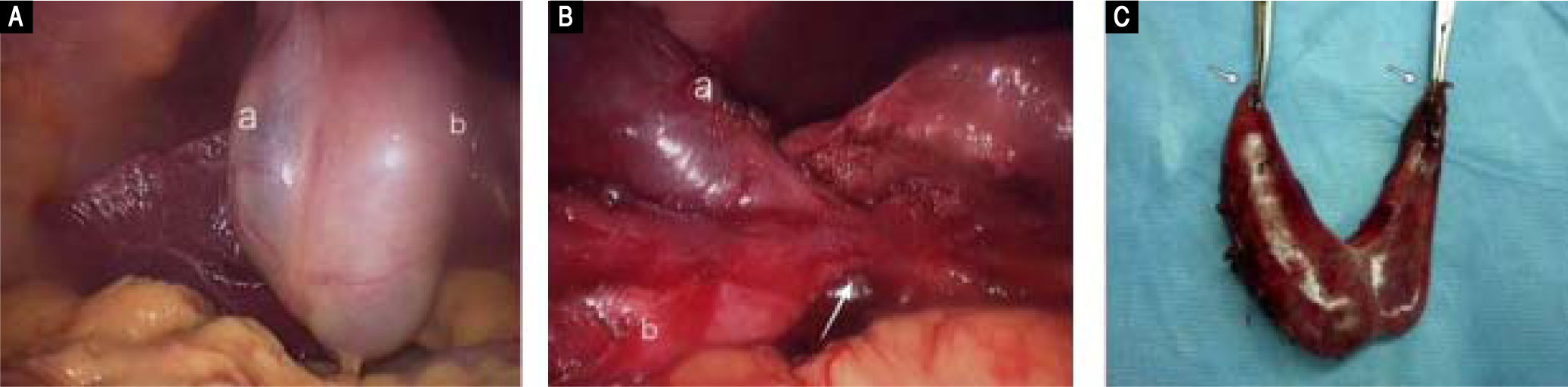
Case ReportThis case report refers to a 63-year-old Caucasian woman whose past medical history included gallbladder disease. The patient was admitted in our department presented with symptoms of acute cholangitis. Initially, she was evaluated with an abdominal ultrasound (U/S) where both chololethiasis and choledocholithiasis were found. Patient underwent ERCP (Endoscopic Retrograde Cholangio-Pancreatography) achieving common bile stone clearance. However, ERCP imaging showed an abnormality suspicious of a duplicated gallbladder (Figure 1). A focused ultrasound examination revealed two adjacent, though, separate and distinct cystic structures within the gallbladder fossa. There were ultrasound features consistent with the presence of two separate cystic ducts. However it was not clear whether they eventually fused before inserting into the common duct. She was further investigated with an MRI (magnetic resonance imaging) and MRCP (Magnetic Resonance Cholangio-Pancreatography). The MRI revealed two pear-shaped structures in the gallbladder fossa with wall thickening and pericholecystic fluid indicating inflammation (Figure 2). The MRCP showed separated cystic ducts that joined together in a main cystic duct (single “common” cystic duct), just before the later joined the common bile duct (Figure 3 and Figure 4). A diagnosis of duplicated gallbladder was consequently made and the patient was scheduled for laparoscopic cholecystectomy. Intraoperative a duplication of the gallbladder was confirmed as a Y-shaped type (vesica fellea duplex) with two cystic ducts joining into a common cystic duct clearly identified before entering the bile duct and a single cystic artery. Both gallbladders lying in the gallbladder fossa was successfully removed laparoscopically (Figure 5). Pathology report confirmed the presence of two gallbladders with features of chronic cholecystitis and adenomyomatosis. The patient had an uneventful recovery and she was discharged home on the 2nd postoperative day.
Axial single-shot fast SE T2-weighted MR image and, B. Axial T1-weighted MR image shows two pear-shaped structures in the gallbladder fossa (arrows). The posterior structure (arrow) has low T2 signal intensity and high T1 signal intensity due to dependent material within the gallbladder lumen. There is wall thickening andpericholecystic fluid indicating inflammation.
Three-dimensional MR cholangiopancreatogram shows a separated cystic duct (arrow) that joins together with the main cystic duct (arrowhead) to become a shared, single “common” cystic duct just before the later joins the common bile duct; indicative of Y-shaped subtype I duplicated gallbladder.
Congenital malformations of the gallbladder have been categorized into morphological and positional abnormalities including malformation, deformation, multiple gallbladder, ectopias, intrahepatic position and heterotopic mucosa. Gallbladder duplication is a morphological abnormality.5 It is considered to result from the incorrect differentiation or excessive division of embryonic organs during the 5th and 6th gestational week, when the caudal bud of the hepatic diverticulum splits into separate buds or outpunching’s. The later the single primordium bifurcates, the less complete is the resulting duplication of the gallbladder. As a result, a true duplication of gallbladder takes place earlier in the gestation and involves the existence of an accessory gallbladder and two distinct cystic ducts. The accurate incidence of duplicated gallbladders is difficult to calculate because only symptomatic cases or incidental surgical, radiological and cadaveric findings are registered.2 The first reported human case was noted in a sacrificial victim of Emperor Augustus in 31 BC. Sherren, reported the first documented case of double accessory gallbladder in a living human in 1911.6
Several authors have classified the anatomical variations of duplicated gallbladders. Classification is based on their relation to the cystic duct and mainly is classified into two major groups, as a duplicated (split-primordium) or as an accessory gallbladder, according to the presence or absence of a common cystic duct respectively. Accessory gallbladders are characterized by separate cystic ducts entering the biliary tree and arise from two or more separate cystic primordia forming. The most widely accepted classification for double gallbladder is the Boyden’s classification.5 Boyden was first to describe the duplicate gallbladder and its variable anatomy in 1926. Based on their relation to the cystic duct, he described “vesica fellea divisa”, (bilobed gallbladder which is drained by a sole cystic duct), and “vesica fellea duplex” (true gallbladder duplication). The latter is sub classified into “Y-shaped type” (two cystic ducts uniting before entering the common bile duct), and “H-shaped or ductular type” (two cystic ducts enter separately into the common bile duct). In 1936, Gross also described congenital abnormalities of gallbladder and classified them into six types labeled A-F. He also stated that a bilobed gallbladder is an anomaly, but not a true duplication.7 In 1977, Harlaftis, et al. further modified the classification by describing two main types based on morphology and embryogenesis.8 In type 1 (split primordium), the duplicate gallbladders have a single cystic duct that enters the common bile duct and is further subdivided into septated, V shaped, or Y shaped. In type 2 (dual primordium), the accessory gallbladders have two or more cystic ducts drain independently into the biliary tree. The organ more proximal to the liver is regarded as the accessory one. This type is subdivided into ductular gallbladder (H type) and trabecular gallbladder. In the ductular type the accessory cystic duct connects to the common bile duct. In the trabecular type the accessory cystic duct connects to the left or right hepatic duct. Finally, Harlaftis type III includes any anatomical variation that cannot be classified in either of the two-aforementioned categories. The most common variant found in the literature (48.6% of cases), is the H or ductular type 2 variant, where there are two separate gallbladders and the cystic and accessory cystic ducts enter the common bile duct separately.
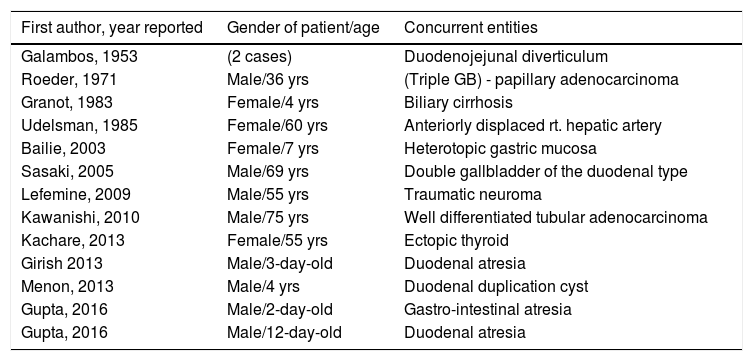
While gallbladder duplication is typically associated with gallstones and cholecystitis, there are sporadic reports in the literature of other anomalies and diseases, which have been presented with this entity.2 Concurrent entities that have been reported alongside a duplicated gallbladder are presented in table 1. In addition to double gallbladders there have been cases of triple gallbladders reported in the literature.9-11
Cases of duplicated gallbladder associated with other entities.
| First author, year reported | Gender of patient/age | Concurrent entities |
|---|---|---|
| Galambos, 1953 | (2 cases) | Duodenojejunal diverticulum |
| Roeder, 1971 | Male/36 yrs | (Triple GB) - papillary adenocarcinoma |
| Granot, 1983 | Female/4 yrs | Biliary cirrhosis |
| Udelsman, 1985 | Female/60 yrs | Anteriorly displaced rt. hepatic artery |
| Bailie, 2003 | Female/7 yrs | Heterotopic gastric mucosa |
| Sasaki, 2005 | Male/69 yrs | Double gallbladder of the duodenal type |
| Lefemine, 2009 | Male/55 yrs | Traumatic neuroma |
| Kawanishi, 2010 | Male/75 yrs | Well differentiated tubular adenocarcinoma |
| Kachare, 2013 | Female/55 yrs | Ectopic thyroid |
| Girish 2013 | Male/3-day-old | Duodenal atresia |
| Menon, 2013 | Male/4 yrs | Duodenal duplication cyst |
| Gupta, 2016 | Male/2-day-old | Gastro-intestinal atresia |
| Gupta, 2016 | Male/12-day-old | Duodenal atresia |
There are no specific symptoms or signs associated with duplicate gallbladders. Higher frequency of pathology (malignant or not) in a duplicated gallbladder comparing to a single gallbladder has not been confirmed. Patients present atypical symptoms for biliary disease or the common pathologies that can occur as a normal, single gallbladder, including acute cholecystitis, cholelithiasis, empyema, torsion, cholecystocolic fistula, lump in the abdomen.12 Since the most common imaging modality for biliary disease is operator dependent, (i.e. ultrasound), this disease entity can be misdiagnosed. As a result, many cases will proceed to cholecystectomy without the presence of a double gallbladder being considered. Many clinical studies, however, have demonstrated that congenital anomalies of the gallbladder are associated with an increased risk of complications postoperative and repeated surgery.13 If symptoms appear post cholecystectomy, the clinician has to include a possibly duplicated gallbladder in his diagnostic algorithm, in case a missed second gallbladder has remained inside the abdomen.
Therefore, defining ductal anatomy is important to appreciate these anatomic variations of the biliary system and imaging plays a fundamental role in the clinical evaluation for gallstone disease. However, none of the imaging modalities is sensitive enough, in view of the fact that successful imaging diagnosis is noted in slightly more than half of the cases. Abdominal ultrasound (US) is often the first-line imaging modality used in the assessment of a patient with gallbladder disease; however does not always allow a precise diagnosis of gallbladder malformations. Even though it can identify a duplicate gallbladder in the presence of two cystic structures occupying the gallbladder fossa, US is not accurate enough to depict properly the anatomy of the cystic duct(s) and to exclude a wide range of alternative diagnoses.12 The most common entities that may imitate a duplicate gallbladder on US examination are a choledochal cyst, gallbladder diverticulum and a phrygian cap. In a review study of 17 cases reports, abdominal ultrasound confirmed duplicate gallbladder in only 3 cases.14
ERCP can provide a detailed imaging of ductal anatomy, however it is invasive and carries a risk of serious complications and is not commonly used as a diagnostic tool. In addition, it may not be indicated in every case of cholelithiasis or cholecystitis. Apparently in our patient ERCP management was imperative as the patient presented with cholangitis. In our case, ERCP showed the gallbladder and a second pear shaped cystic formation filled with contrast, through one common cystic duct. Accordingly, a high index suspicion was maintained for the diagnosis of a duplicate gallbladder. In such cases, while ERCP is reserved for therapeutic indications, an incidental diagnosis of gallbladder malformations can be made.
As a result, MRCP is becoming the initial imaging tool for the biliary tract imaging in case of suspected gallbladder duplication during the preoperative managing.1 However, although MRCP and 3D reconstructions may be able to evaluate ductal anatomy without the use of radiation, CT cholangiography should be used where there are any contraindications to MRCP or where it is unable to identify adequately the biliary anatomy.12 In a study of potential living liver donors, CT cholangiography allowed the visualization of at least the second level branches of the intrahepatic biliary tree in all patients (up to the fourth level in some patients), whereas MRCP only reliably displayed the intrahepatic biliary anatomy up to the bifurcation of the common hepatic duct.15
Surgery should be the treatment of choice only in symptomatic patients. Surgery is not indicated when duplicated gallbladders are discovered incidentally and prophylactic cholecystectomy in an asymptomatic patient with gallbladder duplication is not recommended. Yet, it is recommended to remove both gallbladders in symptomatic patients at one stage to prevent subsequent disease in the remnant gallbladder and repeated surgical procedures. There has been an emphasis on the need for open cholecystectomy to identify and manage the different types of gallbladder duplication in the literature.13 On the other hand, with the advent of newer imaging modalities and expertise, these rare anomalies can be diagnosed preoperatively and can be successfully treated by laparoscopy with minimal morbidity. Laparoscopic cholecystectomy is the mainstay of treatment, and has been successfully utilized, as it can be found in literature with the first of these procedures reported by Garcia, et al. in 1993.16,17 A recent review identified 3 out of 13 laparo-scopically managed cases that require conversion to an open cholecystectomy.3 An important issue performing a laparoscopic procedure is whether and when the procedure should be converted to an open cholecystectomy. This is a judgment call dependent on the experience of the surgeon and the degree of difficulty and suspicion of anatomical variations face during surgery after a fine landmark dissection. In an uncertain situation intraoperative cholangiography and inspection of the gallbladder specimen is indicated to properly evaluate the anatomy and the necessity for further actions.18,19
ConclusionIn conclusion, a duplicated gallbladder should be an additional consideration when typical gallbladder disease symptoms are present under certain circumstances while uncharacteristic imaging is found, and further diagnostic imaging is important. Clinicians have to consider these entities and anatomic variations when evaluating patients with biliary disease, in order to avoid unnecessary biliary injury in case of surgical treatment. Total laparoscopic removal can be performed safely; however these cases probably do better in the hand of an experienced laparoscopic surgeon or a hepatobiliary surgeon.
Abbreviations- •
ERCP: endoscopic retrograde cholangio-pancreatography.
- •
MRI: magnetic resonance imaging.
- •
MRCP: magnetic resonance cholangio-pancreatography.
The authors declares that there is no conflict of interest regarding the publication of this article.