In patients with high-risk localized prostate cancer (HRPCa), multimodal treatment plays a fundamental role.
ObjectiveTo compare relapse-free survival (RFS) in patients with HRPCa, treated primarily with radiotherapy (RT)+hormone therapy (HT) versus radical prostatectomy (RP) and salvage RT (sRT)±HT when biochemical recurrence (BCR) appears.
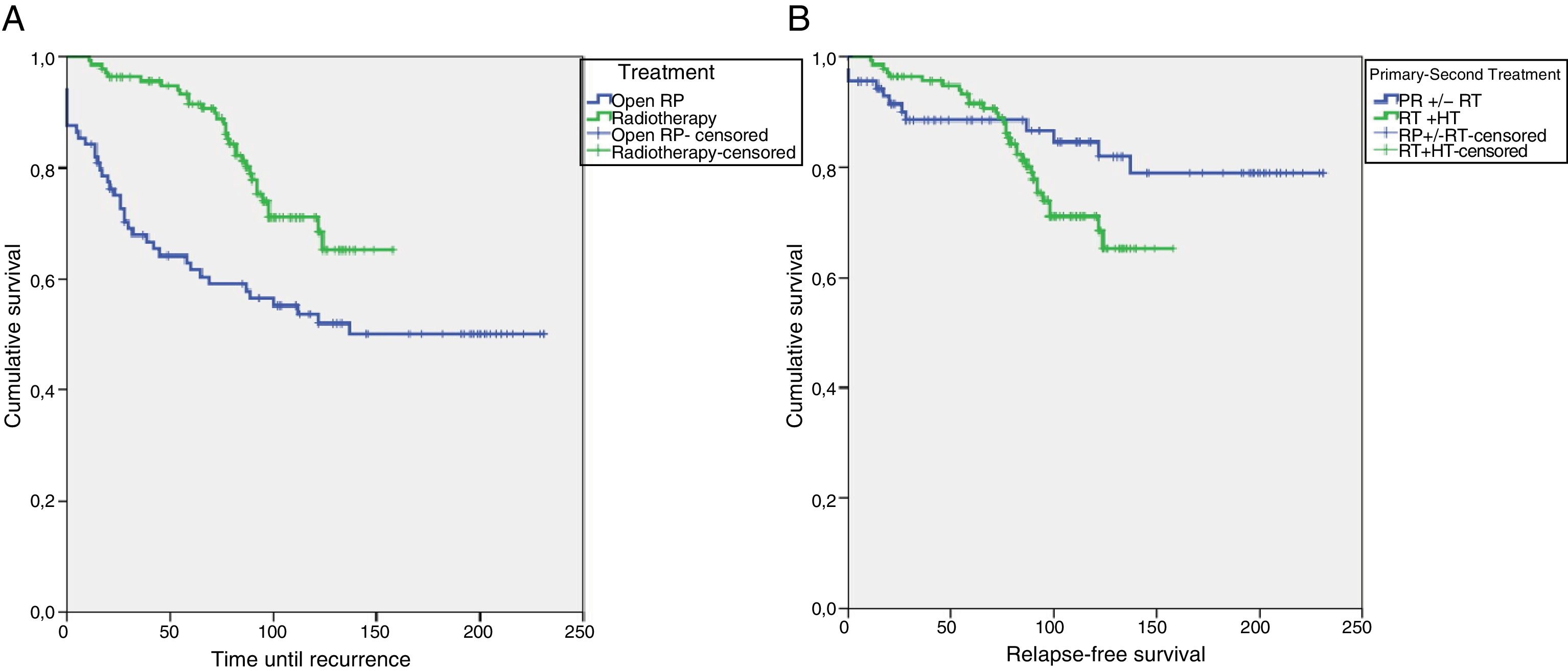
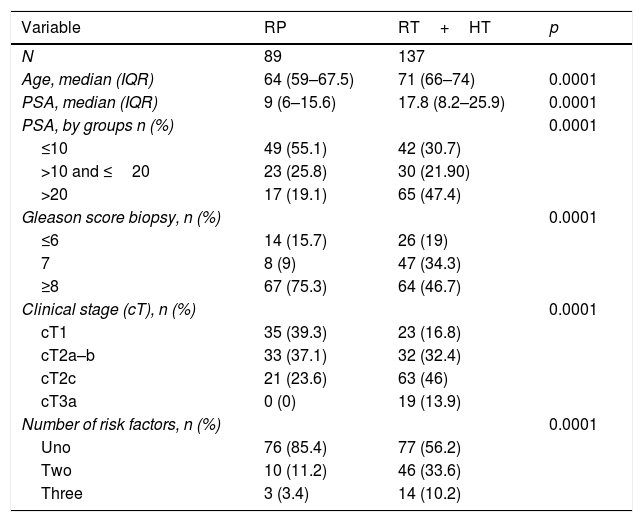
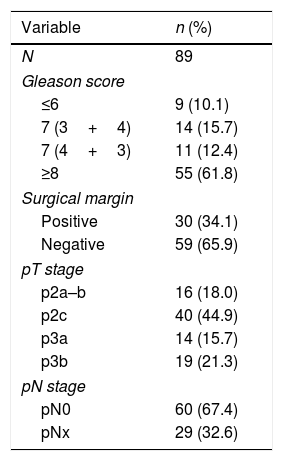
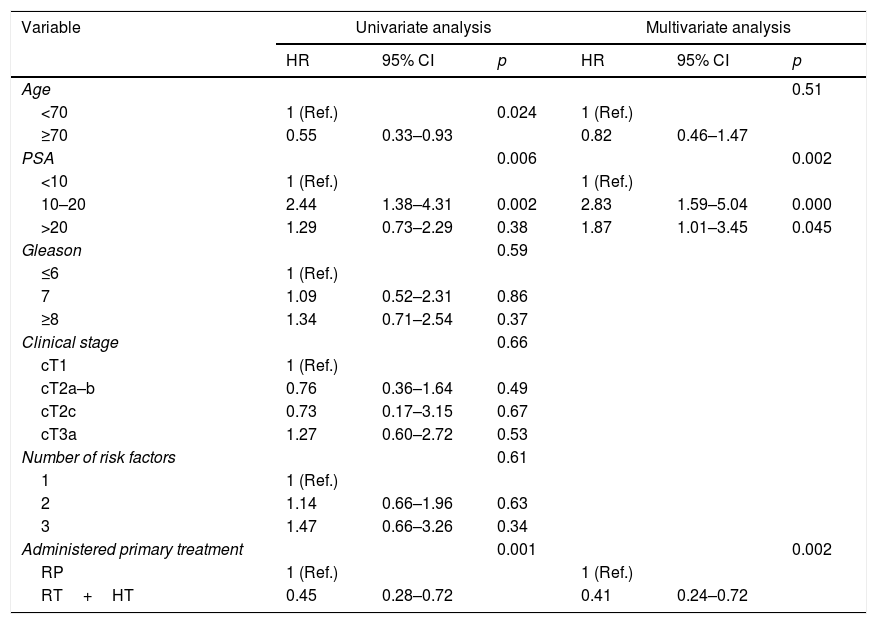
Material and methodsRetrospective analysis of 226 patients with HRPCa (1996–2008), treated primarily with RT+HT (n=137) or RP (n=89). The Kaplan–Meier method has been used to evaluate survival and the log-rank test has been used to evaluate the contrast between the different categories of the variables. Multivariate analysis has been performed using Cox regression to determine variables with an impact on RFS with statistical significance (p<0.05).
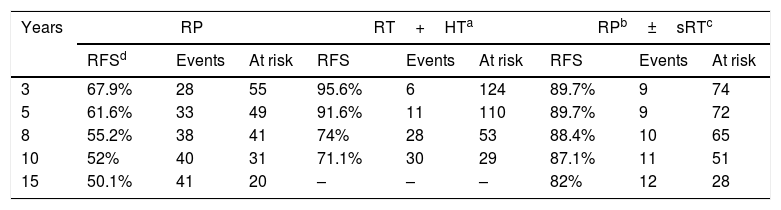
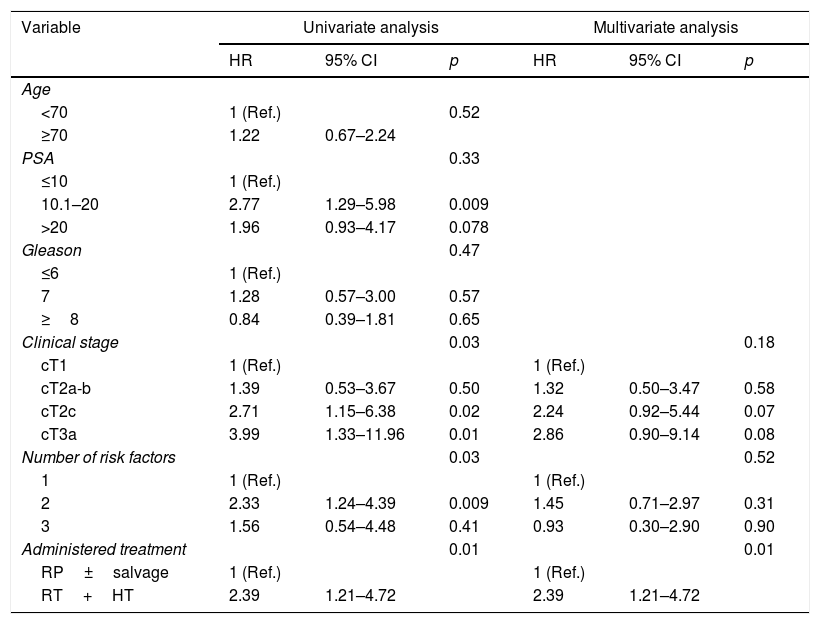
ResultsThe median follow-up of the series was 111 (IQR 85–137.5) months. After RT+HT, 32 (23.4%) patients relapsed, and after RP 41 (46.1%) cases, (p=0.0001). When comparing the primary treatments, the RFS at 5 and 10 years was higher after RT+HT versus RP in monotherapy (p=0.001). The primary treatment with RT+HT reduced the risk of BCR when compared to the RP (HR=0.41, p=0.002). The estimation of the RFS at 5 and 10 years after RP+sRT±HT was 89.7 and 87.1%, while after primary RT+HT was 91.6 and 71.1%, respectively (p=0.01). The only factor that behaved as an independent predictor of RFS was the multimodal treatment with RP+sRT±HT when BCR showed up (HR=2.39, p=0.01).
ConclusionIn HRPCa, multimodal treatment with RP+sRT±HT if BCR, significantly improves RFS with respect to treatment with RT+HT.
En pacientes con cáncer de próstata localizado de alto riesgo (CPAR) el tratamiento multimodal juega un papel fundamental.
ObjetivoComparar la supervivencia libre de recidiva (SLR) en pacientes con CPAR tratados de forma primaria con radioterapia (RT)+hormonoterapia (HT) frente a prostatectomía radical (PR) rescatados con RT de rescate (RTR) con o sin HT tras recidiva bioquímica (RB).
Material y métodosAnálisis retrospectivo de 226 pacientes con CPAR (1996-2008), tratados de forma primaria con RT+HT (n=137) o PR (n=89). Utilizamos el método de Kaplan-Meier para evaluar la supervivencia y el test de log-rank para evaluar las diferencias entre las distintas categorías de las variables. Se realiza análisis multivariante mediante regresión de Cox para determinar variables con impacto en la SLR con significación estadística (p<0,05).
ResultadosLa mediana de seguimiento de la serie fue de 111 (RIC 85-137,5) meses. Tras RT+HT recidivaron 32 (23,4%) pacientes, y 41 (46,1%) tras PR (p=0,0001). Al comparar los tratamientos primarios, la SLR a los 5 y 10 años fue mayor tras RT+HT frente a PR en monoterapia (p=0,001). El tratamiento primario con RT+HT redujo a más de la mitad el riesgo de RB al compararse con la PR (HR=0,41, p=0,002). La estimación de la SLR a los 5 y 10 años después de PR+RTR±HT fue de 89,7 y 87,1%, mientras que tras RT+HT primaria fue de 91,6 y 71,1%, respectivamente (p=0,01). El único factor que se comportó como predictor independiente de SLR fue el tratamiento multimodal mediante PR+RTR±HT cuando se presentó la RB (HR=2,39, p=0,01).
ConclusiónEn CPAR el tratamiento multimodal con PR+RTR±HT si RB mejora significativamente la SLR con respecto al tratamiento con RT+HT.