Vertigo and dizziness as symptoms are frequent in the population. They are present in a wide range of pathologies and it is usually difficult to make an accurate diagnosis. The general objective of this study is to obtain the information to evaluate vertigo and dizziness in the hospital setting. The specific objectives are: to estimate the burden of these symptoms at the hospital; to study patients’ conditions and to detail the flow of these patients inside the hospital.
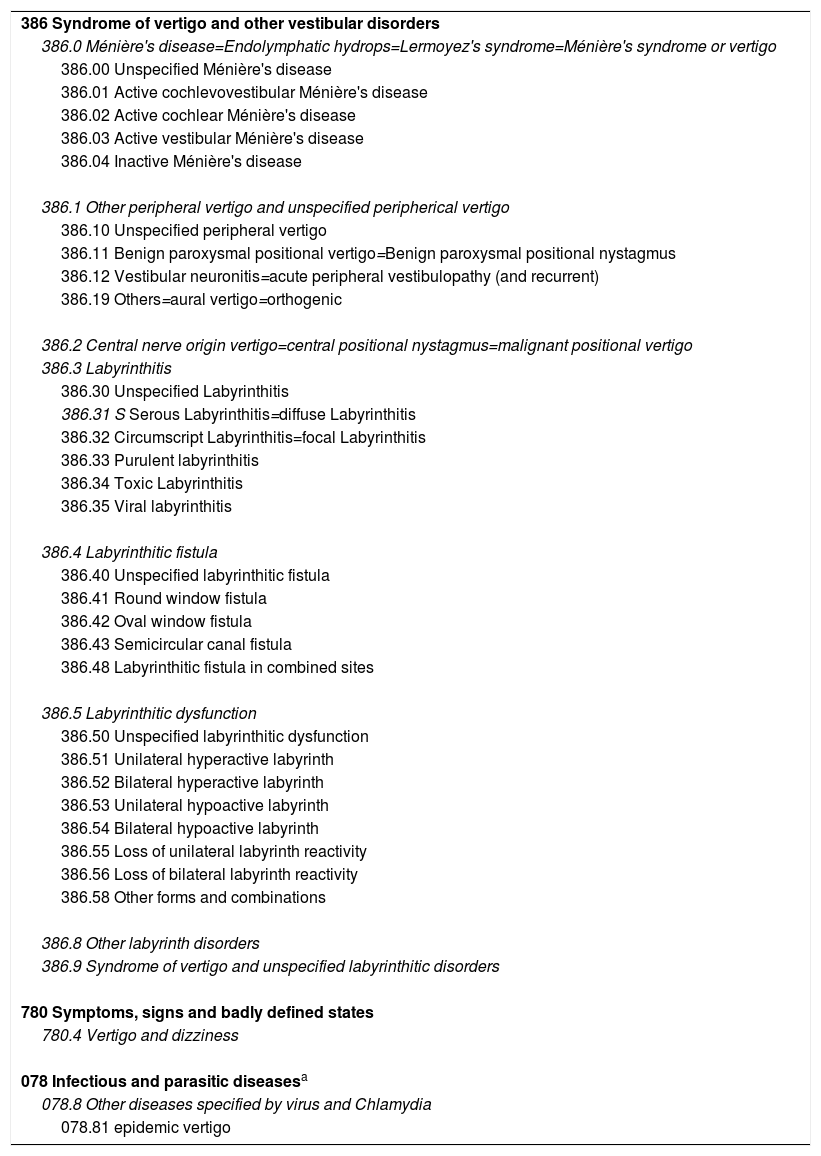
MethodsObservational descriptive study. We made a search of the referral proposals made in 2011 and 2012 to the hospital because of vertigo symptoms. The patients’ demographic and clinical characteristics, and the administrative details of the referrals were analysed.
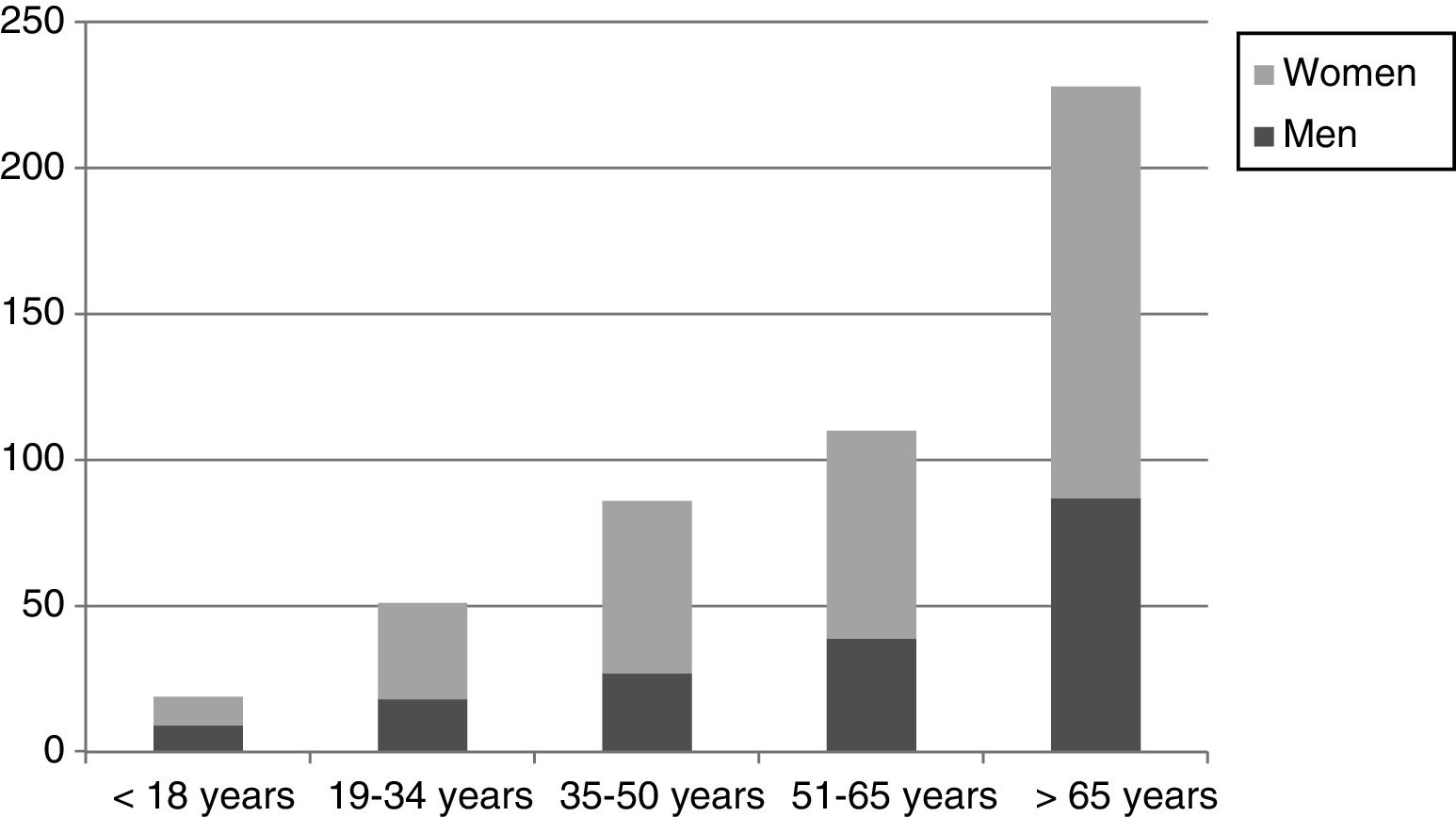
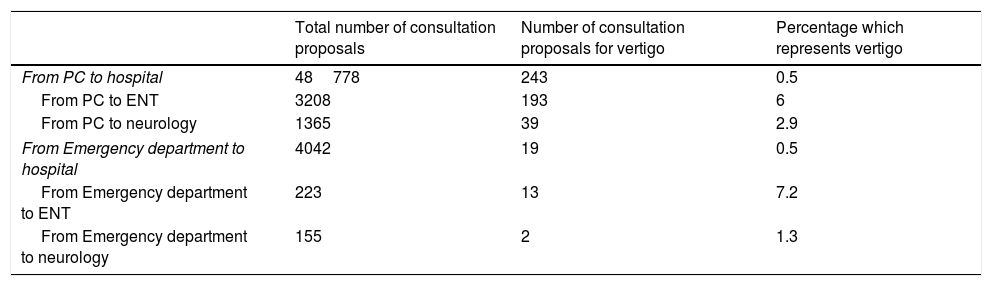
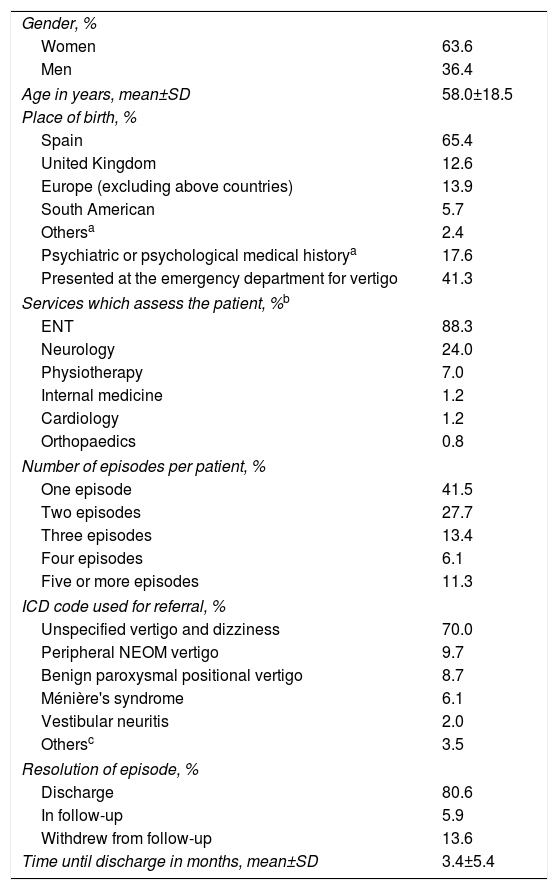
ResultsA total of 558 proposals were analysed corresponding to 494 patients. Vertigo accounted for 0.5% of all referrals made from Primary Care to the hospital. Sixty-three percent of the sample were women; the average age was 58 years. Eighty-eight percent of the patients were evaluated by Otorhinolaryngology, 24% by Neurology. Thirty point eight percent consulted on 3 or more occasions for the symptom. Sixteen percent were assessed for psychiatric conditions in the hospital.
ConclusionsVertigo as a symptom is a significant burden in the hospital setting. The patients who suffer it consult on several occasions and are assessed by different specialties. This implies in some cases an excessive and ineffective flow of patients. In our setting, otorhinolaryngology is the main department to treat vertigo and dizziness patients.
Los síntomas de vértigo y mareo son frecuentes en la población, se presentan como manifestación de un amplio abanico de enfermedades y habitualmente es difícil realizar un diagnóstico de certeza. El objetivo general de este estudio es obtener la información para evaluar estos síntomas en el entorno hospitalario. Los objetivos específicos son: estimar el peso global que representan estos síntomas en las derivaciones al hospital; conocer las características de los pacientes derivados y detallar el flujo de las consultas.
MétodosEstudio descriptivo observacional. Se buscaron las propuestas de consulta realizadas en 2011 y 2012 al hospital por el síntoma de vértigo. Se analizaron características demográficas y clínicas de los pacientes, y administrativas de las derivaciones.
ResultadosSe analizaron un total de 558 propuestas correspondientes a 494 pacientes. El vértigo supuso el 0,5% del total de las derivaciones realizadas desde Atención Primaria al hospital. El 63% de la muestra han sido mujeres, con una edad media de 58 años. El 88% de los pacientes fue valorado por Otorrinolaringología y el 24% por Neurología. Un 30,8% consultó en 3 o más ocasiones por el síntoma. El 16% fue valorado por enfermedad psiquiátrica en el hospital.
ConclusionesEl vértigo como síntoma supone una carga significativa en el ámbito hospitalario. Los pacientes que lo presentan consultan en múltiples ocasiones y son valorados en distintas especialidades. En ciertos casos, el flujo de pacientes puede resultar excesivamente dinámico e ineficaz. En nuestro entorno, Otorrinolaringología es el principal receptor de pacientes con síntomas de vértigo y mareo.