There has been a very significant increase in the use of minimally invasive surgery has in the last decade. In order to provide a common language after transoral surgery of the oropharynx, a system for classifying resections has been created in this area, regardless of the instrumentation used.
MethodsFrom the Oncology Working Group of the Catalan Society of Otorhinolaryngology, a proposal for classification based on a topographical division of the different areas of the oropharynx is presented, as also based on the invasion of the related structures according to the anatomical routes of extension of these tumours.
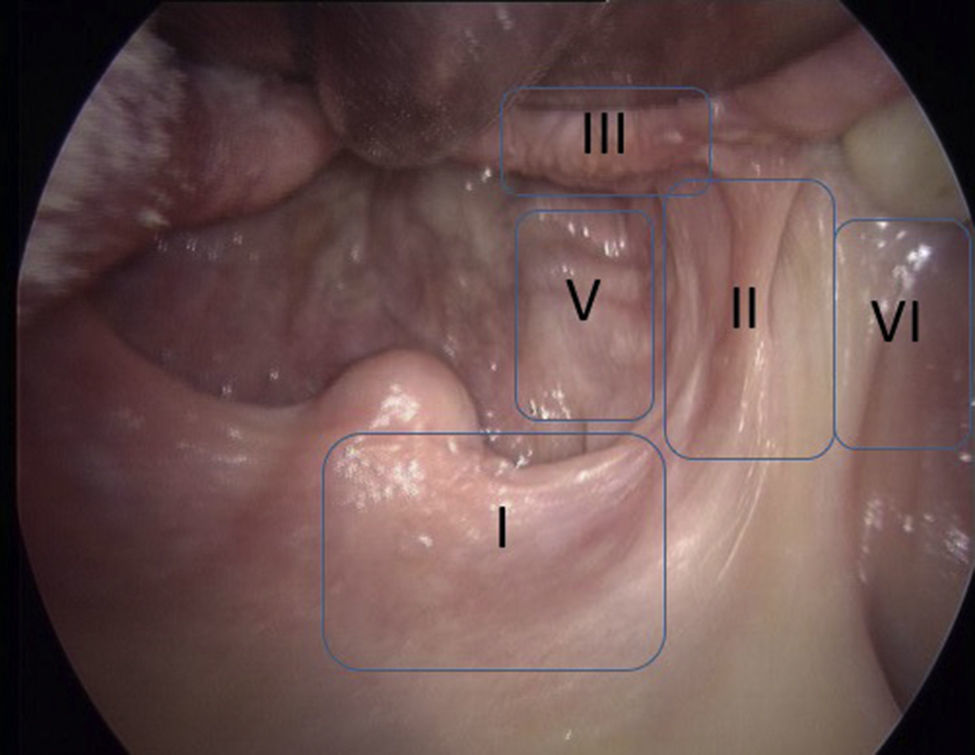
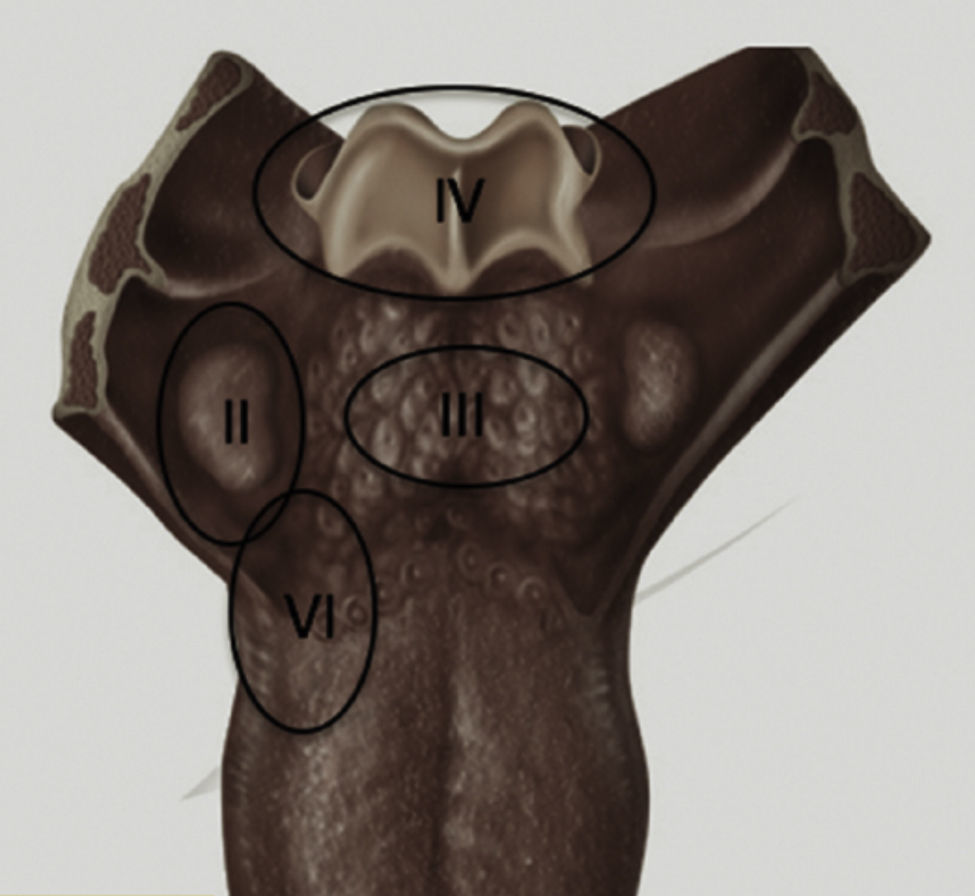
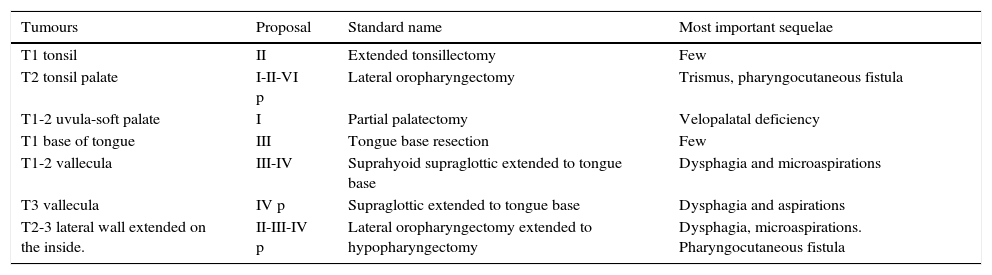
ResultsThe classification starts using the letter D or I according to laterality either right (D) or left (I). The number of the resected area is then placed. This numbering defines the zones beginning at the cranial level where area I would be the soft palate, lateral area II in the tonsillar area, area III in the tongue base, area IV in the glossoepiglottic folds, epiglottis and pharyngoepiglottic folds, area V posterior oropharyngeal wall and VI the retromolar trigone.
The suffix p is added if the resection deeply affects the submucosal plane of the compromised area. The different proposed areas would, in theory, have different functional implications.
ConclusionProposal for a system of classification by area to define different types of transoral surgery of the oropharynx, and enable as sharing of results and helps in teaching this type of technique.
La cirugía mínimamente invasiva ha presentado una expansión muy importante en la última década. Con el objetivo de aportar un lenguaje común tras cirugía transoral de la orofaringe, se ha creado un sistema de clasificación de las resecciones en esta zona, independientemente de la instrumentalización utilizada.
MétodosDesde el Grupo de Trabajo en Oncología de la Sociedad Catalana de Otorrinolaringología, se presenta una propuesta de clasificación basada en una división topográfica de las diferentes zonas de la orofaringe, así como en la afectación de las estructuras anexas según las vías anatómicas de extensión de estos tumores.
ResultadosLa clasificación se inicia utilizando la letra D o I según la lateralidad sea derecha (D) o izquierda (I). A continuación se coloca el número del área resecada. Esta numeración define las zonas iniciando a nivel craneal donde el área I sería el paladar blando, el área II lateral en la zona amigdalina, el área III en la base de lengua, el área IV en los repliegues glosoepiglóticos, la epiglotis y repliegues faringoepiglóticos, el área V pared orofaríngea posterior y VI el trígono retromolar.
Se añade el sufijo p si la resección afecta profundamente al plano submucoso de la zona comprometida. Las diferentes áreas propuestas tendrían, de una forma teórica, diferentes implicaciones funcionales.
ConclusionesPropuesta de sistema de clasificación por áreas que permite definir diferentes tipos de cirugía transoral de la orofaringe así como compartir los resultados y ayudar en la docencia de este tipo de técnicas.