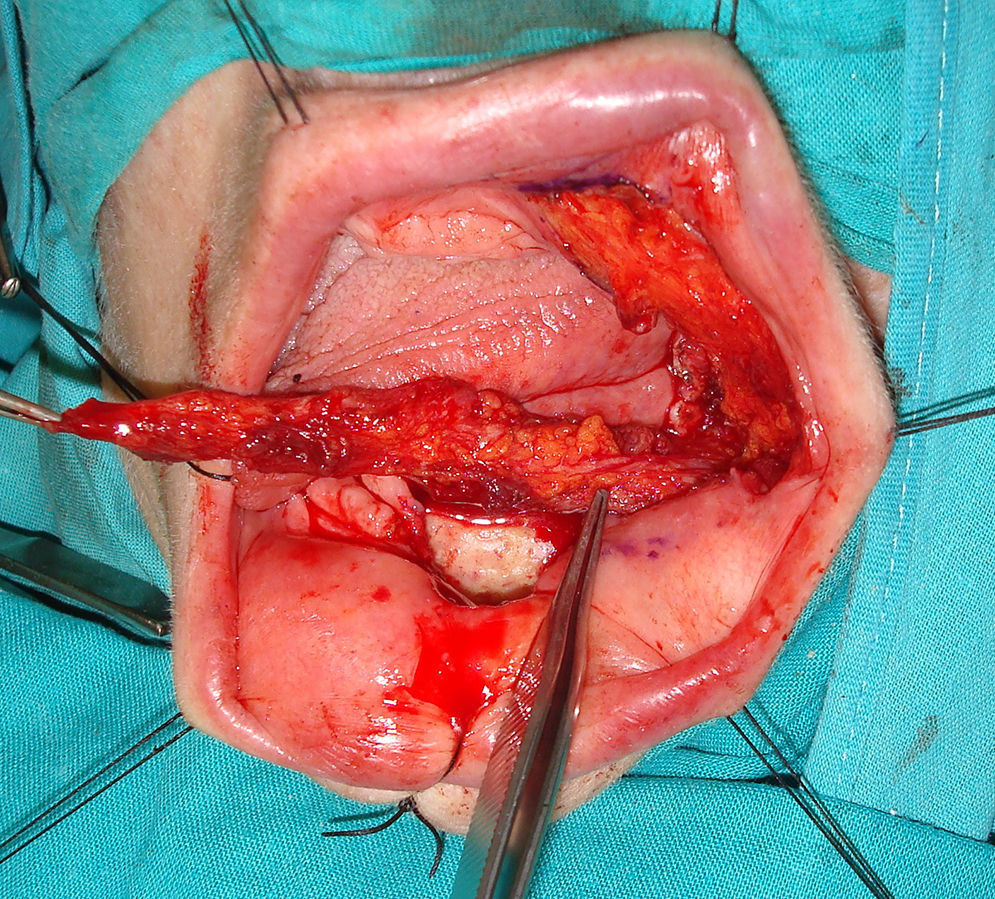
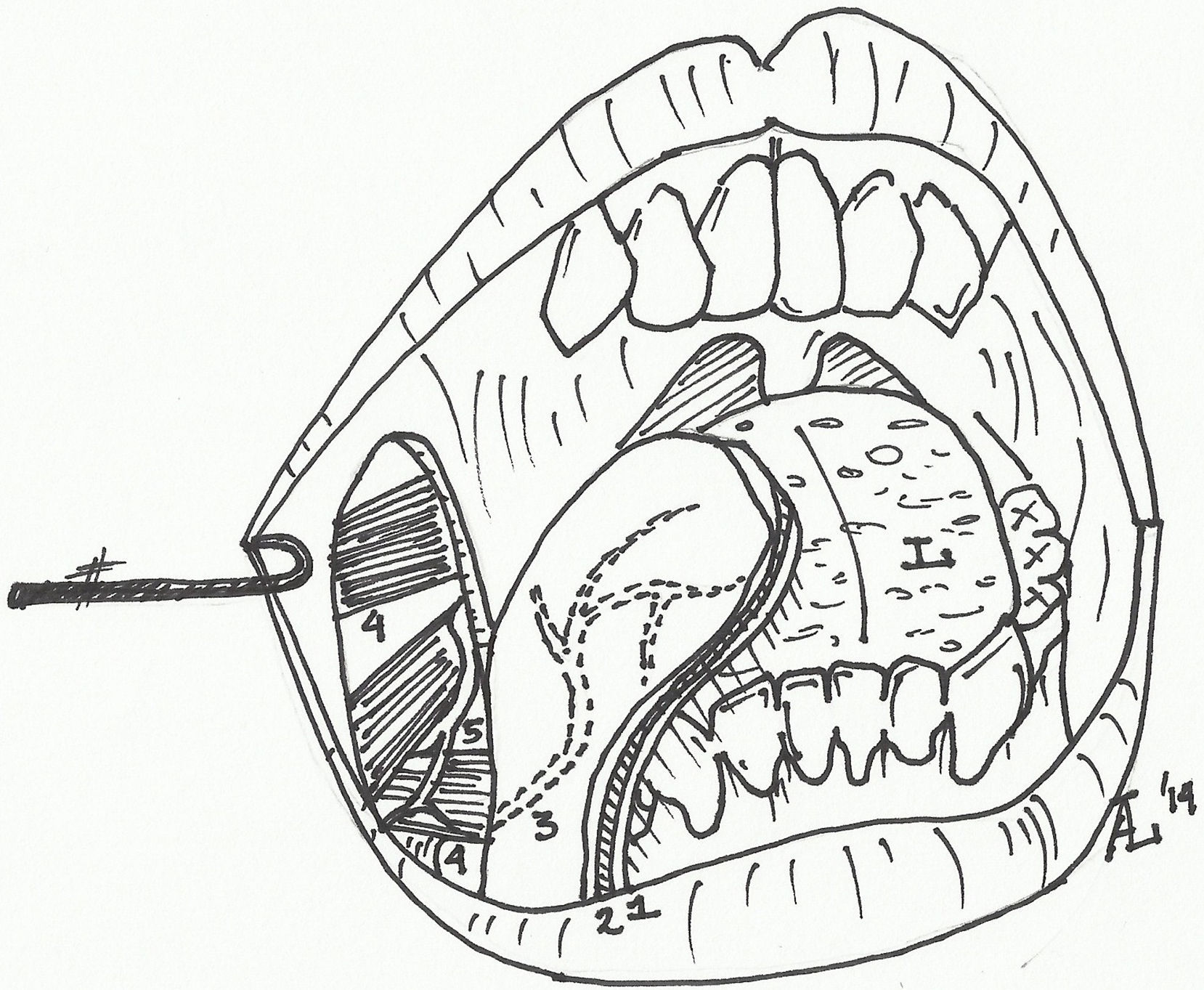
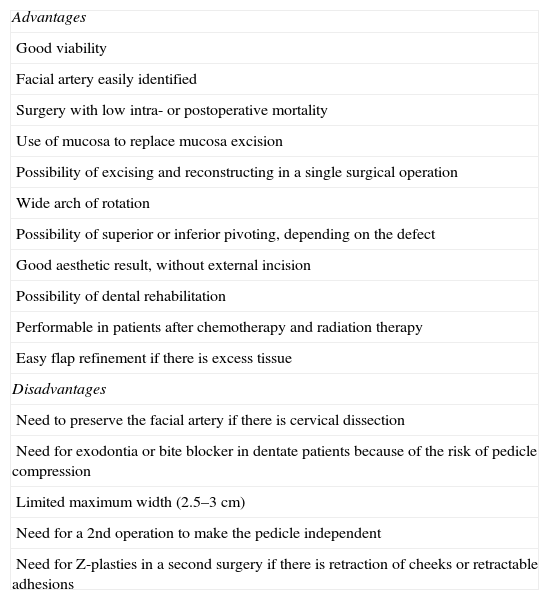
The facial artery musculomucosal (FAMM) flap is a good option for covering small and medium-sized defects in the oral cavity because of its similar tissue characteristics and easy implementation.
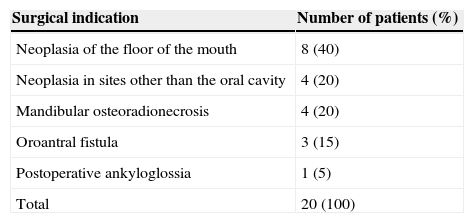
MethodsWe reviewed our results using this flap between 2006 and 2014. A total of 20 patients were included and 25 FAMM flaps were performed, 16 right (64%) and 9 left (36%) flaps. Five patients had simultaneous bilateral reconstructions. The indications for flap surgery were reconstruction after resection of tumours in the floor of the mouth (8 cases, 40%), tumours in other sites of the oral cavity (4 cases, 20%), mandibular osteoradionecrosis (4 cases, 20%), oroantral fistula (3 cases, 15%), and postoperative ankyloglossia (one case, 5%).
ResultsReconstruction was successful in 92% of cases (n=23). Total flap necrosis occurred in one case and dehiscence with exposure of bone in another. Oral function and ingestion were satisfactory in all patients.
ConclusionsThe facial artery musculomucosal flap is reliable and versatile for reconstruction of small and medium-sized intraoral defects. It allows functional reconstruction of the oral cavity with a low risk of complications.
El colgajo músculo-mucoso de arteria facial (FAMM) es un buen recurso para la cobertura de defectos intraorales de pequeño y mediano tamaño debido a sus características tisulares y a su facilidad de realización.
MétodosRevisión retrospectiva de los resultados obtenidos con el colgajo, realizados en nuestro centro durante el periodo 2006–2014. Se intervino a un total de 20 pacientes sobre los que se realizaron 25 colgajos tipo FAMM, 16 derechos (64%) y 9 izquierdos (36%). El colgajo se utilizó de forma bilateral y simultánea en 5 pacientes. Las indicaciones para la realización de los colgajos fueron: reconstrucción tras exéresis de neoplasias del suelo de la boca (8 casos; 40%), neoplasias en otras localizaciones de cavidad oral (4 casos; 20%), osteorradionecrosis mandibular (4 casos; 20%), fístula oroantral (3 casos; 15%) y anquiloglosia posquirúrgica (un caso; 5%).
ResultadosEl colgajo consiguió una reconstrucción satisfactoria en el 92% de los casos (n=23). Se produjo una necrosis del colgajo en una ocasión, y una dehiscencia con exposición de hueso subyacente en otra ocasión. Se consiguió una ingesta y función oral satisfactoria en la totalidad de los pacientes.
ConclusionesDada su fiabilidad y versatilidad, el colgajo músculo-mucoso de arteria facial es una técnica adecuada para la reconstrucción de defectos orales de pequeño y mediano tamaño. Permite una reconstrucción funcional adecuada de la cavidad oral con escaso riesgo de complicaciones.