Lymph node density or lymph node ratio (LNR), defined as the quotient between the total number of positive lymph nodes and the total number of dissected lymph nodes, has demonstrated a prognostic capacity in several tumour models, including patients with head and neck squamous cell carcinomas (HNSCC). The aim of the present study is to analyse the prognostic value of LNR in a wide cohort of patients with HNSCC.
MethodsWe carried out a retrospective study of a cohort of 1311 patients with HNSCC treated with unilateral or bilateral neck dissections. Of the patients included in the study, 55.0% had lymph node metastases (pN +). We proceeded to calculate the value of the LNR, and its categorization through a recursive partition analysis considering specific survival as the dependent variable.
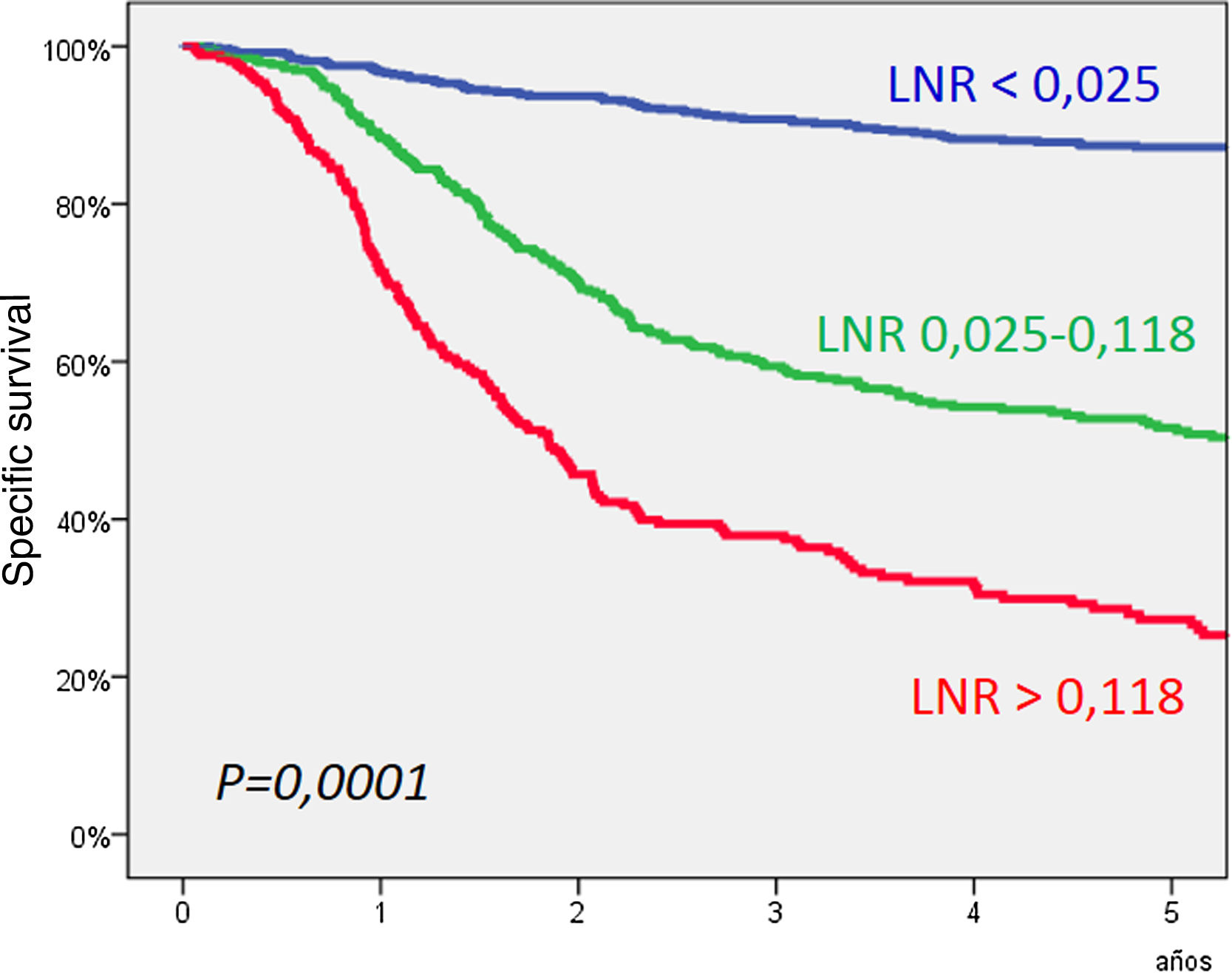
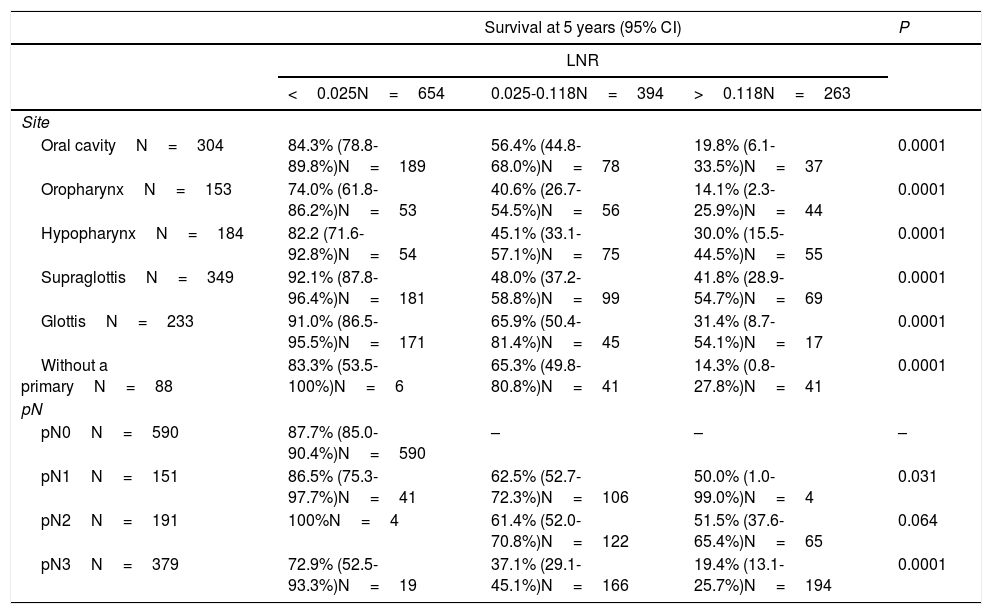
ResultsThree categories were defined according to the value of the LNR with a cut-off point at the values < of .025 and .118. The 5-year specific survival for patients with an LNR less than .025 (n = 654, 49.8%) was 87.2%, for patients with a LNR .025–.118 (n = 394, 30.1%) it was 51.6%, and for patients with a LNR greater than .188 (n = 263, 20.1%) it was 27.3% (P = .0001). According to the results of a multivariate analysis, the LNR significantly related to specific survival.
ConclusionThe LNR can be a prognostic variable to be considered in the pathological staging of the lymph nodes.
La densidad ganglionar o lymph node ratio (LNR), definido como el cociente entre el número total de ganglios positivos y el número total de ganglios disecados ha demostrado una capacidad pronóstica en diferentes modelos tumorales, incluidos los pacientes con carcinomas escamosos de cabeza y cuello (CECC). El objetivo del presente estudio es analizar el valor pronóstico del LNR en una serie amplia de pacientes con CECC.
MétodosSe llevó a cabo un estudio retrospectivo de una cohorte de 1.311 pacientes con CECC tratados con vaciamientos cervicales uni o bilaterales. El 55,0% de los pacientes incluidos en el estudio contaron con la presencia de metástasis a nivel ganglionar (pN+). Se procedió a calcular el valor del LNR, y a su categorización mediante un análisis de partición recursiva considerando la supervivencia específica como la variable dependiente.
ResultadosSe definieron tres categorías en función del valor del LNR con unos puntos de corte en los valores de 0,025 y 0,118. La supervivencia específica a los 5 años para los pacientes con un LNR inferior a 0,025 (n = 654, 49,8%) fue del 87,2%, para los pacientes con un LNR 0,025–0,118 (n = 394, 30,1%) del 51,6%, y para los pacientes con LNR superior a 0,188 (n = 263, 20,1%) del 27,3% (P = 0,0001). De acuerdo con los resultados de un análisis multivariante, el LNR se relacionó de forma significativa con la supervivencia específica.
ConclusiónEl LNR puede ser una variable pronóstica a considerar en la estadificación patológica de las áreas ganglionares.