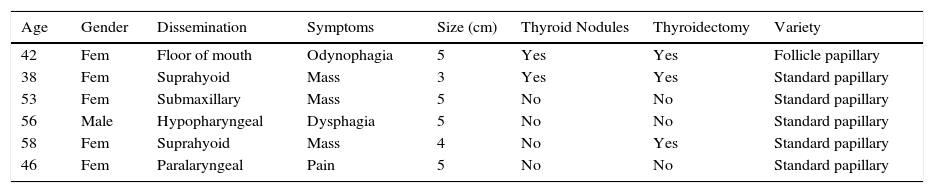
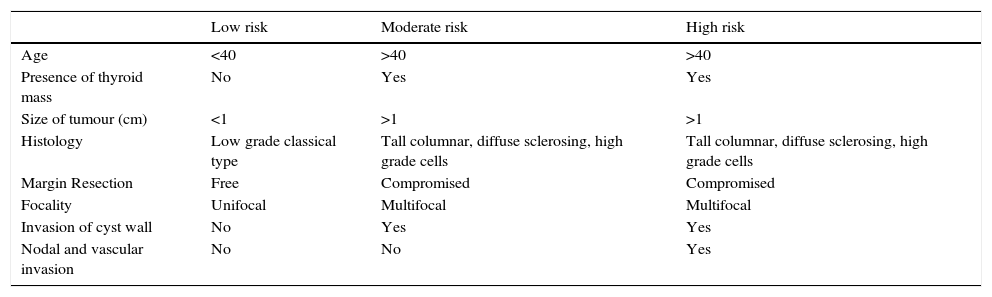
The thyroglossal cyst can exceptionally appear as a primary cyst carcinoma. We discuss a series of 6 adult patients, assessed for long-lasting asymptomatic suprahyoid or lateral-to-larynx mass. The images showed a heterogeneous mass invading adjacent soft tissues. Fine needle aspiration biopsy did not contribute to diagnosis. We performed a Sistrunk procedure in all cases, 3 combined with total thyroidectomy and 1 with neck dissection. The postoperative course was favourable. No additional treatment was required, without evidence of recurrence in follow-up. The management is controversial due to the limited number of cases reported. Some classifications based on size and extent have been proposed to define the surgical treatment of such cysts.
El quiste del conducto tirogloso se puede manifestar excepcionalmente como un carcinoma primario. Se presenta una serie de 6 casos de pacientes adultos que consultaron por masa suprahiodea o paralaríngea asintomática de larga evolución. Las imágenes mostraron una masa heterogénea con extensión a tejidos blandos. La biopsia aspirativa de la lesión no contribuyó al diagnóstico. En todos los casos se realizó cirugía de Sistrunk, en 3 casos combinada con tiroidectomía total y en uno, con vaciamiento. El curso posquirúrgico fue favourable. No requirieron tratamiento adicional y no presentaron recurrencias. El manejo es controvertido debido a los pocos casos reportados. Se han propuesto algunas clasificaciones basadas en el tamaño y la extensión para definir el tratamiento quirúrgico.