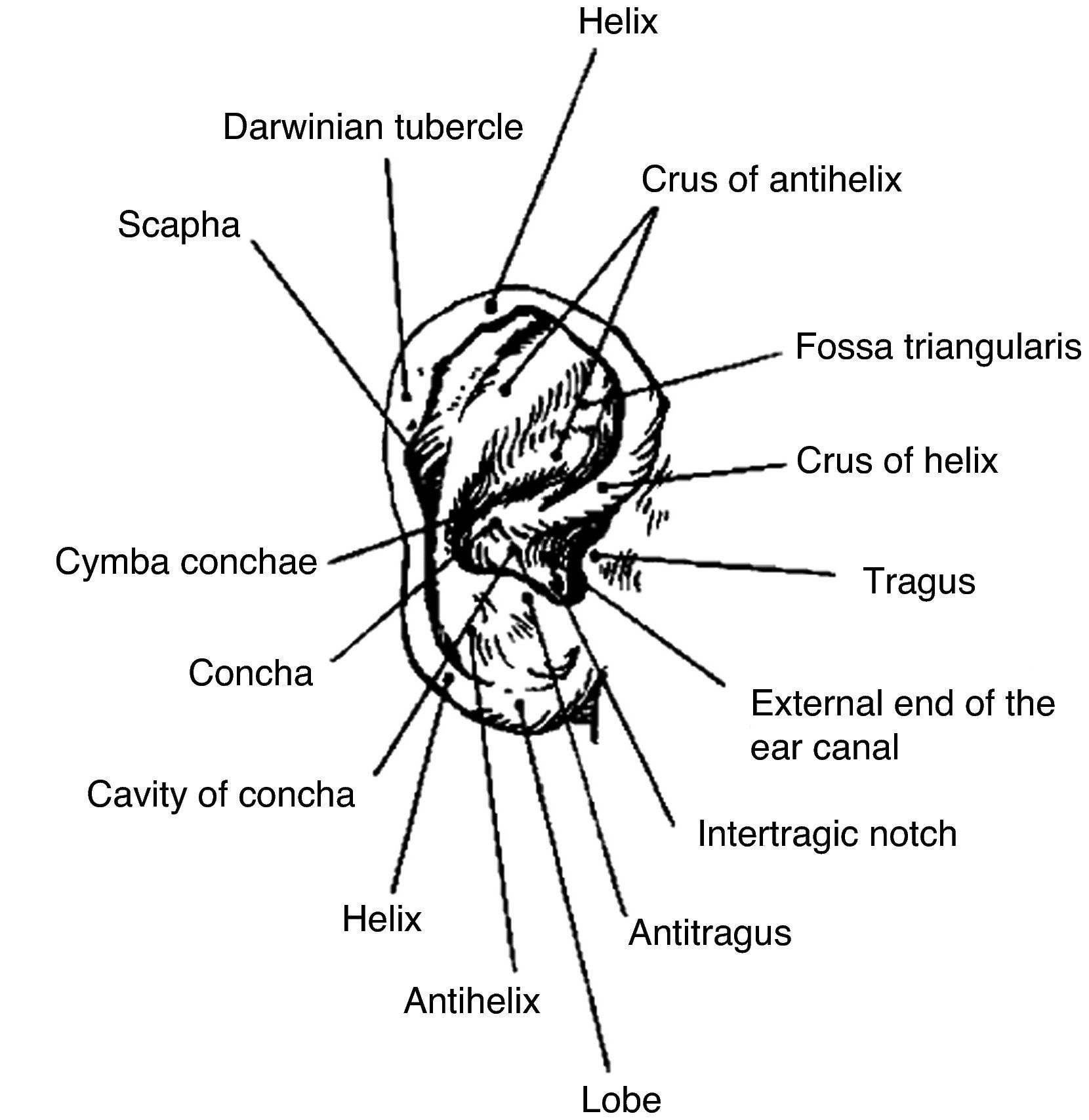
Some loop ear surgical procedures include cartilage section or abrasion, while others involve antihelix folding by simple suture.
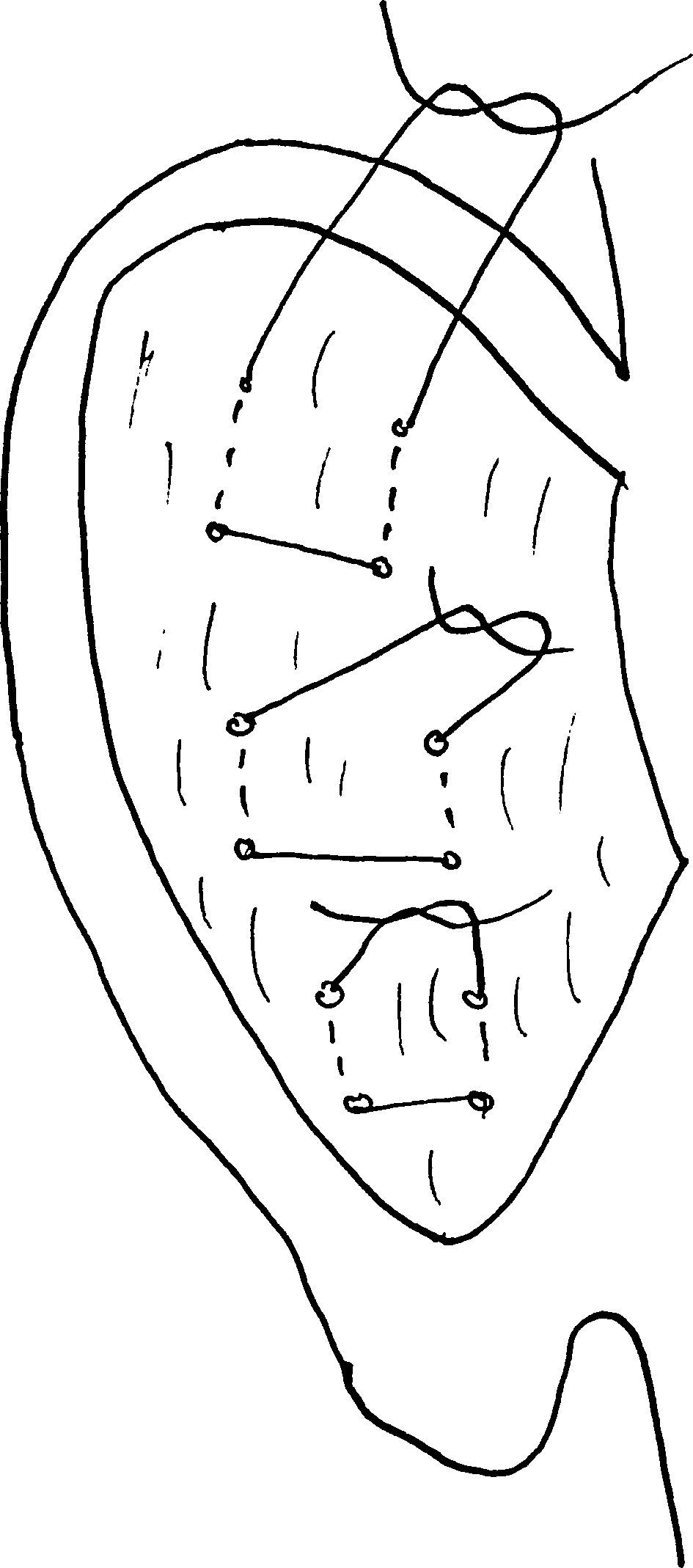
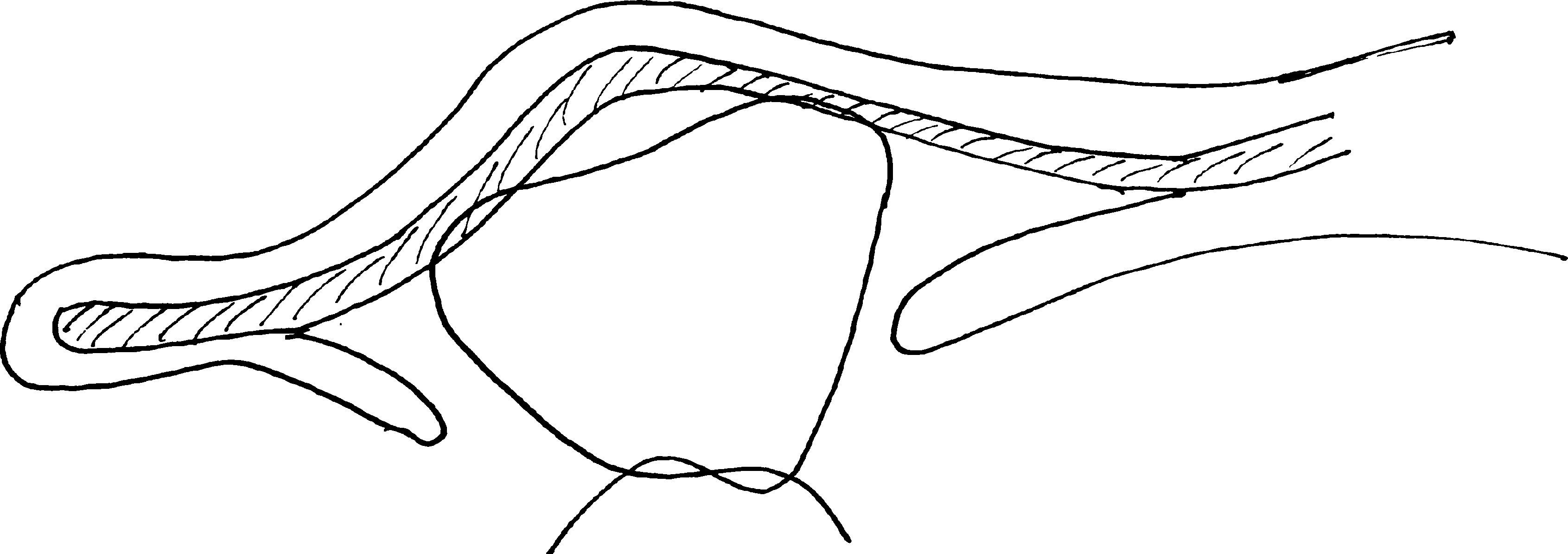
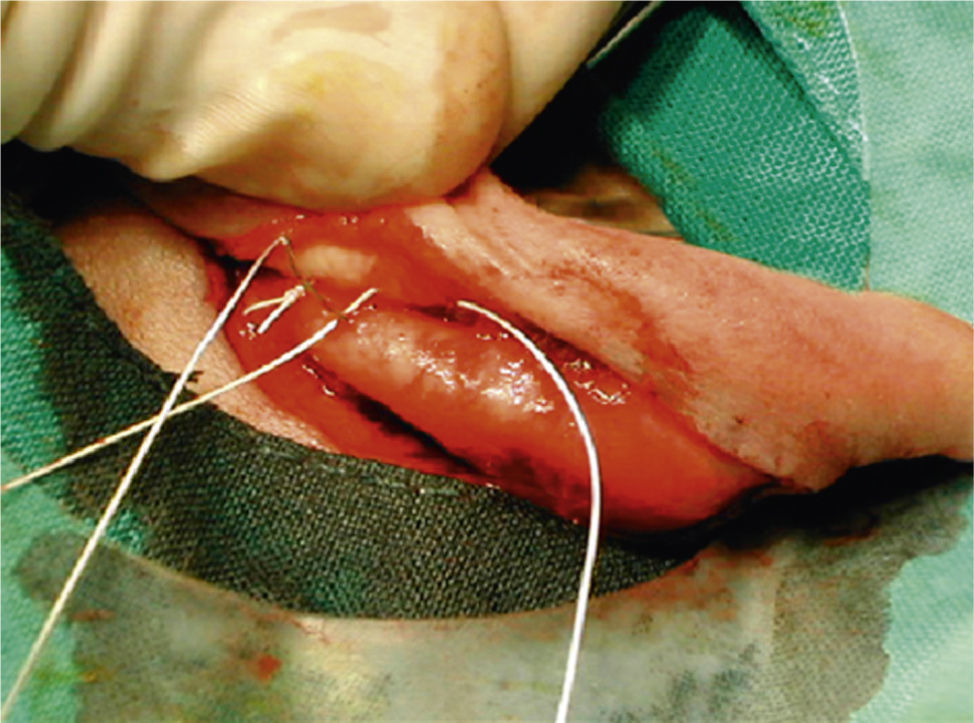
MethodsOur results with the Mustardé technique are presented. This procedure avoids an aggressive action on the ear cartilage and makes antihelix folding easier.
ResultsGood aesthetic results were obtained in all our patients, with a low complication rate.
ConclusionsWe conclude this cartilage technical procedure has an advantage over the aggressive ones, with a low complication rate.
Entre las técnicas quirúrgicas para el tratamiento de las orejas en asa podemos distinguir entre las que conllevan una sección ó abrasión del cartílago y las que únicamente se basan en la sutura del mismo.
MétodosPresentamos nuestros resultados mediante la técnica de Mustardé, con la que evitamos realizar una acción agresiva sobre el cartílago, facilitando la formación del pliegue del antehélix.
ResultadosEn nuestra serie hemos obtenido un buen resultado estético, con bajo porcentaje de complicaciones.
ConclusionesPensamos que esta técnica aporta una ventaja sobre las que son agresivas con el cartílago, presentando un bajo porcentaje de complicaciones.