The middle fossa approach is a surgical technique that is very useful for lateral skull base surgery. However, it is true that it has limited surgical indications and implementation due to its technical complexity.
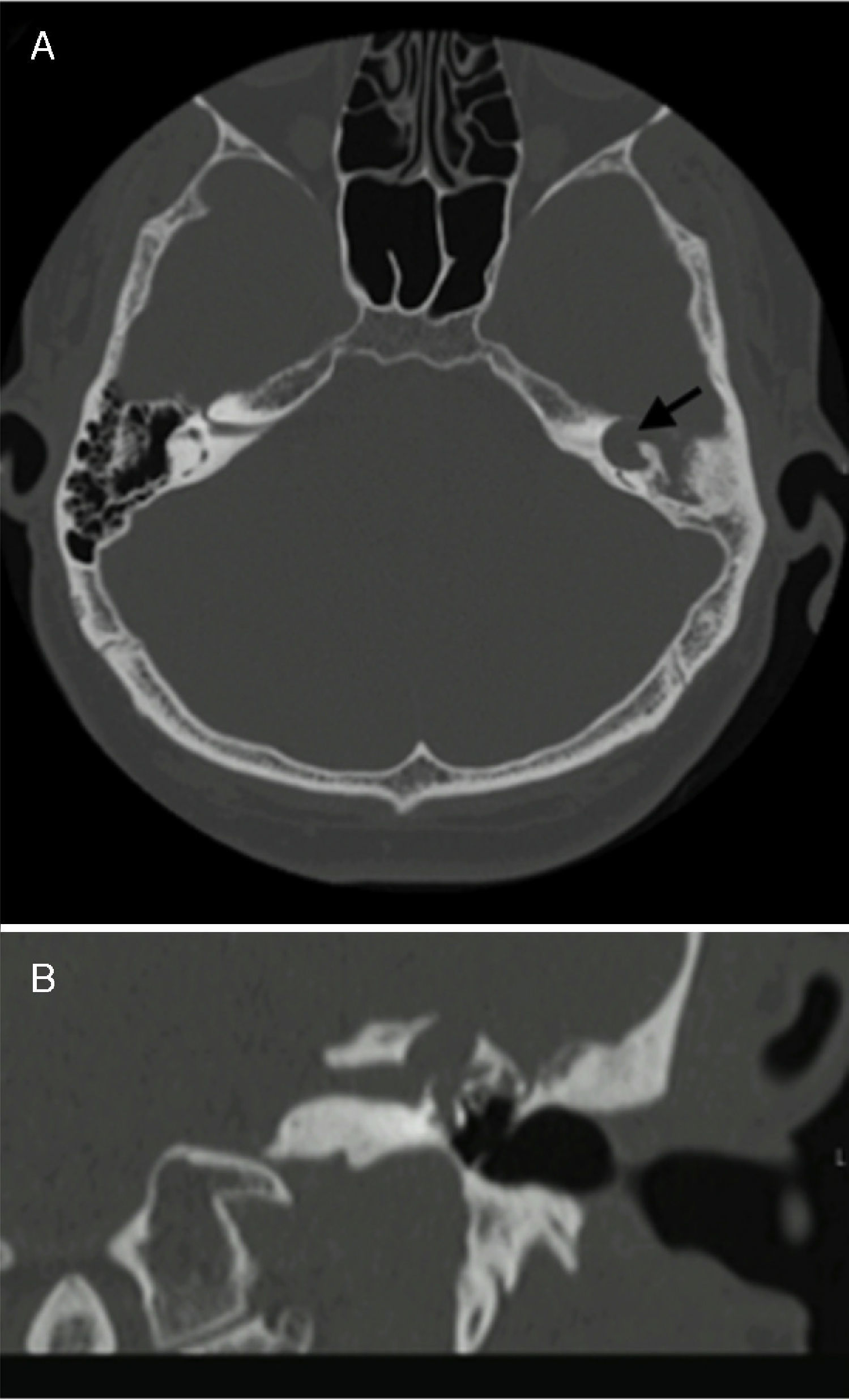
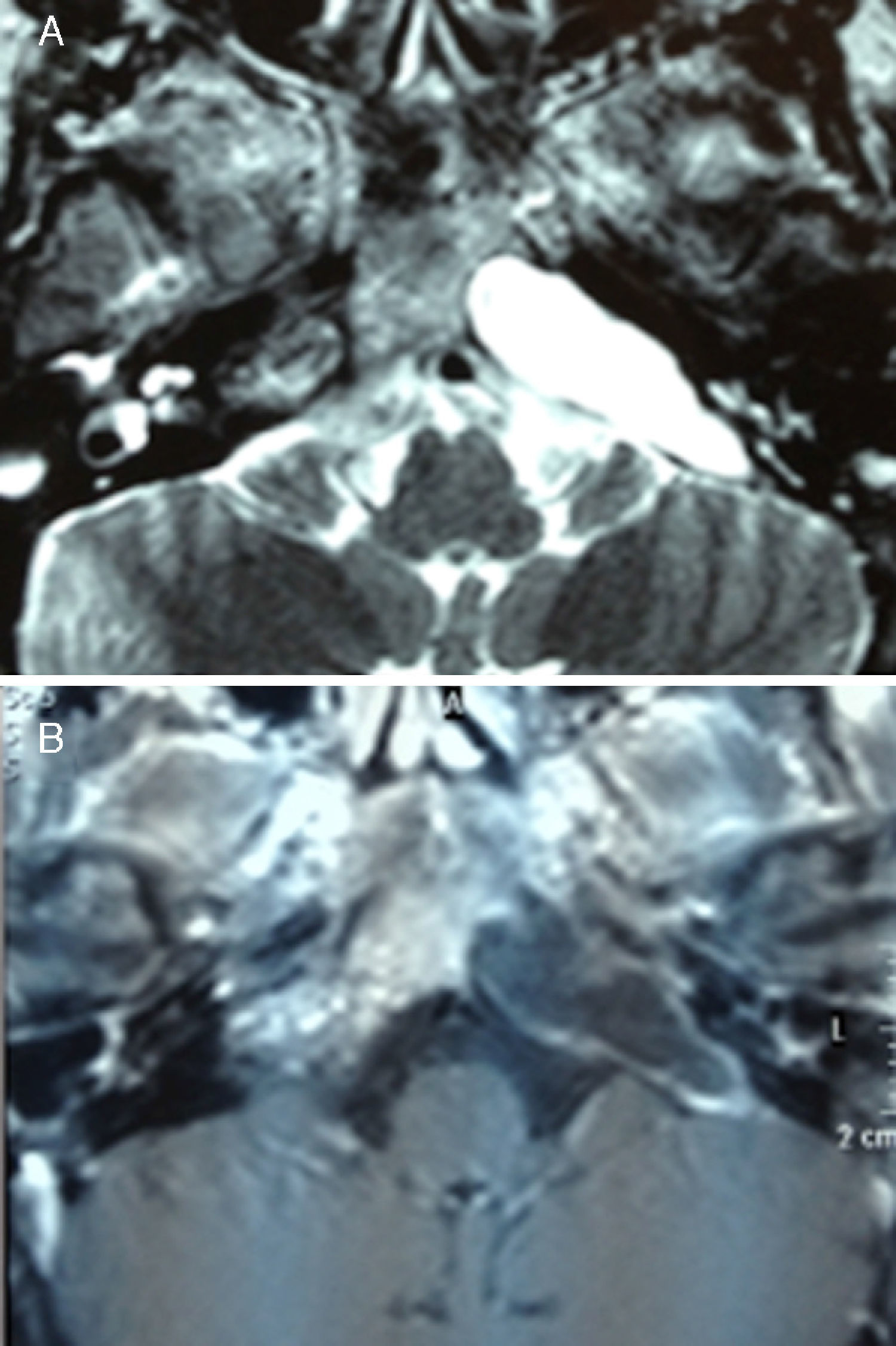
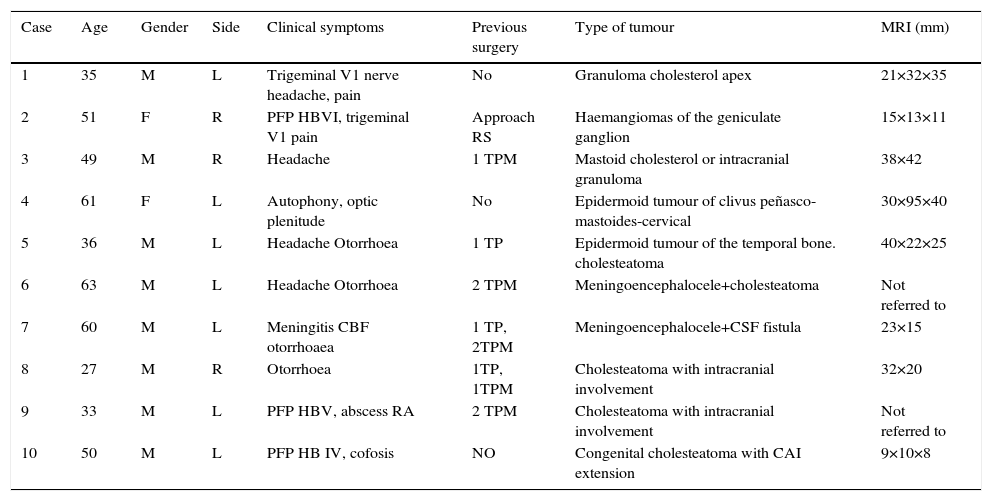
We present our experience in 10 patients in whom the middle fossa approach was the treatment of choice because of the extent of the injury and complexity of the lesion or process.
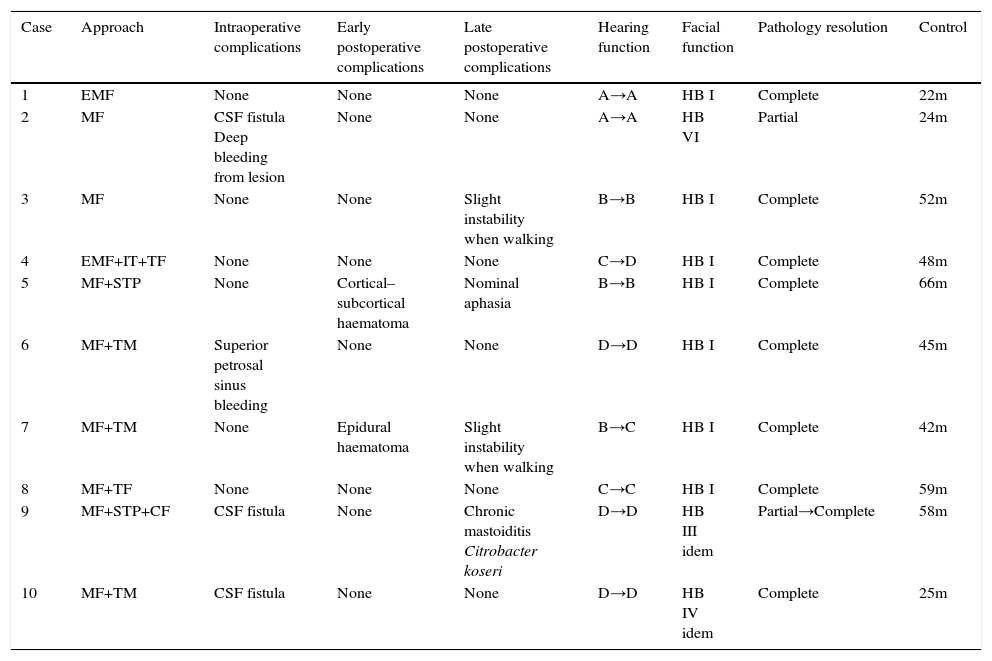
Despite the complexity of the cases, there was no mortality associated with surgery. Postoperative complications were found in 2 patients who presented an epidural haematoma and a cortico-subcortical haematoma. Hearing function was preserved in 5 patients out of the 7 who had adequate hearing at the time of surgery. House/Brackmann I-II facial nerve function was achieved in 8 patients; the remaining 2 had no deterioration of the nerve function. In 9 out of 10 patients, the surgery achieved complete solution of the lesion.
The middle fossa approach is a safe and reliable surgical technique. It gives us great control and exposure of different skull base processes. We consider its knowledge of great importance, because it may be the only viable surgical alternative in some specific patients. That is the reason why it is important to learn this approach and know about it in our specialty.
El abordaje por fosa media es una técnica quirúrgica de gran utilidad en la cirugía de base de cráneo lateral. Si bien es cierto, que por sus restringidas indicaciones así como por su complejidad técnica ha tenido una implantación limitada.
Presentamos nuestra experiencia en 10 pacientes en los cuales por gran complejidad del proceso, la situación o la extensión de la lesión, el abordaje por fosa media fue el tratamiento de elección.
A pesar de la gran complejidad de los casos no hubo ningún caso de mortalidad asociada a la cirugía. De la morbilidad registrada destacar un hematoma epidural y un hematoma córtico-subcortical. La función auditiva se preservó en 5 pacientes de los 7 pacientes que presentan audición en el momento de la cirugía. En 8 pacientes se logró una función facial House/Brackmann I-II y en los 2 restantes no hubo empeoramiento de la misma función. En 9 de los 10 pacientes se realizó una cirugía resolutiva de la patología.
El abordaje por fosa media es una técnica quirúrgica segura y fiable. Nos proporciona un gran control y exposición de los diferentes procesos patológicos de la base de cráneo. Consideramos de gran importancia su conocimiento, pues en determinados pacientes puede ser la única alternativa viable y resolutiva, de ahí la importancia de difundir este abordaje en nuestra especialidad.