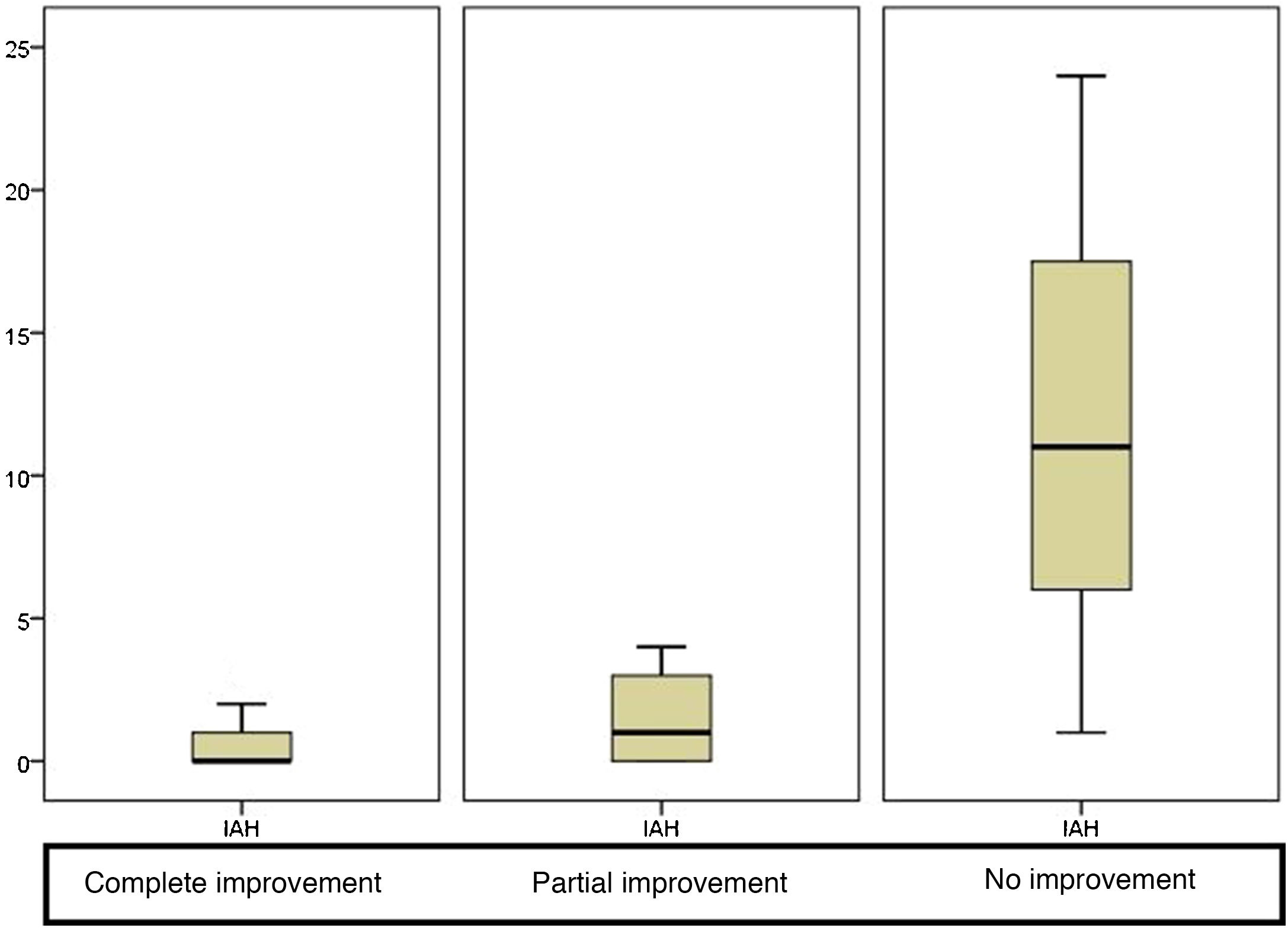
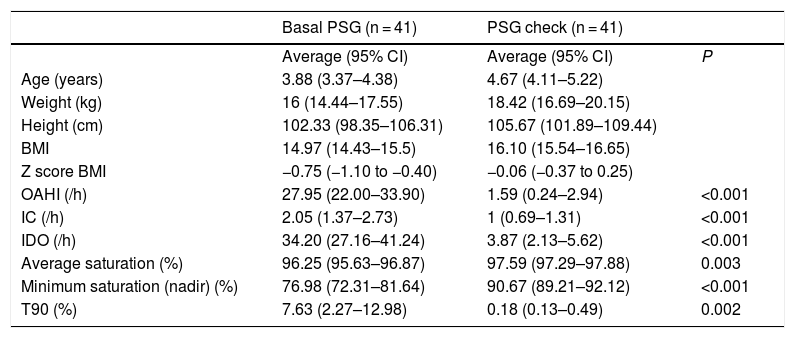
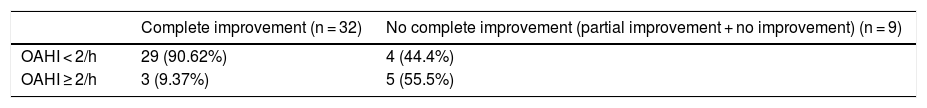
Hypertrophy of adenotonsillar tissue is the most common cause of OSAS in otherwise healthy children, and therefore adenotonsillectomy is the first line treatment. Scientific societies recommend nocturnal follow-up PSG to assess for residual OSAS in children with preoperative evidence for moderate to severe OSAS, obesity, craniofacial anomalies that obstruct the upper airway and neurological disorders, based on the increasing trend of publications reporting residual OSAS after adenotonsillectomy. Follow-up PSG values in children with a pre-operative diagnosis of severe OSAS were analysed retrospectively, and compared to the parents’ impression after ENT surgery. The study population included 41 healthy children with severe OSAS and adenotonsillar surgery. The percentage of children with normal PSG parameters (AHI < 2/h) after adenotonsillectomy was 80.48%. A very good correlation was observed between the parents’ perception after treatment and the follow-up PSG parameters, specifically when the parents perceived that the patient had shown “complete resolution” (no snoring or apnoea), 90.62% of the children had an AHI < 2/h in the follow-up PSG, the maximum residual AHI being 2.6/h. In healthy children with no underlying pathology, the information provided by the parents on clinical progression after surgery could be useful and might enable the selection of those patients who require a follow-up study, avoiding overload in sleep units.
La hipertrofia adenoamigdalar es, en niños sin patología de base, la causa más frecuente de SAHOS y, por tanto, la adenoamigdalectomía constituye la primera línea de tratamiento. Diferentes sociedades científicas recomiendan la realización de una PSG de control en el seguimiento, en caso de niños con patología de base o si el diagnóstico previo a la cirugía era de SAHOS moderado o severo, debido a la tendencia creciente de publicaciones con SAHOS residual tras adenoamigdalectomía. Se analiza retrospectivamente la correlación entre la percepción de los padres tras cirugía ORL y el resultado de la PSG de control en niños con diagnóstico de SAHOS severo en los que se ha realizado tratamiento quirúrgico. Se incluyeron 41 niños con SAHOS severo y cirugía adenoamigdalar, cuya tasa de curación ha sido del 80,48%. Se observa muy buena correlación entre la percepción de los padres tras el tratamiento y los índices en la PSG de control, destacando que cuando los padres percibían que el paciente había experimentado una «resolución completa» (no ronquido ni apneas), el 90,62% de los niños presentaban un IAHO < 2/h en el control posterior al tratamiento, siendo el IAHO residual máximo de 2,6/h. Concluimos que, en un niño sin patología de base, la información aportada por los padres acerca de la evolución clínica tras la cirugía podría ser discriminativa para elegir a aquellos pacientes a los que solicitar un estudio de control, evitando sobrecargas en las unidades de sueño.