Benign lesions of the external auditory canal (EAC) are an infrequent cause of temporal bone CT scan requests. We are not usually well-versed in the different pathologies located in the EAC, perhaps because it is “only” a conduit and the relevant anatomical structures are located in the middle and inner ear.
Our objective was to improve knowledge of this structure by reviewing the different benign conditions found in this location.
MethodsWe reviewed the CT studies from 2 years (January 2010 through January 2012), selecting those containing lesions in the EAC. To complement this, due to the importance of these lesions, these medical histories were then analysed considering the presentation and otoscopic examination findings.
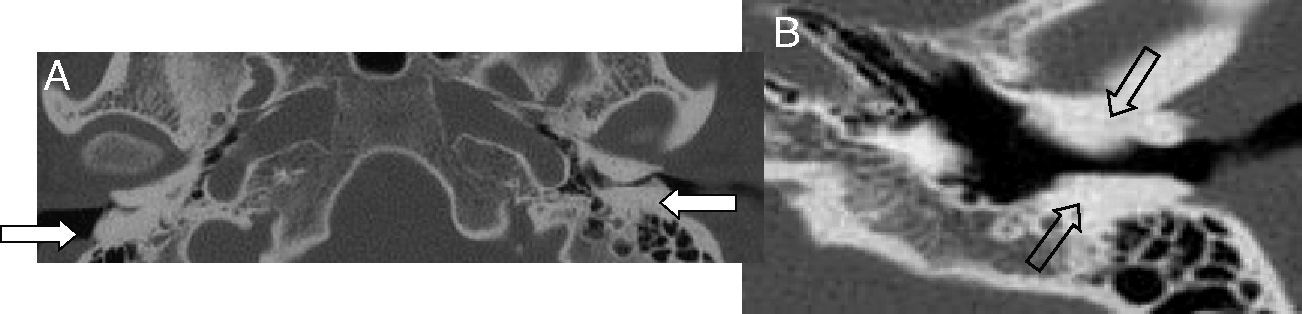
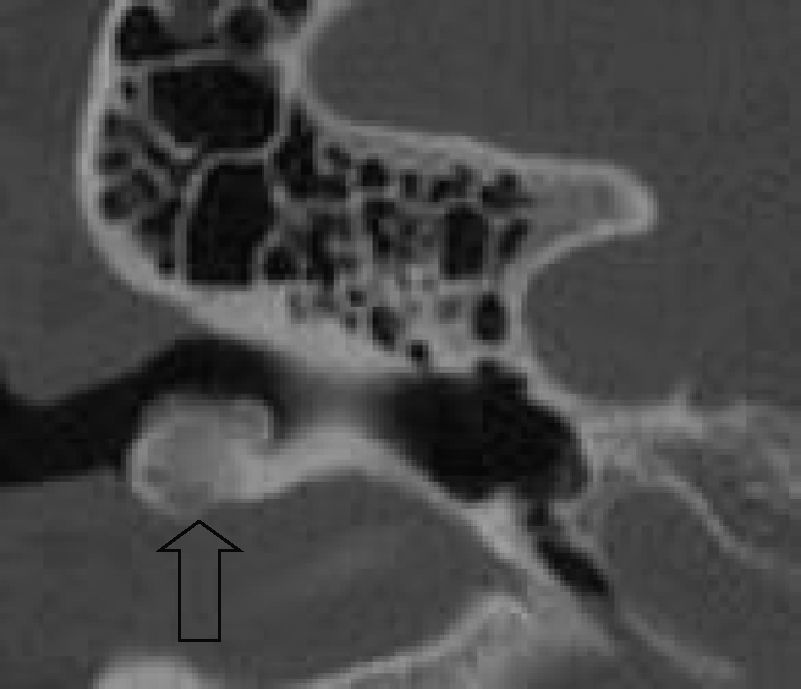
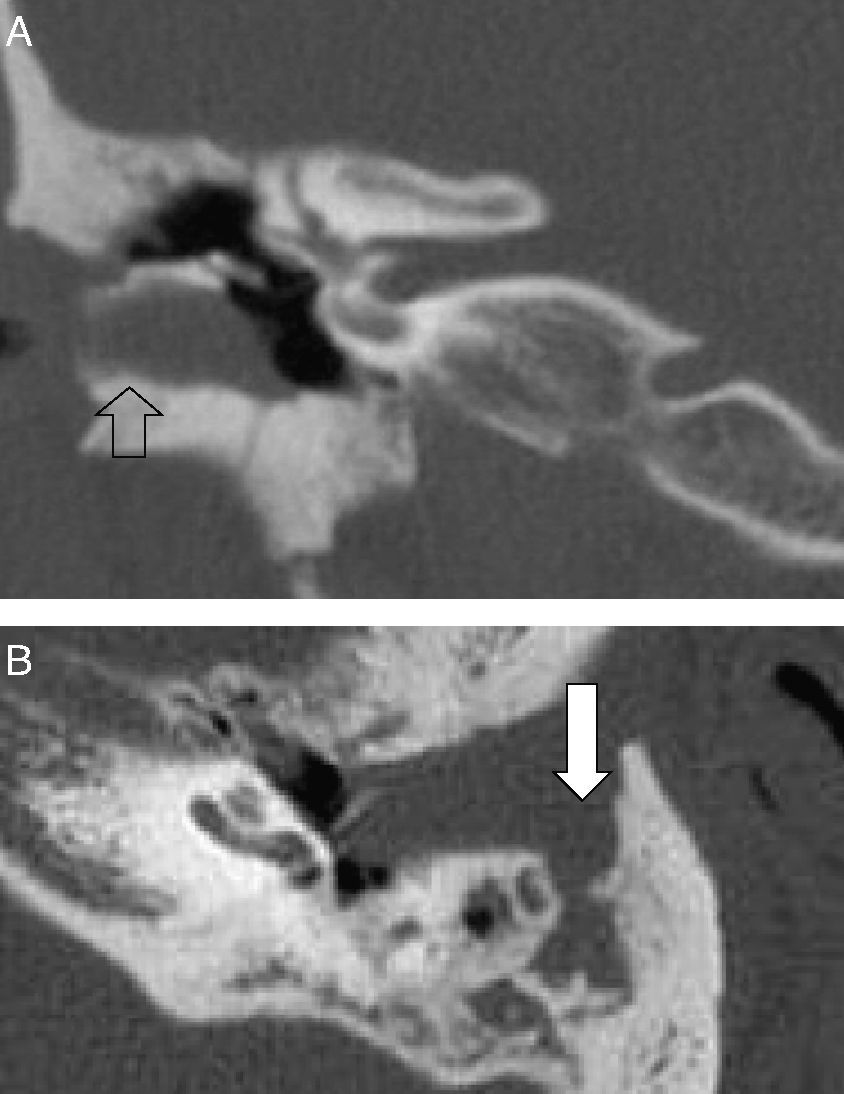
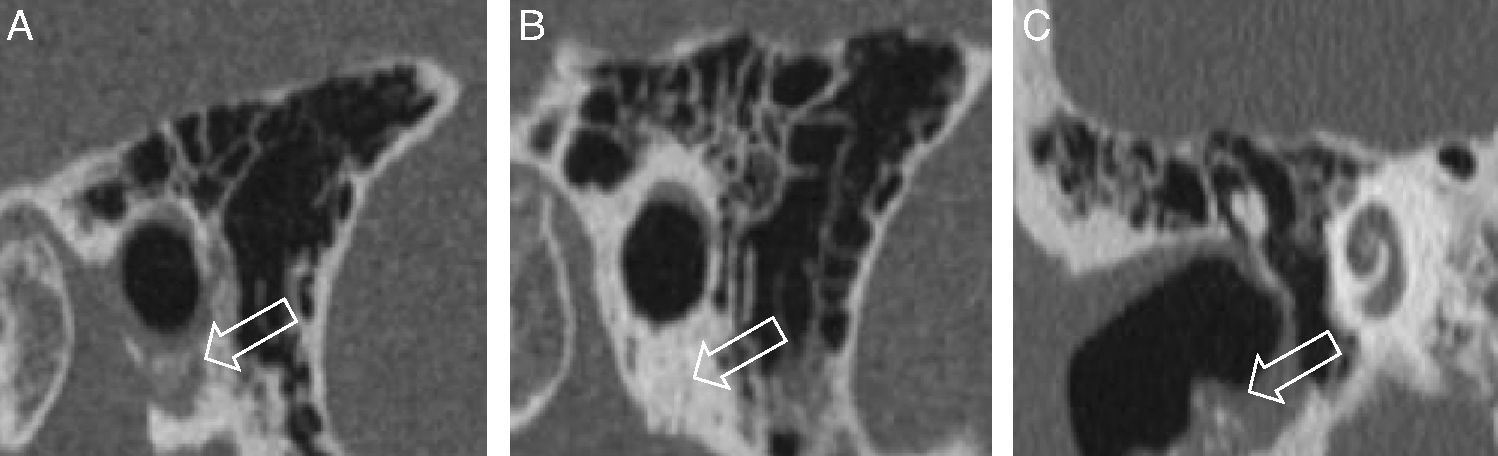
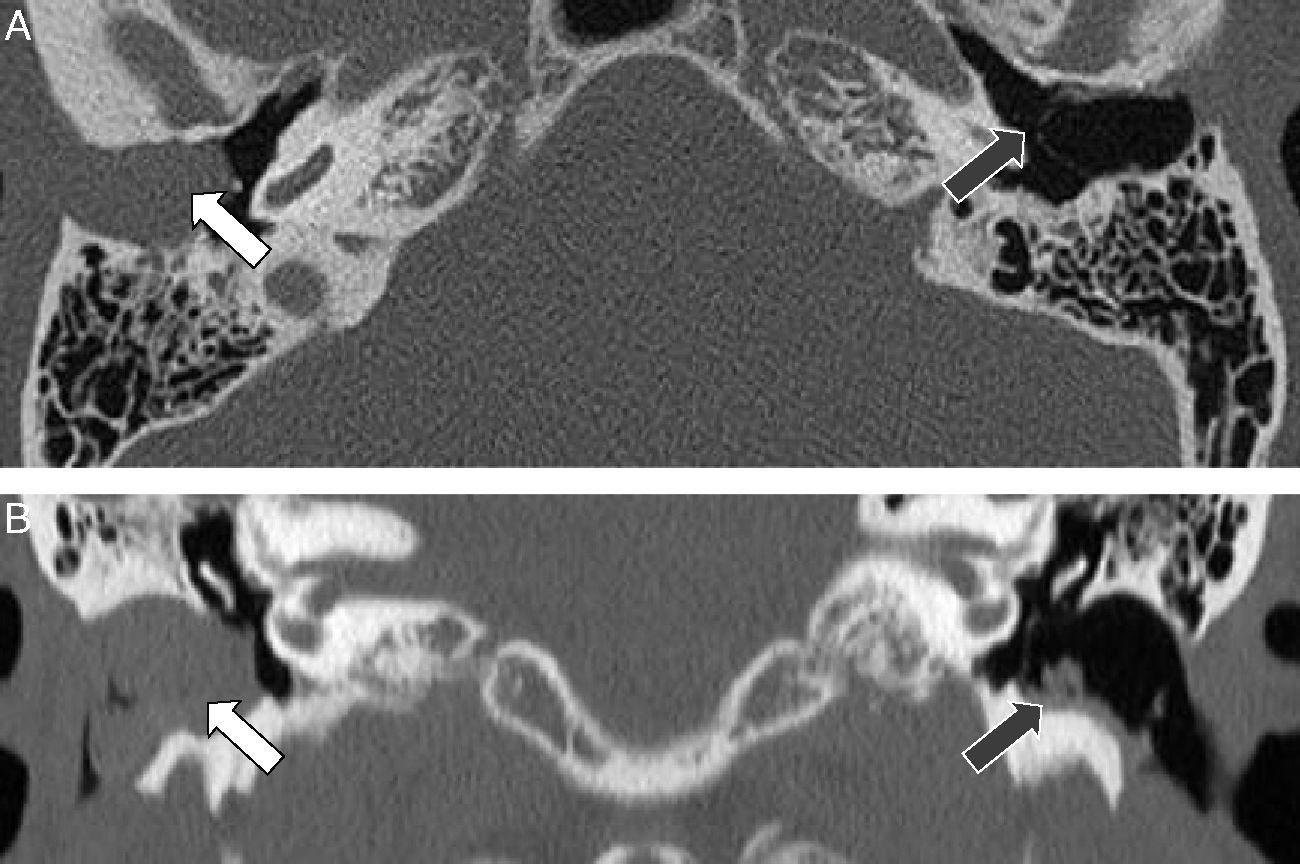
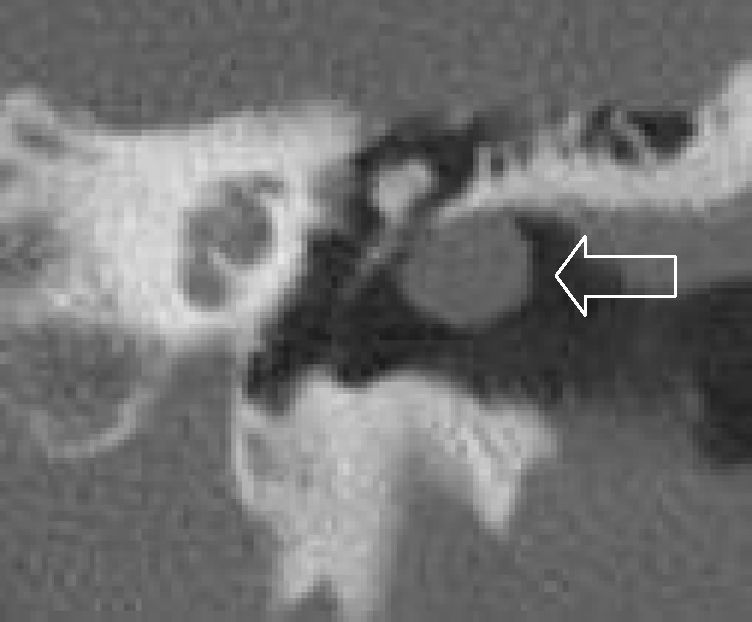
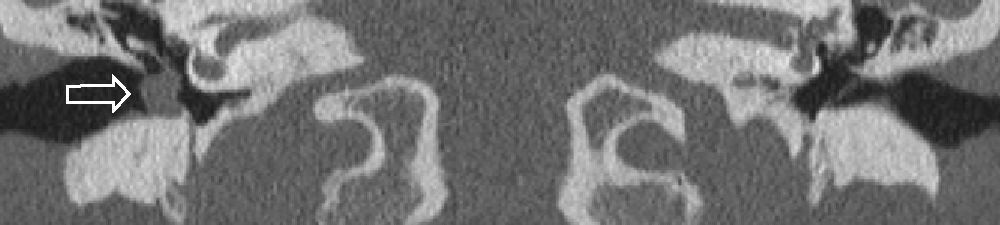
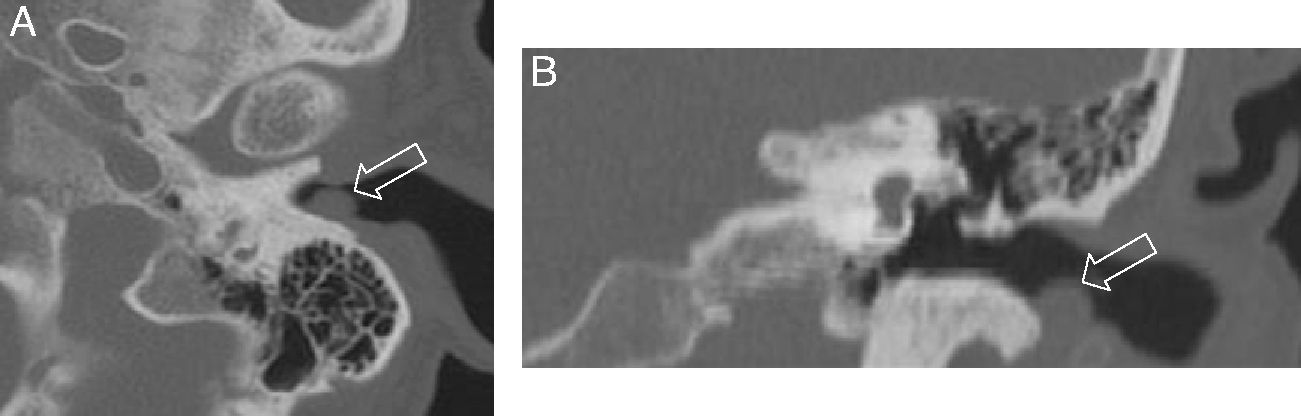
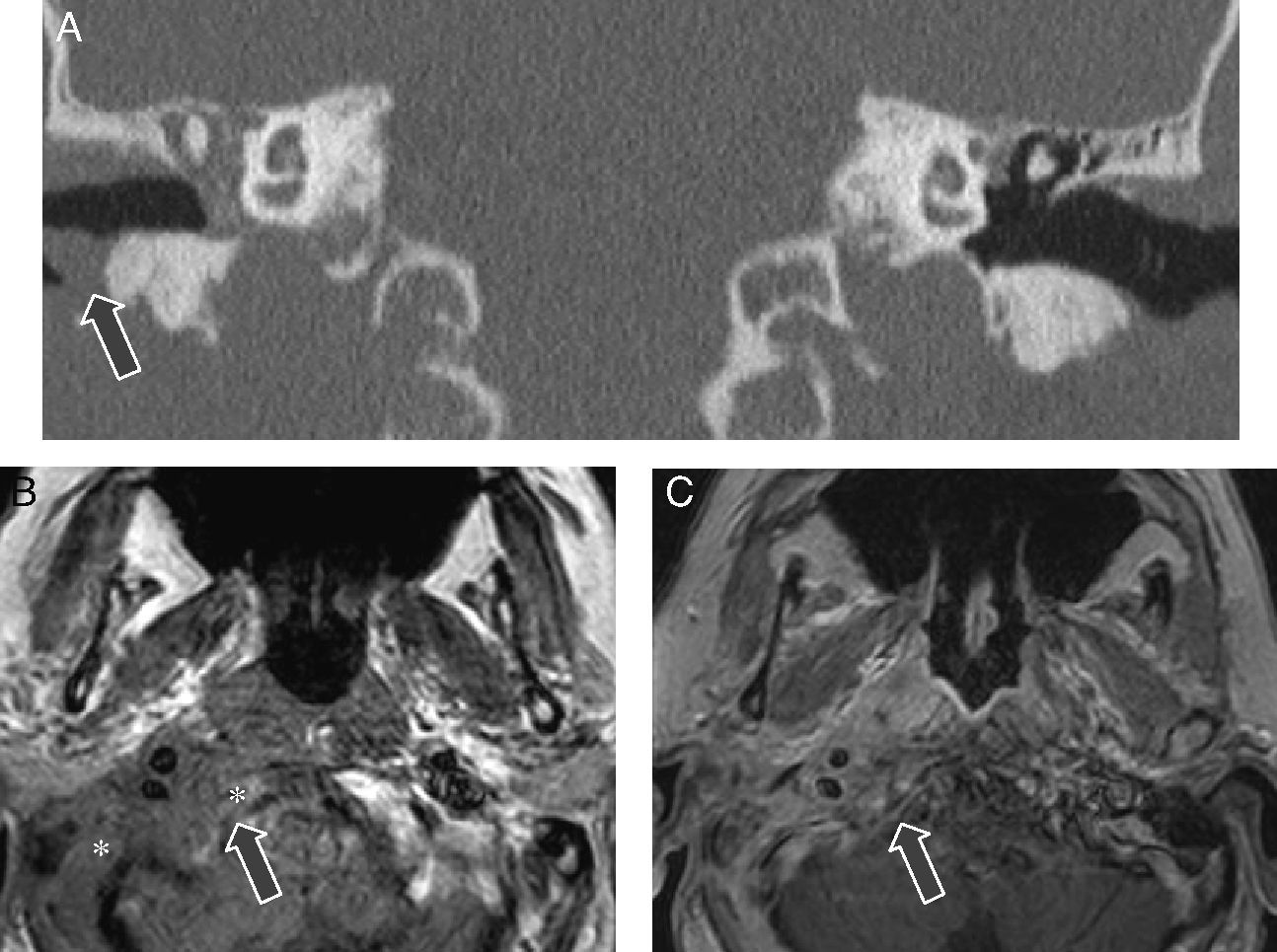
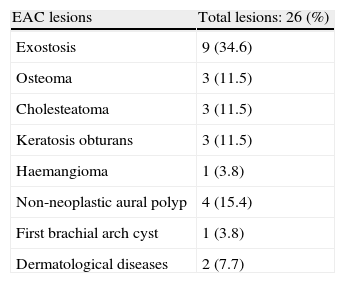
ResultsThe lesions were classified according to their diagnoses: exostosis, osteoma, cholesteatoma, keratosis obturans, haemangioma, non-neoplastic aural polyp, first branchial cyst and dermatologic disease (malignant external otitis). The presence of EAC occupation in the otological examination and chronic otorrhea as the symptom of presentation were the most relevant exploratory and clinical findings.
ConclusionsBenign EAC lesions are an uncommon and seldom studied cause of temporal bone CT scan requests. Knowing the most relevant clinical and radiological findings is necessary for their proper diagnosis.
Las lesiones benignas del conducto auditivo externo son una causa infrecuente de estudio en la TC de peñascos. Tal vez porque es «solo» un conducto, y las estructuras anatómicas relevantes se encuentran en el oído medio e interno, generalmente no están bien valoradas las diferentes afecciones que asientan en el conducto auditivo externo.
Con el objetivo de mejorar el conocimiento de esta estructura se llevó a cabo una revisión de las lesiones benignas que podemos encontrar en esta localización.
MétodosSe trata de un estudio retrospectivo en el que se revisaron las imágenes de la TC de peñascos realizados en 2 años (enero de 2010 a enero de 2012). De ellos, se seleccionaron aquellos en los que el informe radiológico reportaba lesiones del conducto auditivo externo.
Posteriormente, y también de forma retrospectiva se realizó un análisis de las historias médicas de los pacientes, valorando los hallazgos clínicos y la exploración otoscópica.
ResultadosLas lesiones fueron clasificadas según su diagnóstico en: osteoma, colesteatoma, queratosis obturans, hemangioma, pólipo aural no neoplásico, quiste de primer arco branquial y enfermedades dermatológicas (otitis externa maligna). Los hallazgos clínicos más frecuentemente encontrados fueron la otorrea crónica como síntoma de presentación y la ocupación del conducto en la exploración otoscópica.
ConclusionesLas lesiones que afectan al canal auditivo externo son estudiadas de forma infrecuente en la TC de peñascos. Es necesario conocer los hallazgos clínicos y radiológicos más relevantes para poder realizar su correcto diagnóstico y estudio.