Pulmonary involvement exists in 80% of cases of infection with Mycobacterium tuberculosis; however, in up to 20% of cases there may be extra-pulmonary involvement. In the ENT area, the most common site is cervical lymphadenitis, affecting approximately 95% of cases.
Materials and methodsThis was a retrospective study of patients attending an ENT department in a tertiary hospital for head and neck symptoms that were diagnosed with tuberculosis (TB), between December 2007 and December 2013.
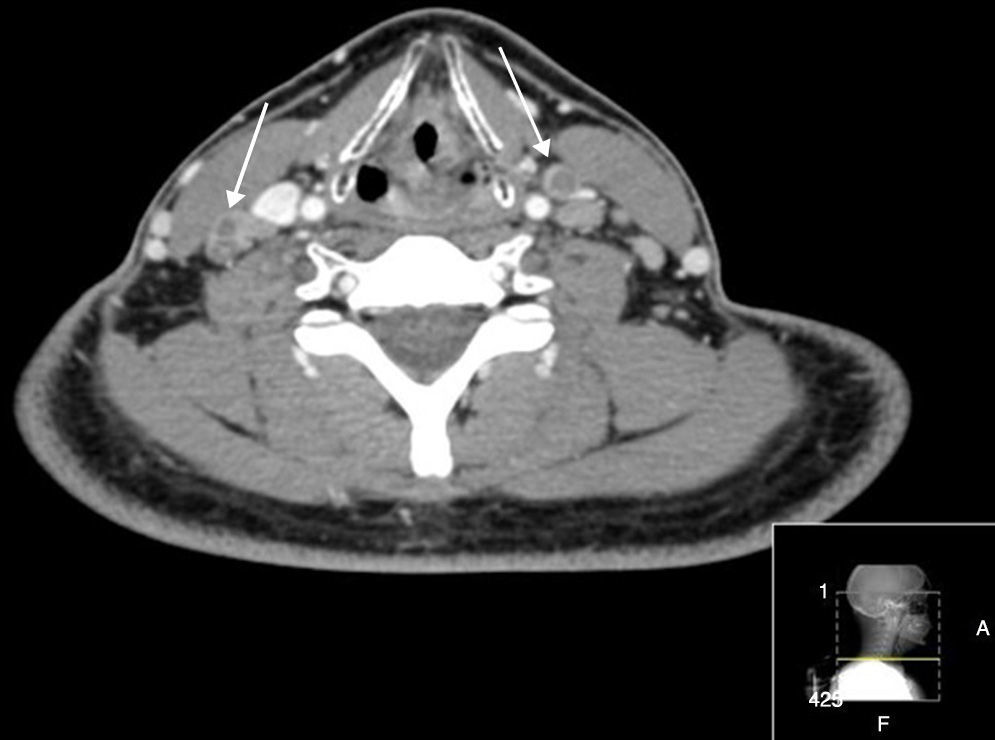
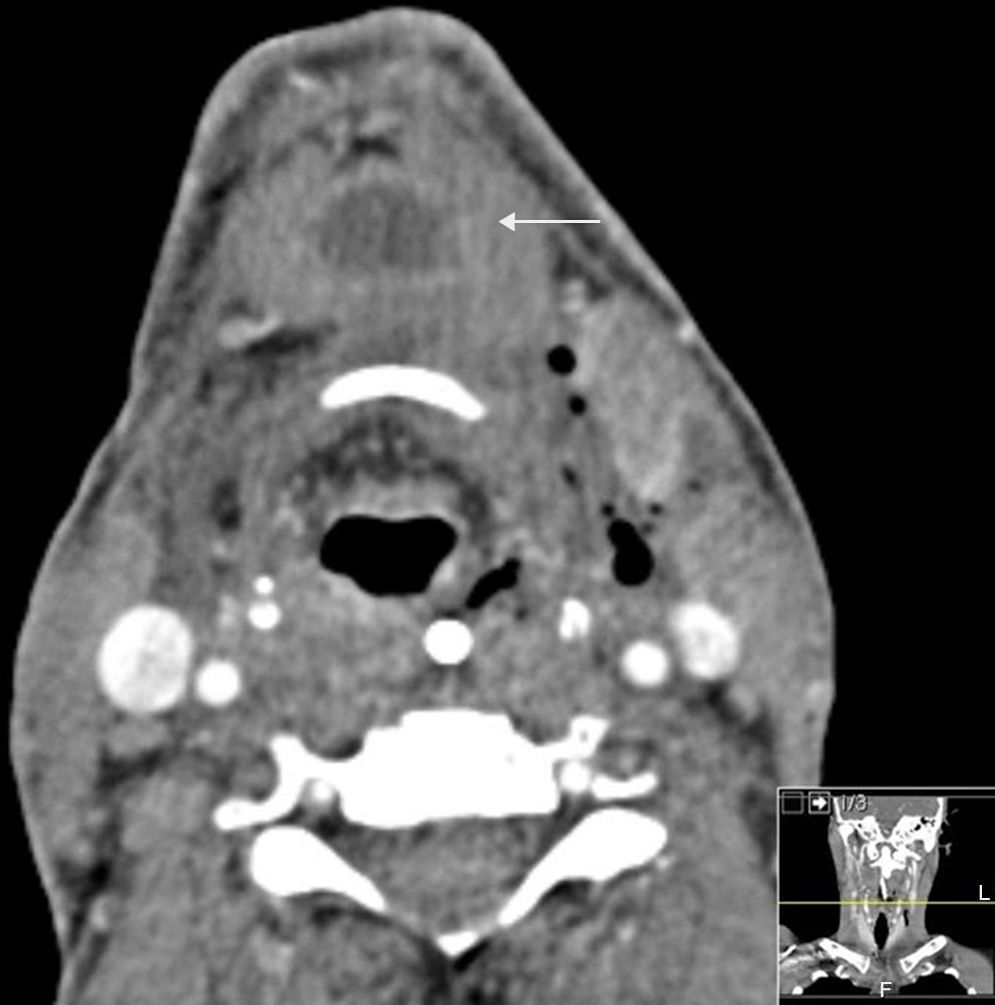
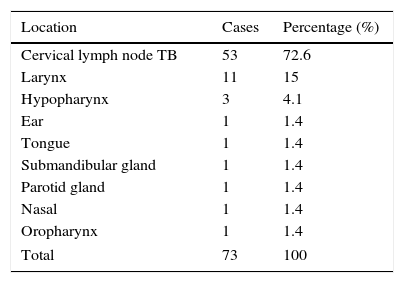
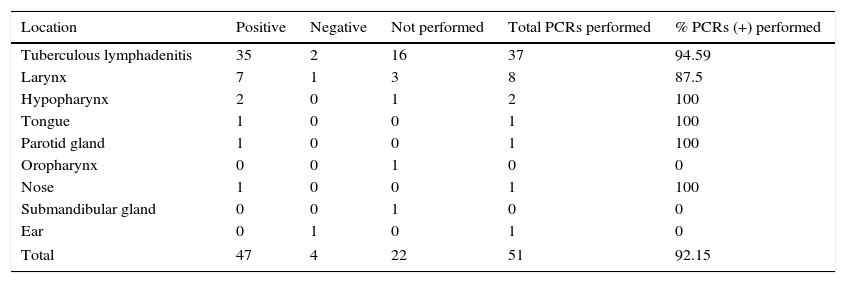
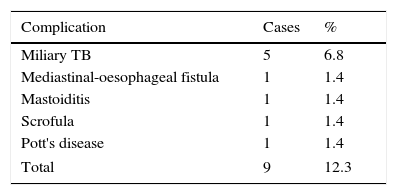
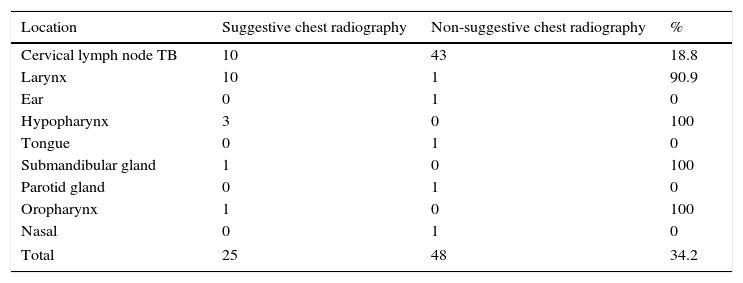
ResultsThe study included 73 patients, 41 (56.2%) males and 32 (43.8%) females (M/F ratio=1.28), with a mean age of 39.4 years (±26.5 years; Min 1, Max 88). There were 53 (72.6%) cases of cervical lymphadenopathy, 11 (15%) of laryngeal tuberculosis 3 (4.1%) of hypopharyngeal tuberculosis, and six cases in other locations. Of the total, 14 (19.2%) patients were HIV positive and 10 (13.7%) had a history of contact with relatives who had suffered pulmonary tuberculosis. PCR was performed in 51 (69.8%) cases to confirm being positive, of which 47 (92.1%) cases were.
ConclusionThe similarity of tuberculosis to diseases of poor prognosis and the difficulty of its diagnosis make considering tuberculosis necessary when exploring patients with ulcerative or granulomatous ENT lesions. Analysing our results, the incidence of TB according to its ENT area location is similar to that reported in the literature. It is important to make special mention of the use of PCR in our study and the benefits that its implementation means for diagnosis.
En el 80% de los casos de infección por Mycobacterium tuberculosis existe afectación pulmonar, sin embargo hasta en un 20% de casos puede haber compromiso extrapulmonar. En el área otorrinolaringológica la localización más frecuente es la linfadenitis cervical, que afecta aproximadamente al 95% de los casos.
Materiales y métodosEstudio retrospectivo en pacientes que acudieron a consulta de ORL en un hospital terciario por sintomatología en cabeza y cuello y que fueron diagnosticados de tuberculosis, entre diciembre del año 2007 y diciembre del año 2013.
ResultadosUn total de 73 pacientes fueron incluidos, 41 (56,2%) hombres y 32 (43,8%) mujeres (ratio H/M=1,28), con una edad promedio de 39,4 años (±26,5 años; mín: 1/máx 88). Un total de 53 (72,6%) casos correspondieron a linfadenopatía cervical, 11 (15%) a tuberculosis laríngea, 3 (4,1%) a tuberculosis hipofaríngea, y los restantes 6 en otras localizaciones. Del total, 14 (19,2%) pacientes eran VIH positivo y 10 (13,7%) tenían antecedentes de contacto con familiares que habían sufrido tuberculosis pulmonar. En 51 (69,8%) de los casos se realizó una PCR como medida de confirmación, siendo positiva en 47 de estos (92,1%).
ConclusiónLa similitud de la tuberculosis con enfermedades de mal pronóstico y la dificultad que entraña su diagnóstico hacen necesario tener en cuenta la tuberculosis a la hora de explorar a pacientes con lesiones granulomatosas o ulcerativas del área ORL. Al analizar nuestros resultados, la incidencia de tuberculosis según su localización en el área ORL es similar a la reportada en la literatura. Es importante hacer mención especial del uso de la PCR en nuestro estudio y las ventajas que su aplicación significa para el diagnóstico.