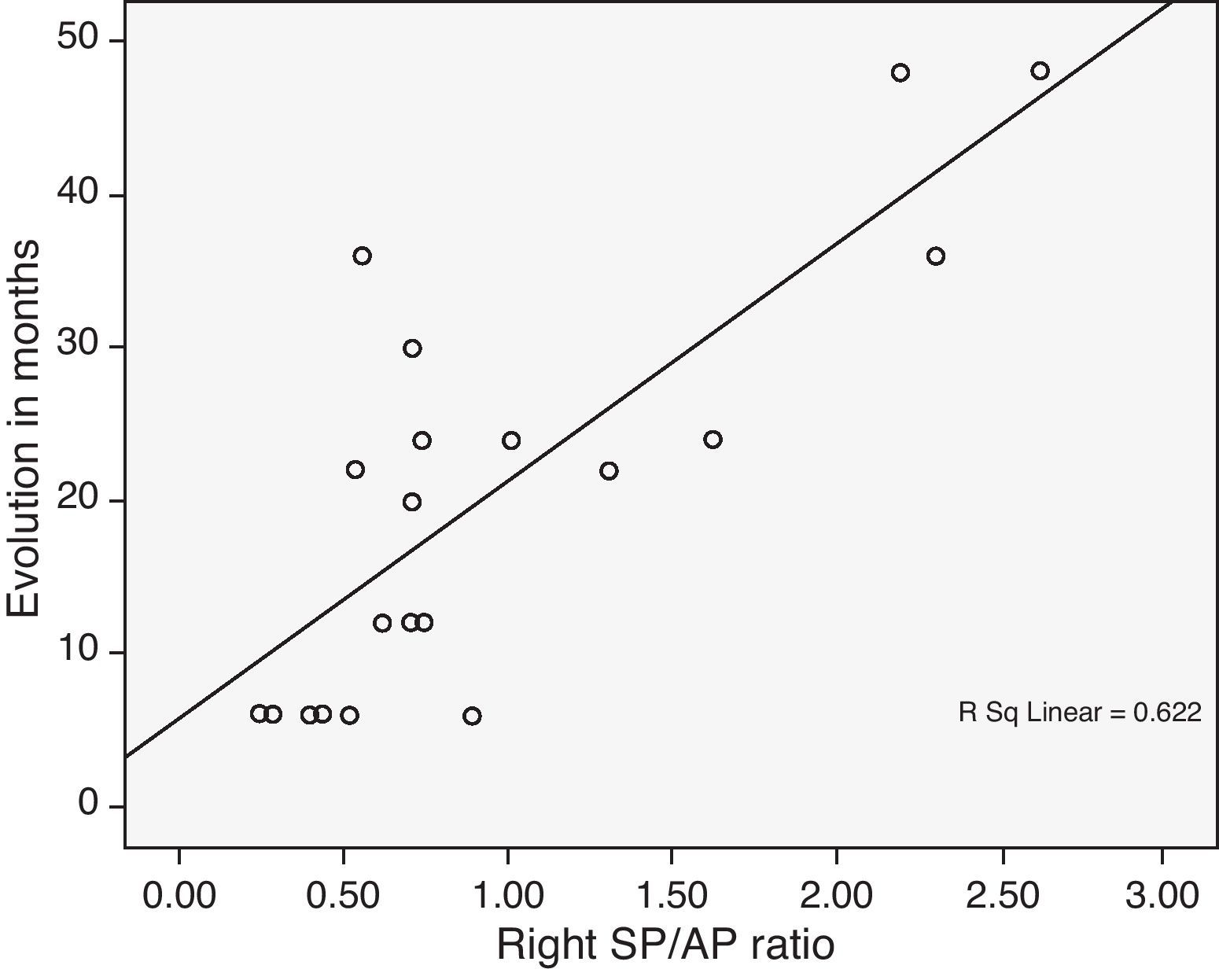
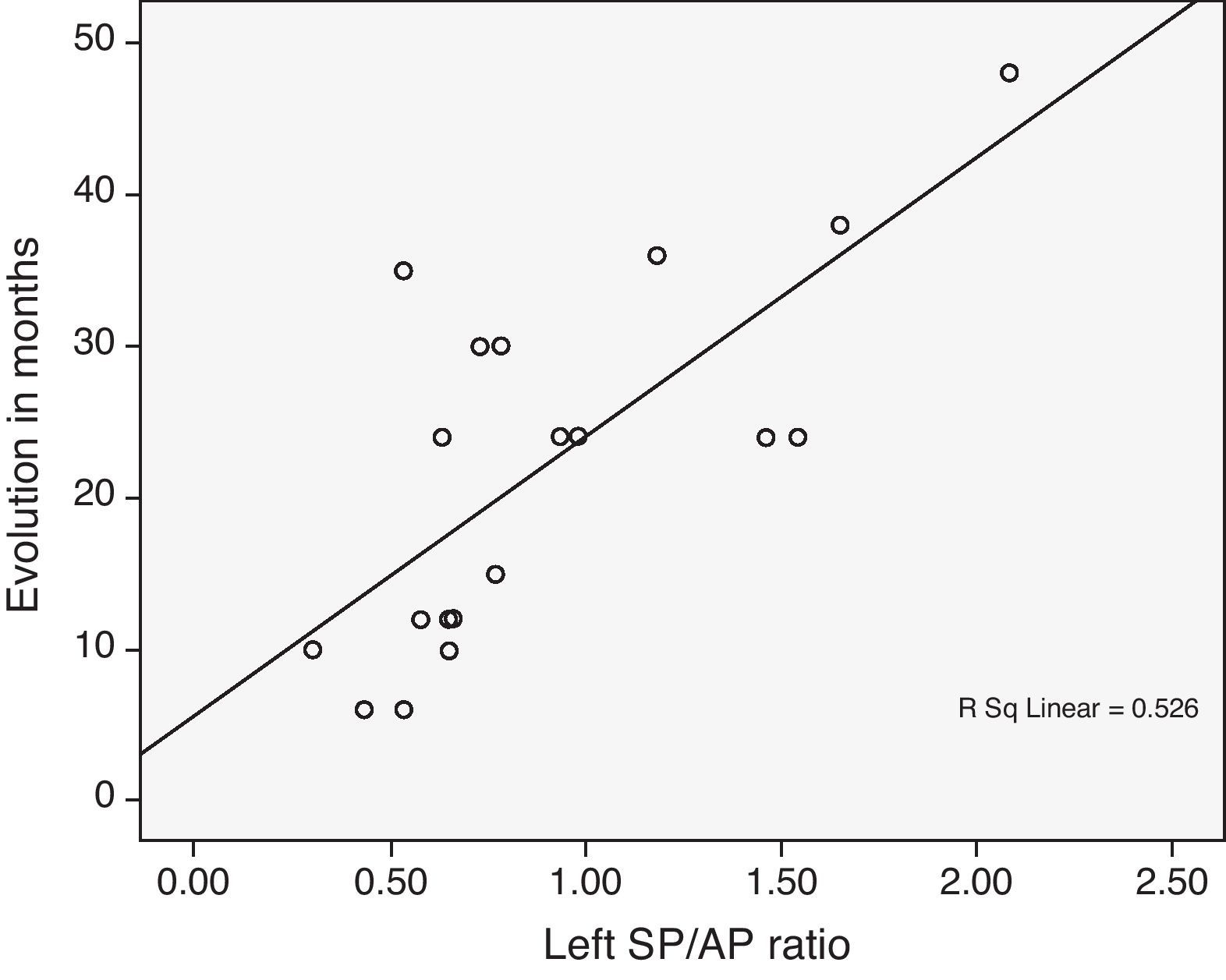
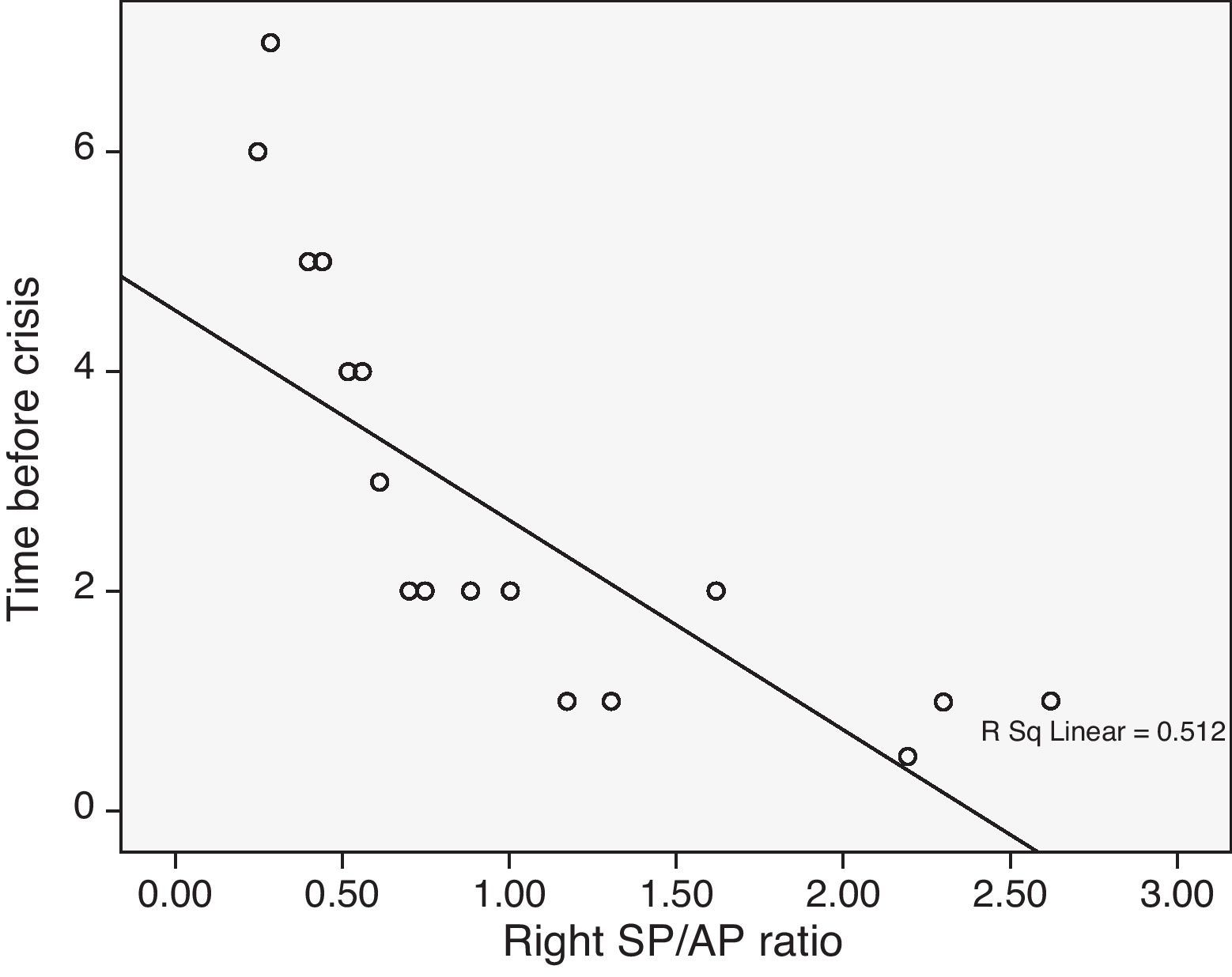
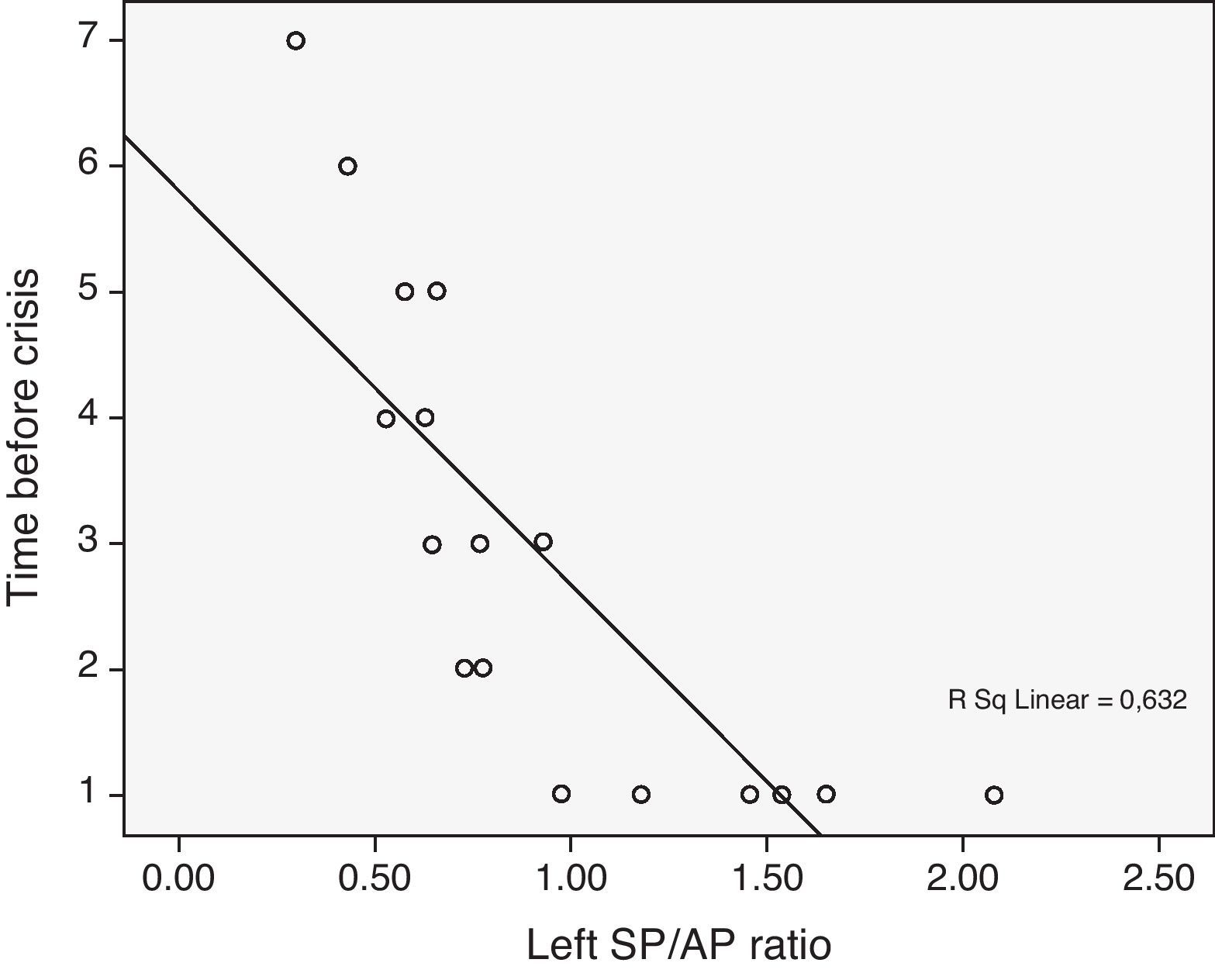
Electrocochleography is the registration of an electrophysiological event which takes place in the cochlea after an acoustical stimulus. Most of the authors consider an increased summating potential (SP)/action potential (AP) ratio as characteristic of endolymphatic hydrops.
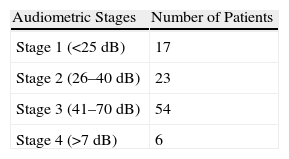
MethodsA longitudinal, prospective study of a unilateral Ménière's population diagnosed according to the American Academy of Otolaryngology–Head and Neck Surgery classification was carried out. A complete clinical history and bedside examination were performed, in addition to complete auditory and vestibular testing and an extratympanic electrocochleography. We selected 20 normal hearing subjects with no history of vestibular and otological pathology as a control group.
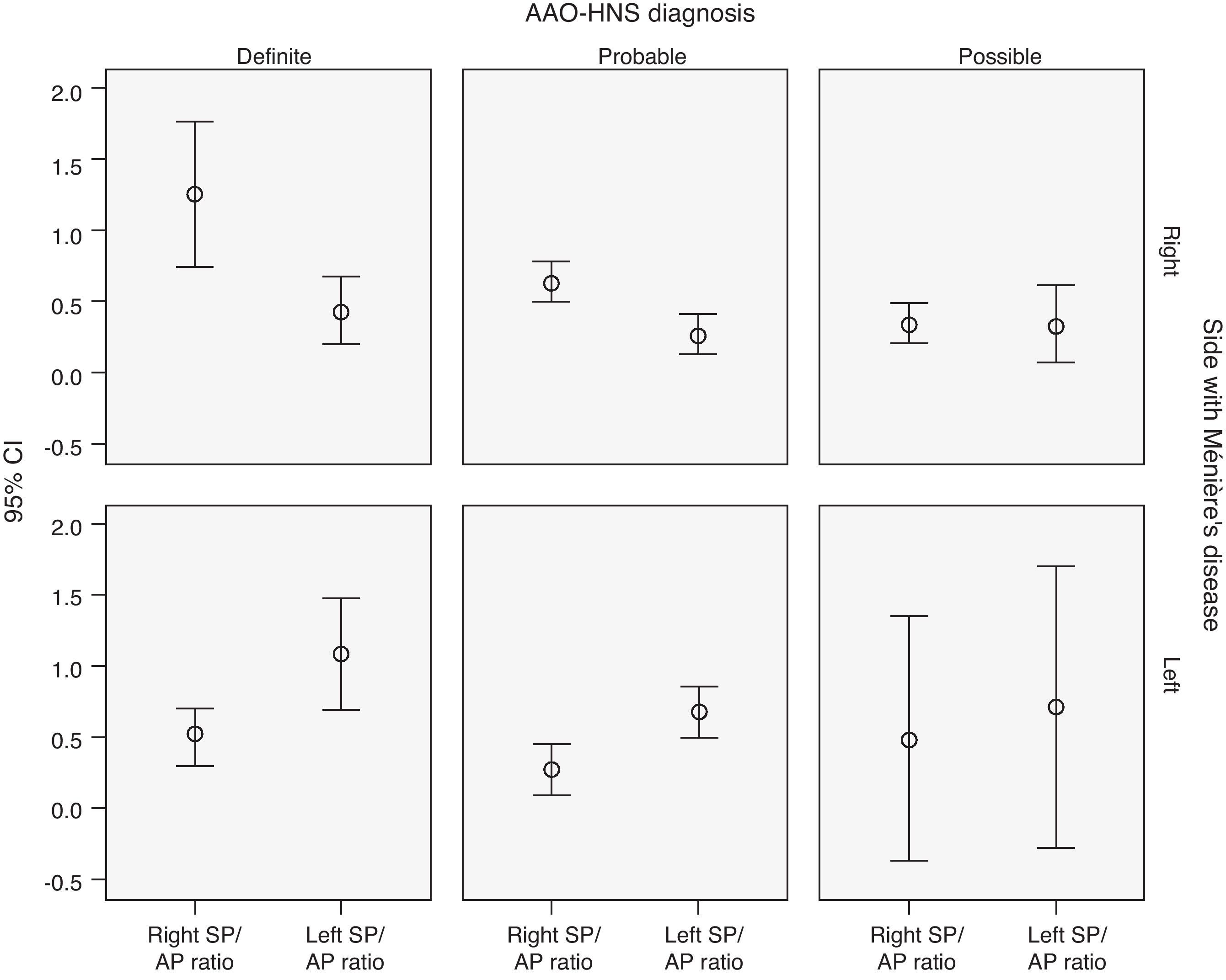
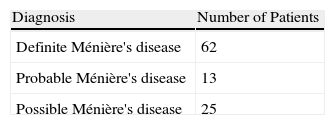
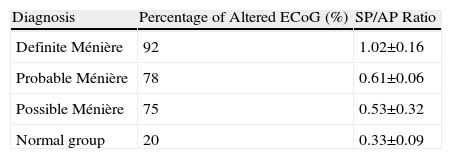
ResultsOf the 100 patients included in the study, 62 were diagnosed as definite Ménière's disease, and 13 and 25 as probable and possible Ménière's disease, respectively. In the electrocochleography, 85% of all the patients had an SP/AP ratio above 0.5. A sensibility of 92%, 78% and 75% was obtained in the definite, probable and possible Ménière's disease patients, respectively.
Discussion and conclusionsElectrocochleography is a useful method for diagnosing and evaluating patients with Ménière's disease syndrome. It provides information about the progression of the process and shows a significant correlation with the clinical stage.
La electrococleografía (ECoG) es un registro de un episodio electrofisiológico, que tiene lugar en la cóclea tras un estímulo acústico. La mayoría de los autores consideran que un aumento del cociente SP/AP utilizando clicks, es característico del hidrops.
MétodosPresentamos un estudio longitudinal y prospectivo de una población de pacientes con enfermedad de Ménière unilateral definida según los criterios de la Academia Americana de Otorrinolaringología y patología cervicofacial. Tras una correcta anamnesis y exploración otoneurológica completa, todos los pacientes fueron sometidos a un estudio de la función auditiva y vestibular mediante audiometría tonal liminar, pruebas calóricas, rotatorias y una ECoG extratimpánica. Como controles se escogieron 20 sujetos normoacúsicos carentes de antecedentes de afección vestibular u otológica, ni antecedentes quirúrgicos en el oído medio.
ResultadosDe los 100 pacientes incluidos, 62 fueron diagnosticados de enfermedad de Ménière definida, 13 de probable y 25 de enfermedad de Ménière posible. Un 85% de la población con enfermedad de Ménière, cumplían criterios electrofisiológicos de enfermedad de Ménière según los parámetros de la ECoG (SP/AP>0,5). El porcentaje de ECoG alteradas según el diagnóstico era del 92, 78 y 75% para el Ménière definido, probable y posible respectivamente.
Discusión y conclusionesLa ECoG es un método útil para el diagnóstico y evaluación de la enfermedad de Ménière. Aporta información fidedigna del progreso de la enfermedad y existe correlación con su estadio diagnóstico.