Deep neck infections (DNI) are potentially lethal processes and are susceptible to severe complications. This study shows an increment of the incidence and investigated the cause. More than 30% of cases are idiopathic, but they are commonly related to a dental or oropharyngeal infection.
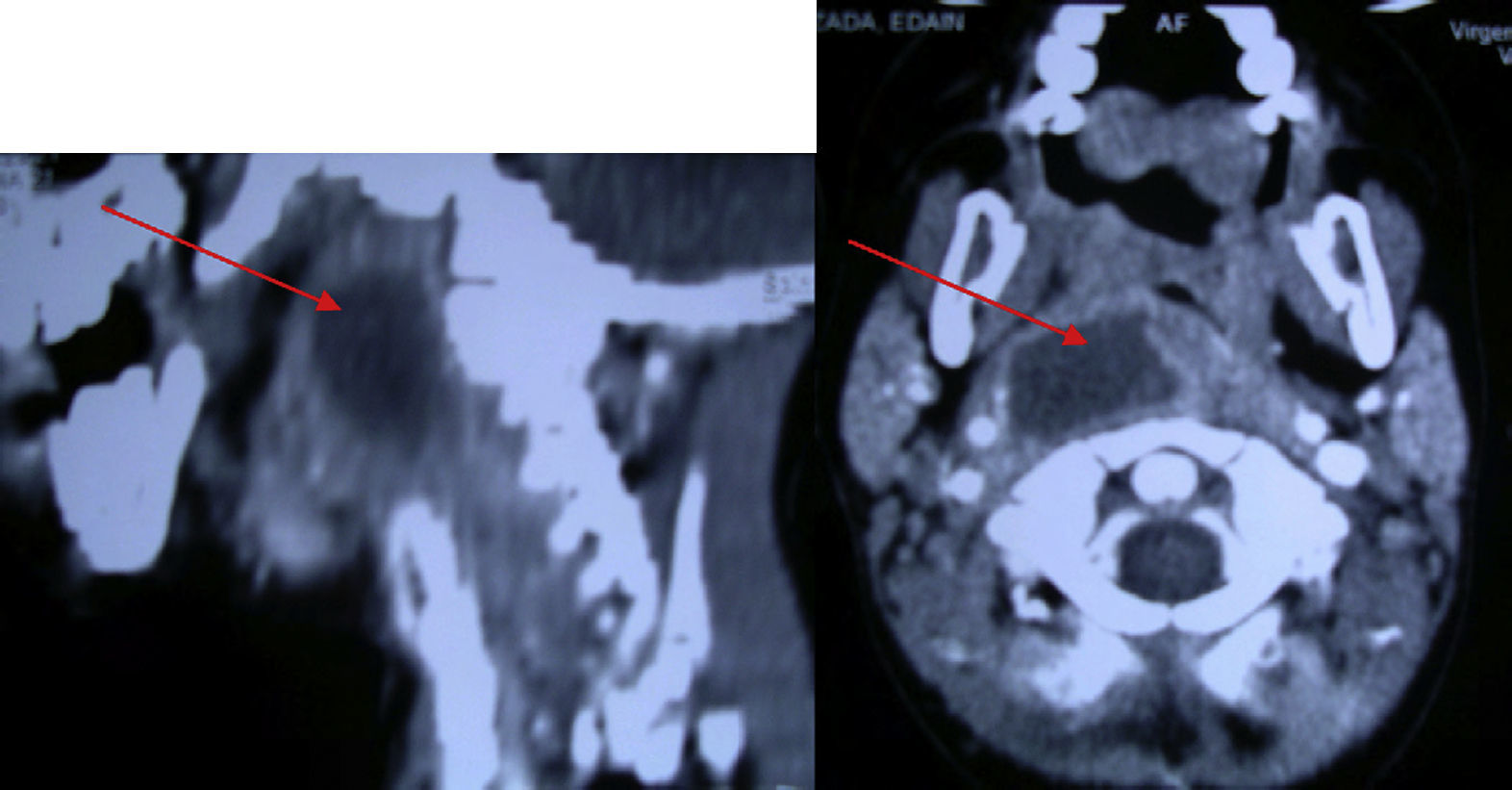
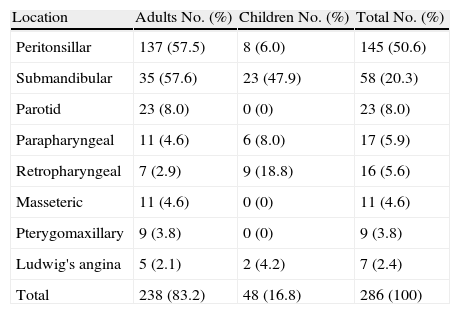
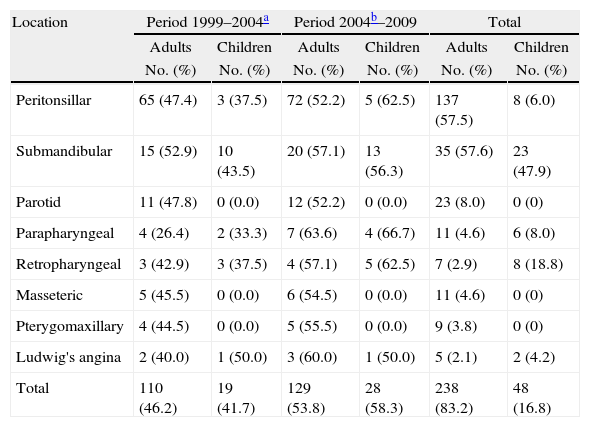
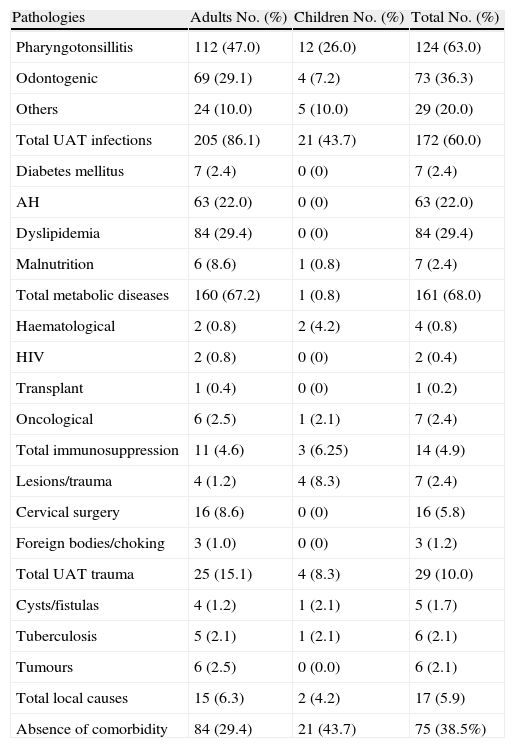
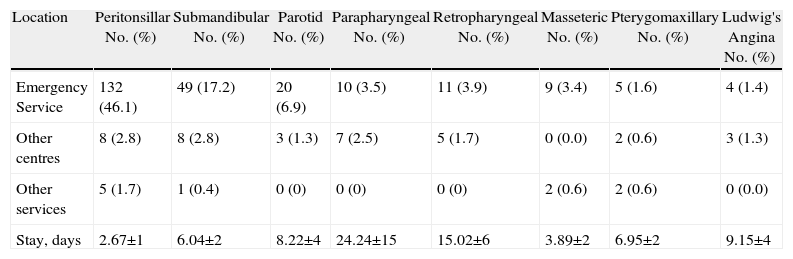
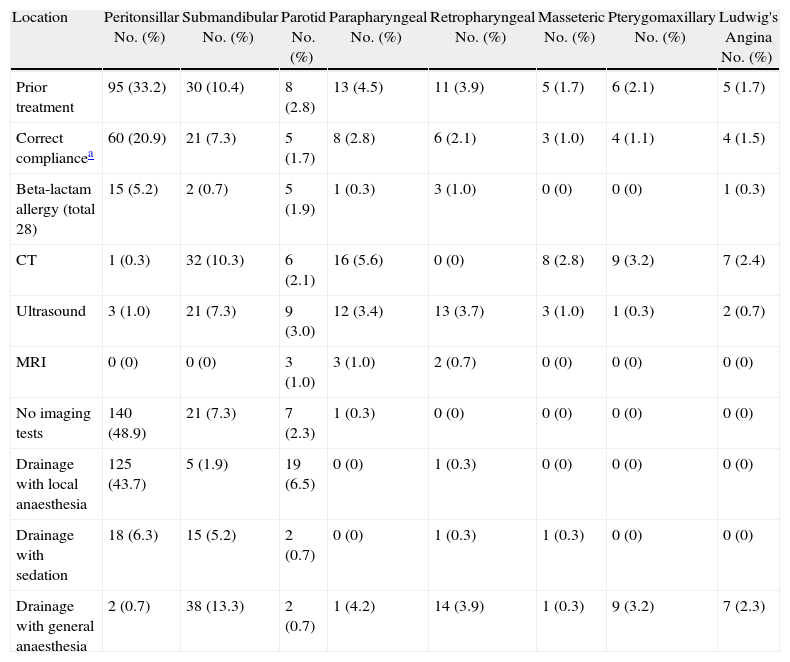
Material and methodsWe present 286 consecutive cases in a retrospective 11-year study. We analysed the clinical picture, antecedents and concurrent diseases, and diagnostic and therapeutic approaches that could be related to developing a DNI.
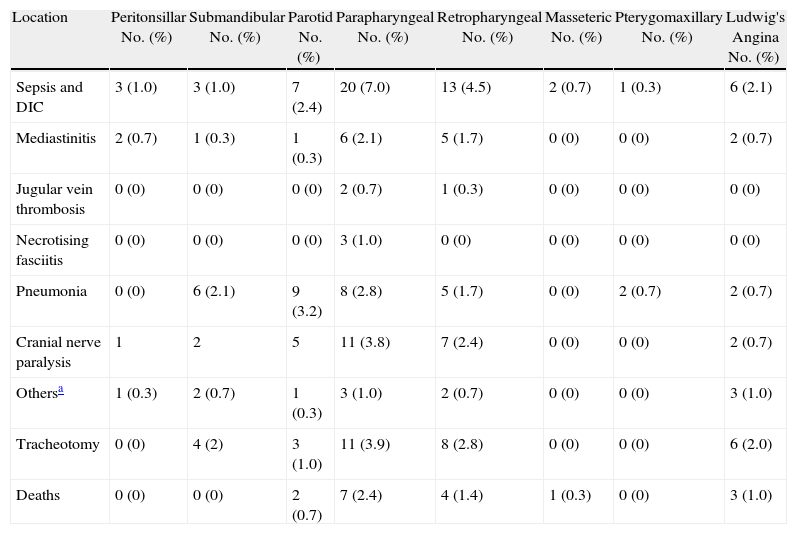
ResultsA major increase in DNI incidence in our setting was seen in the last few years. The major complications were mediastinitis, septic shock with disseminated intravascular coagulation syndrome, necrotising fasciitis and acute respiratory failure. A lower cranial nerve palsy that develops into dysphagia and leukoencephalopathy is the most frequent sequela. We found 10% of aspiration pneumonia. Mortality in adults was 5.9% and in children 6.2%.
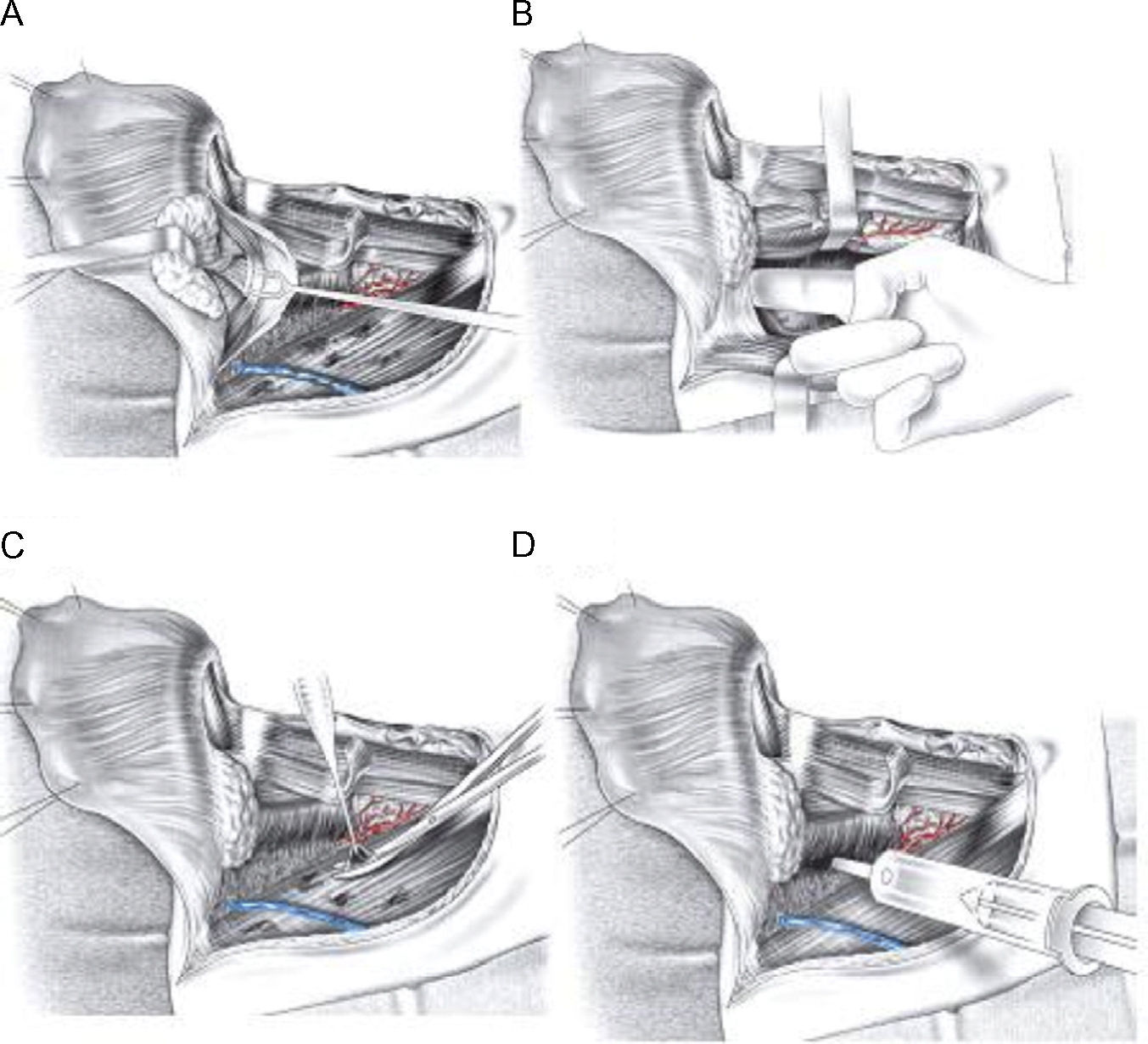
ConclusionsDeep neck infections constitute a medical and surgical emergency. Severe complications may arise in a short time. We must be vigilant to alarm symptoms such as dyspnoea, stridor, pain in the floor of the mouth, sialorrhoea, trismus, etc.
Improvements in antibiotic therapy, diagnostic imaging and critical patient support modalities have decreased mortality and there is a better prognosis, with complications being identified and treated earlier.
Las infecciones cervicales profundas (ICP) son afecciones potencialmente letales y susceptibles de complicaciones graves. En este estudio se constata el aumento de la incidencia y se trata de buscar las causas. Más del 30% son idiopáticas, pero suelen relacionarse con infecciones dentarias y orofaríngeas.
Material y métodosSe presentan 286 ICP consecutivas en un estudio retrospectivo de los últimos 11 años en nuestro centro y se analizan antecedentes y enfermedades concomitantes y aspectos diagnósticos y terapéuticos de los pacientes que pueden influir en el desarrollo de las ICP.
ResultadosSe objetiva un repunte de la incidencia de las ICP en nuestro medio. Las complicaciones más frecuentes fueron mediastinitis, shock séptico con coagulación intravascular diseminada, fascitis necrotizante y compromiso respiratorio agudo. Las secuelas más frecuentes observadas fueron la disfagia por parálisis de pares craneales bajos y neuroencefalopatía. Se produjeron un 10% de neumonías aspirativas. La mortalidad por ICP en los adultos es del 5,9% y en los niños del 6,2%.
ConclusionesLas ICP debe ser consideradas una urgencia médicoquirúrgica. Son susceptibles de complicaciones graves en cuestión de horas. Debemos estar atentos a la aparición de síntomas de alarma como: disnea, estridor, dolor a la palpación en el suelo de la boca, sialorrea, trismus, etc.
El avance en los diversos procedimientos diagnósticos (imagen, microbiología) y terapéuticos (antibióticos, cirugía), así como la mejor atención del paciente crítico (UCI- REA), han sido decisivos en el diagnóstico y tratamiento precoz, identificar y tratar las complicaciones y mejorar el pronóstico y la mortalidad de los pacientes.