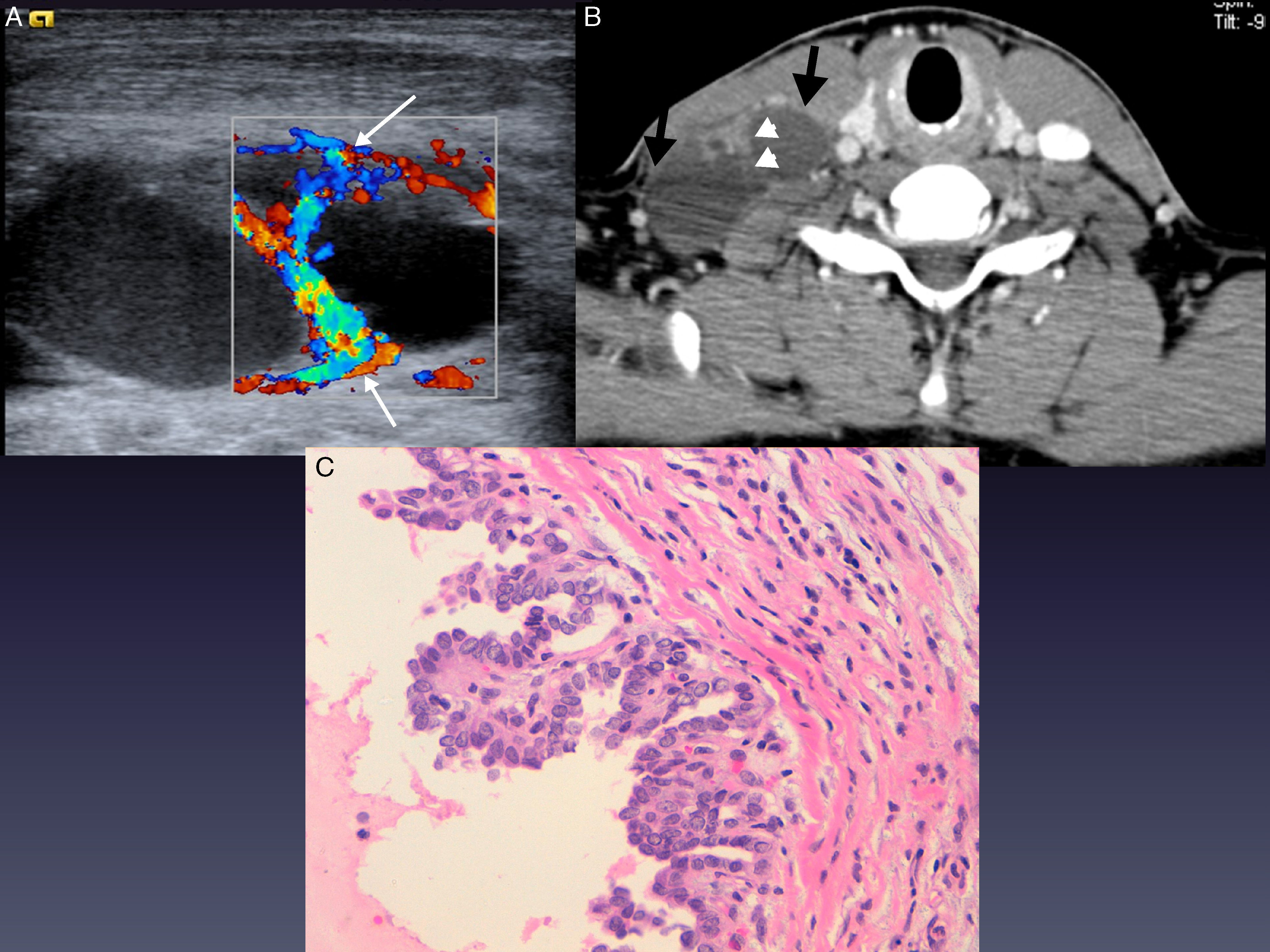
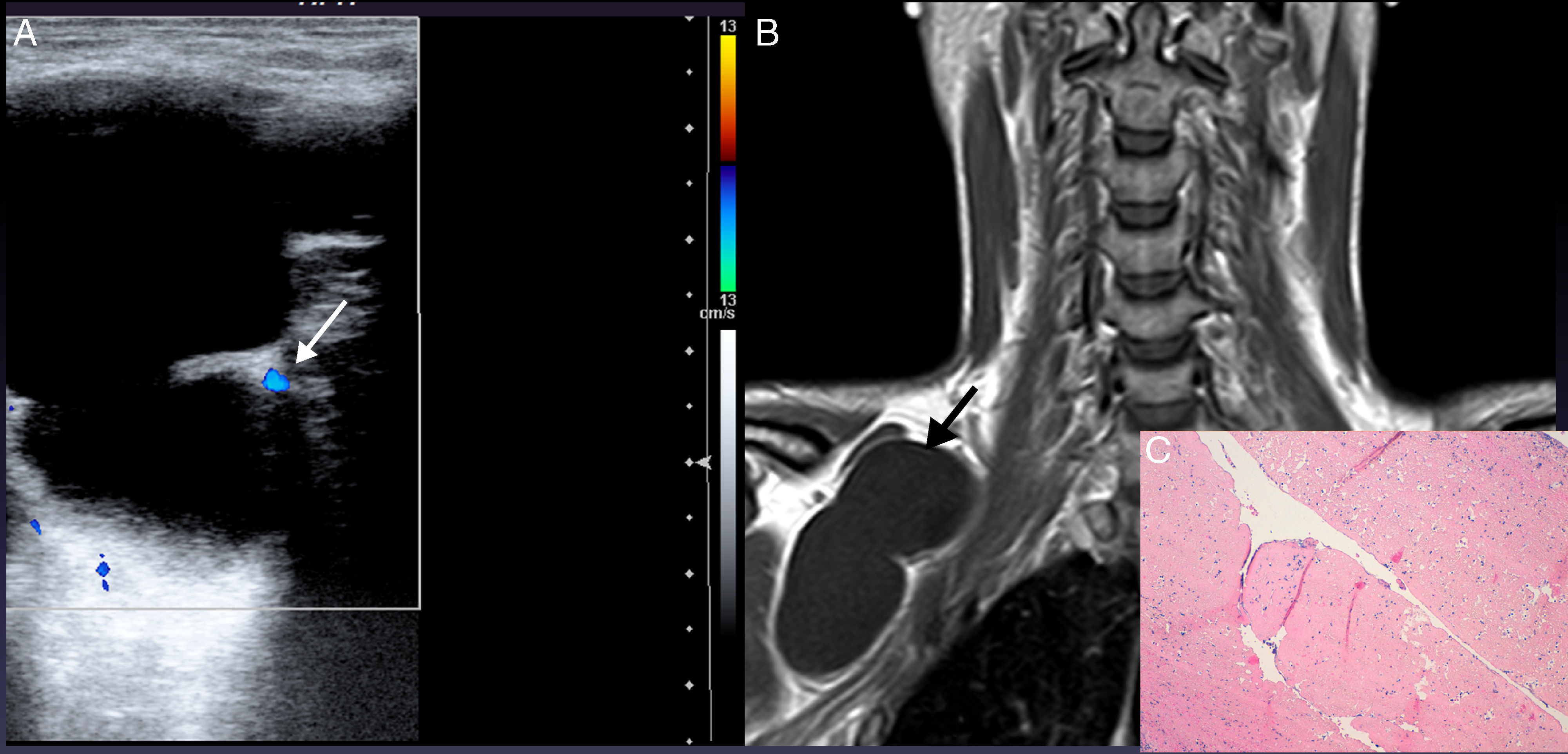
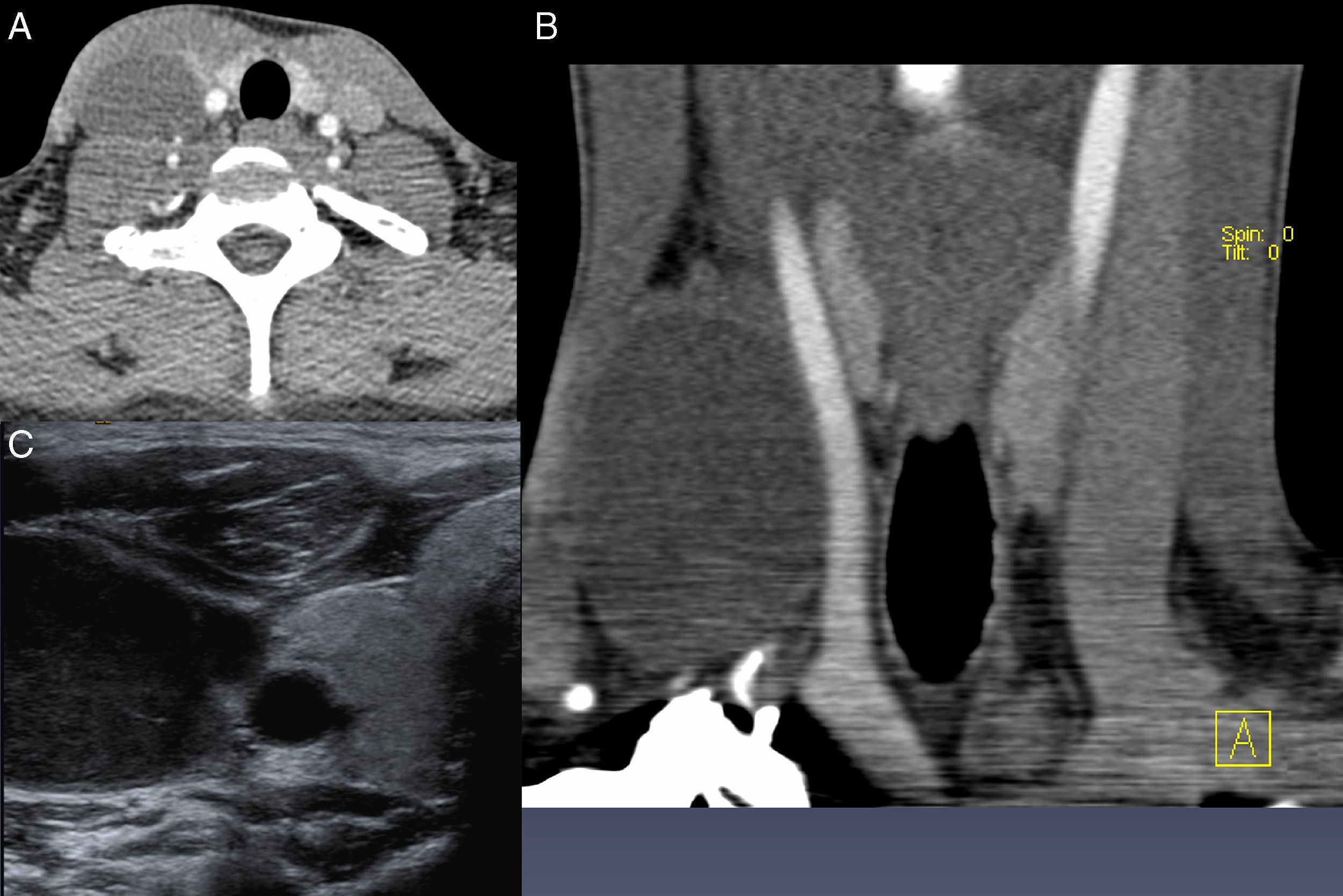
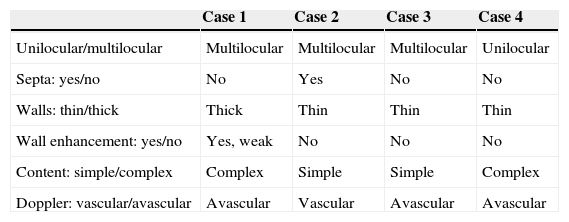
Cystic lesions of the posterior triangle are a pathologic entity whose diagnosis is made in the first two years of life. Its presentation in adulthood is an incidental finding and the differential diagnosis includes cystic lymphangioma, lymphatic metastasis of thyroid cancer and branchial cyst. Often with the finding of a cervical lump, FNA is made before diagnostic imaging is performed, however, this procedure is not always advisable. We reviewed the cases of patients who came last year to our department with a cystic mass in this location and correlating the imaging findings with pathologic specimen.
We show characteristic findings of these lesions in order to make an early diagnosis and thus to get the approach and treatment appropriate of adult patients with a cystic lesion in the posterior cervical triangle.
Las lesiones quísticas del triángulo posterior forman una entidad patológica cuyo diagnóstico se realiza en los 2 primeros años de vida. Su presentación en la edad adulta es un hallazgo ocasional y su diagnóstico diferencial incluye el linfangioma quístico, las metástasis linfáticas del cáncer de tiroides y el quiste branquial. Con frecuencia, ante el hallazgo de una tumoración cervical se realiza PAAF previa a la imagen diagnóstica, sin embargo, este procedimiento no siempre es el aconsejable. Hemos revisado los casos de pacientes que acudieron en este último año a nuestro servicio con lesiones en esta localización correlacionando los hallazgos de imagen con los resultados anatomopatológicos.
Mostramos los hallazgos de imagen característicos de estas entidades con el fin de realizar un diagnóstico precoz que permita el abordaje y tratamiento adecuado del paciente adulto con una lesión quística en el triángulo cervical posterior.