Foreign body aspiration in childhood is a common and potentially serious problem. Complications may be the result of the aspiration episode itself, delayed diagnosis or treatment. We describe our experience in a paediatric hospital in Argentina.
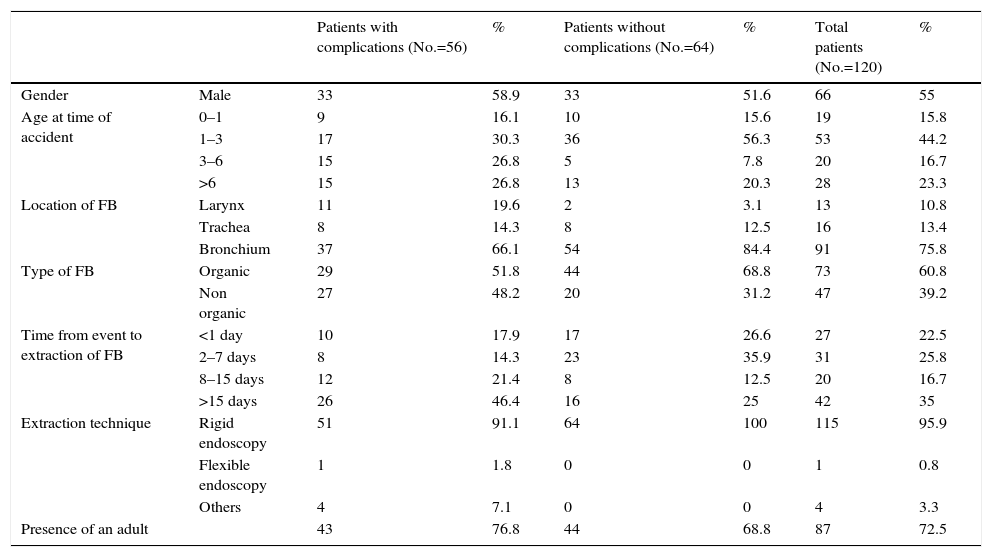
MethodsWe retrospectively evaluated 56 patients with complications due to foreign body aspiration recorded in the Susy Safe Project between January 2010 and November 2013. The clinical variables analysed were sex, age at time of aspiration, foreign body location and type, time elapsed from the event until object removal, extraction technique, complications, need for hospitalisation and circumstances of the event.
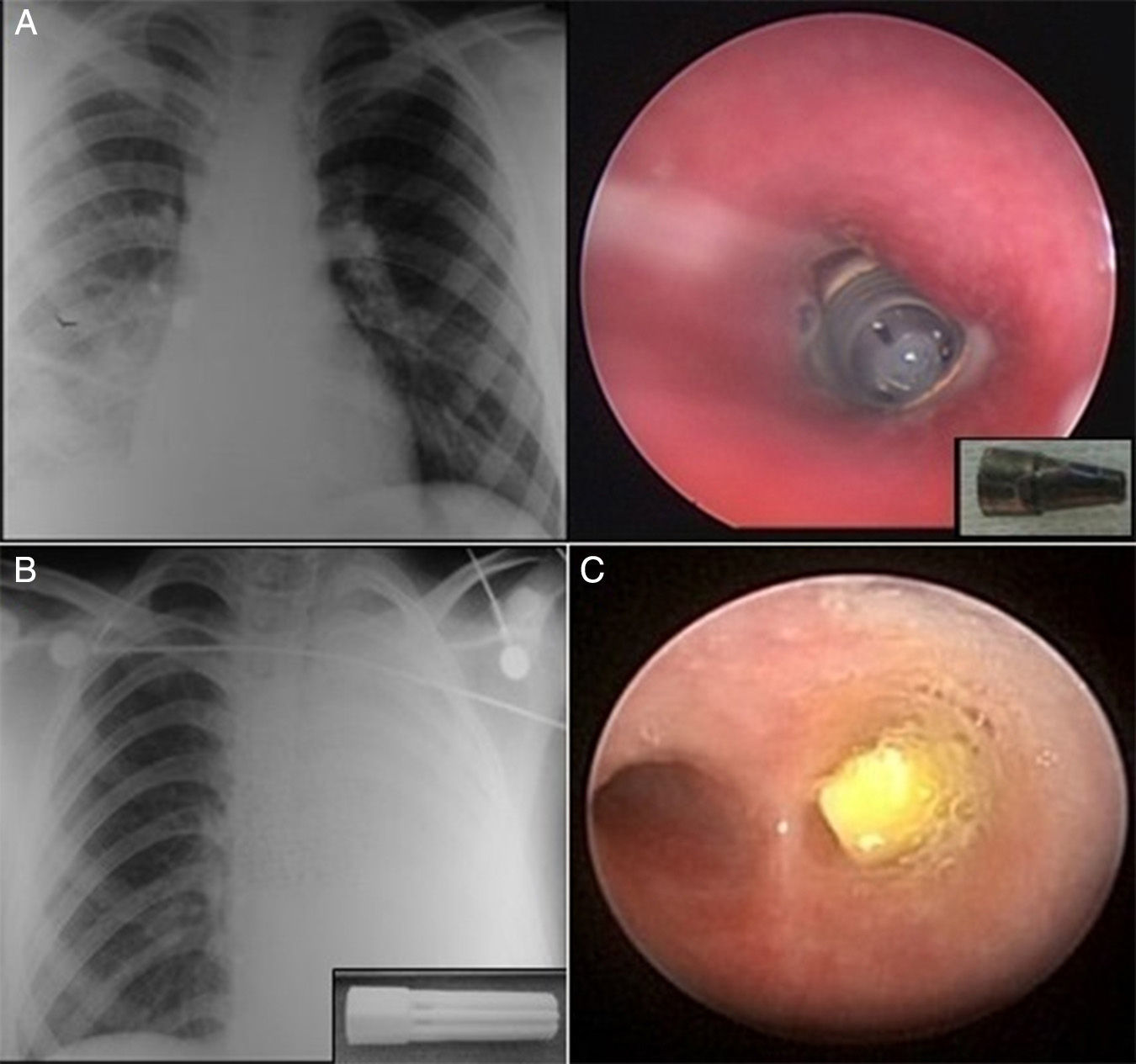
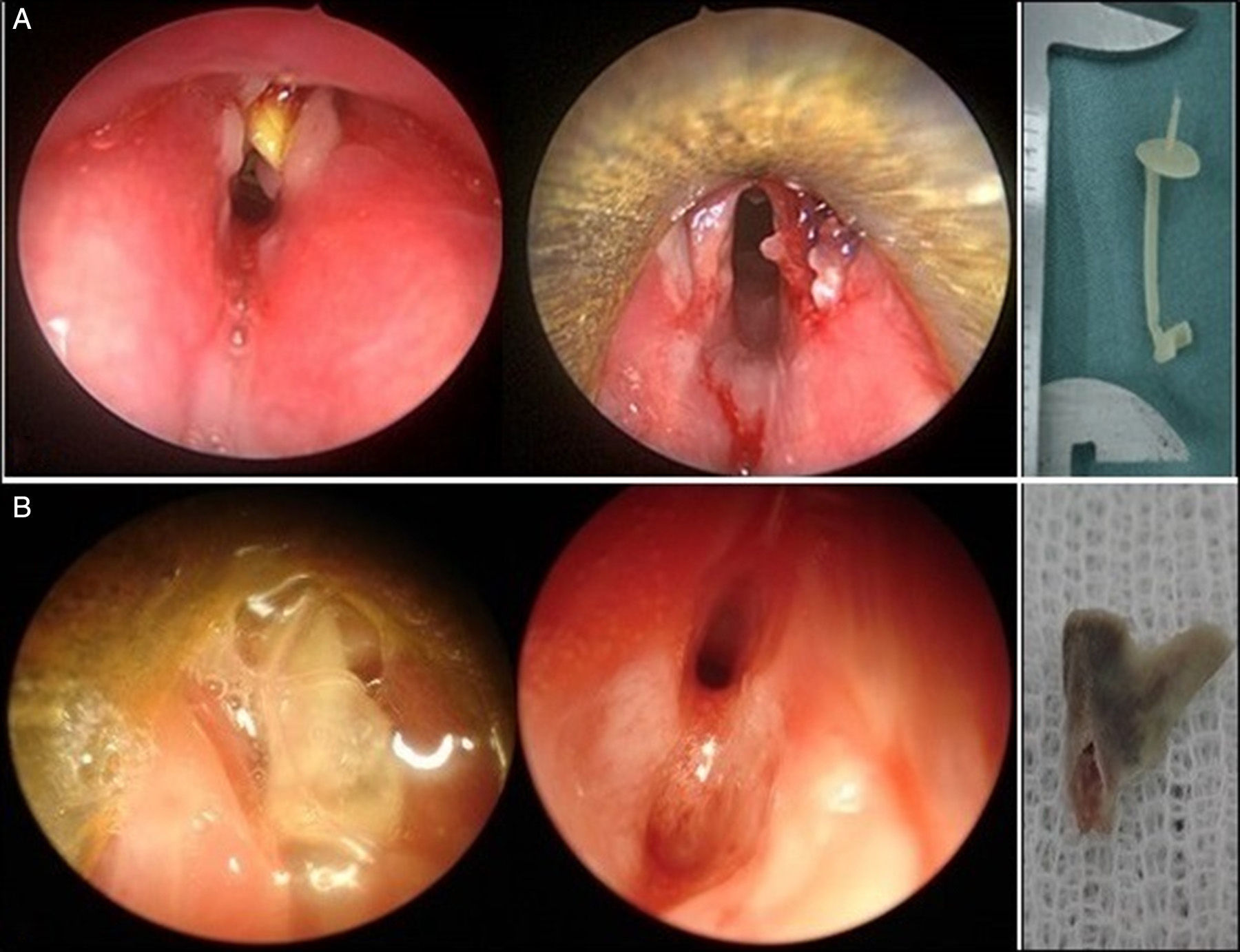
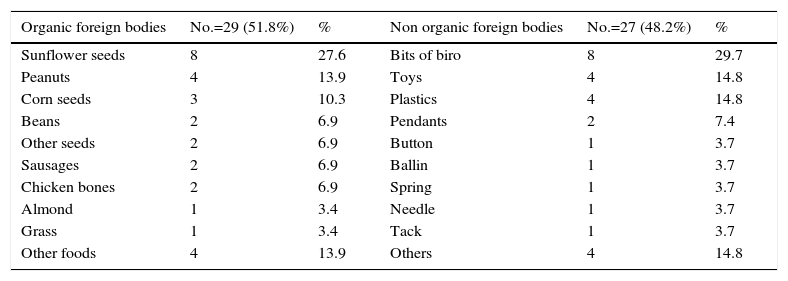
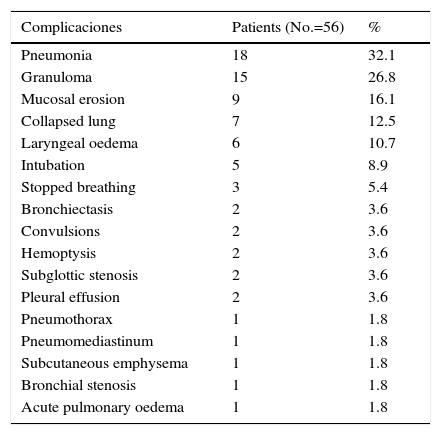
Results58.9% of the cases described occurred in males, with high presence of adults (76.8%) at the time of aspiration. The incidence was slightly higher in children older than 3 years. In 37 cases (66.1%), the foreign body was located in bronchus; sunflower seeds and ballpoint caps were the most common foreign objects. Only in 10 cases (17.9%) was the object extracted within 24hours of the event. The most common complications were pneumonia (18 cases), granuloma (15 cases) and mucosal erosion (9 cases). Hospitalisation was necessary for 41 patients.
ConclusionEarly diagnosis and immediate control through specialised teams are essential to ensure proper treatment, usually endoscopic, without risk of complications.
La aspiración de cuerpos extraños en niños es un problema frecuente y potencialmente grave. Las complicaciones pueden ser consecuencia tanto del propio episodio aspirativo como del retraso en el diagnóstico o de la terapéutica empleada. Describimos nuestra experiencia en un hospital pediátrico de Argentina.
MétodosSe evaluaron de forma retrospectiva 56 niños con complicaciones por cuerpo extraño en la vía aérea registrados en el Proyecto Susy Safe entre enero de 2010 y noviembre de 2013. Las variables analizadas fueron el sexo, la edad en el momento de la aspiración, la localización y el tipo de cuerpo extraño, el tiempo transcurrido desde el evento hasta la extracción del objeto, la técnica de extracción, las complicaciones, la necesidad de hospitalización y las circunstancias del evento.
ResultadosEl 58,9% de las complicaciones ocurrieron en varones, con alta presencia de adultos (76,8%) en el momento del accidente. La incidencia fue levemente mayor en mayores de 3 años. En 37 casos (66,1%) el cuerpo extraño se localizó en bronquio, siendo los más frecuentes las semillas de girasol y las partes de bolígrafo. Solo en 10 casos (17,9%) se extrajo el objeto dentro de las 24h del evento. Las complicaciones más comunes fueron la neumonía (18 casos), el granuloma (15 casos) y la erosión mucosa (9 casos). Fueron hospitalizados 41 pacientes.
ConclusiónUn diagnóstico precoz y un control inmediato a través de un equipo especializado son indispensables para garantizar un tratamiento apropiado sin riesgo de complicación.