The risk of producing bilateral laryngeal paralysis (BLP) in total thyroidectomy (TT) is low, but it is a concern for the surgeon and a serious safety incident that may compromise the airway, require reintubation or tracheostomy and cause serious sequelae or death. Neuromonitoring (NM), as an early diagnostic tool for the existence of injury to the recurrent laryngeal nerve (RLN), has not been shown to have reduced the risk, even though published series show lower incidences. Our objective was to estimate the risk of bilateral RLN paralysis with and without NM TT by systematic review and meta-analysis.
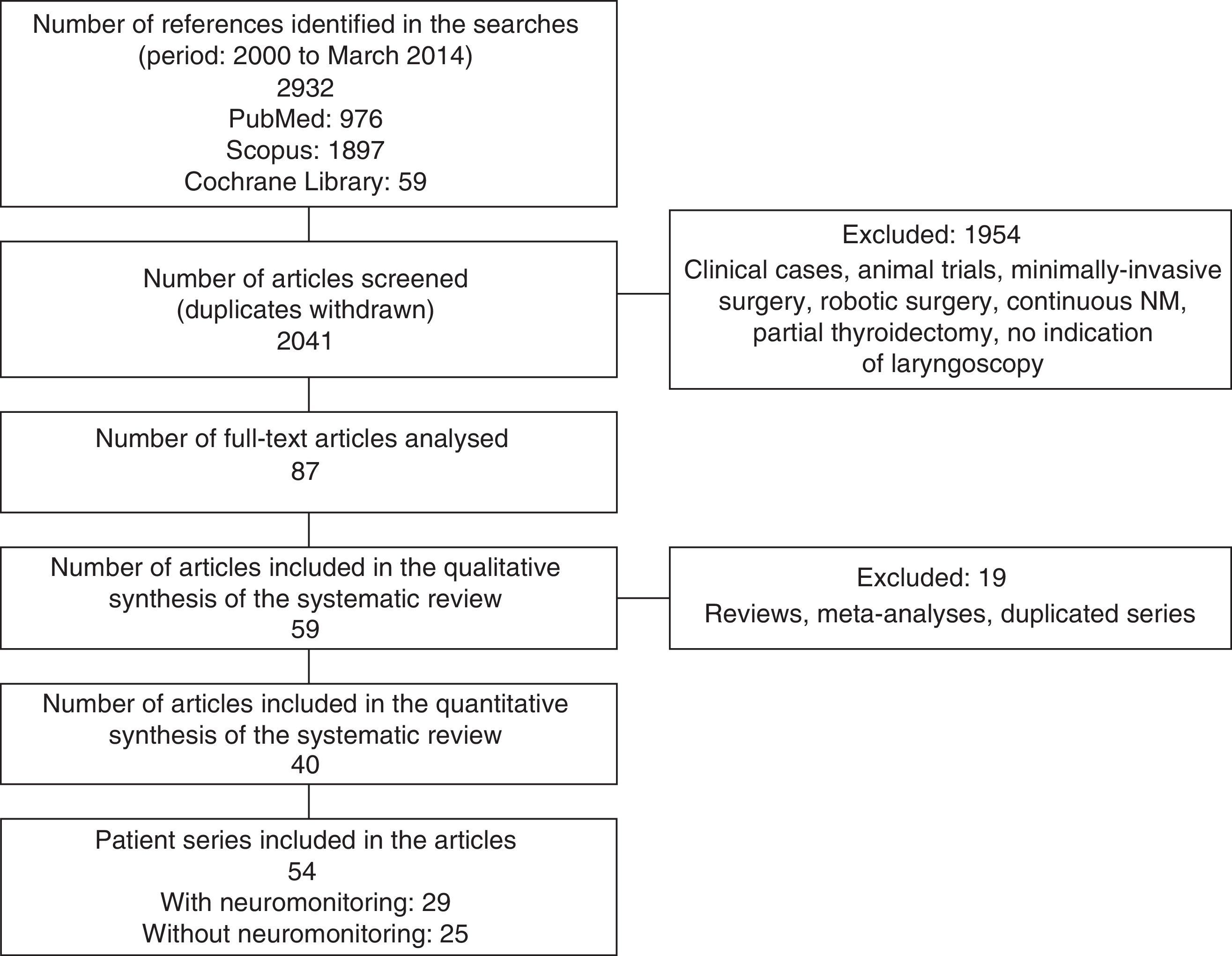
MethodWe performed a systematic review of clinical trials, cohort studies and case series with total thyroidectomy without NM published in the period 2000–2014. A database search was performed using PubMed, Scopus (EMBASE) and the Cochrane Library. Heterogeneity between studies was explored and weighted risks grouped according to random effects models were estimated.
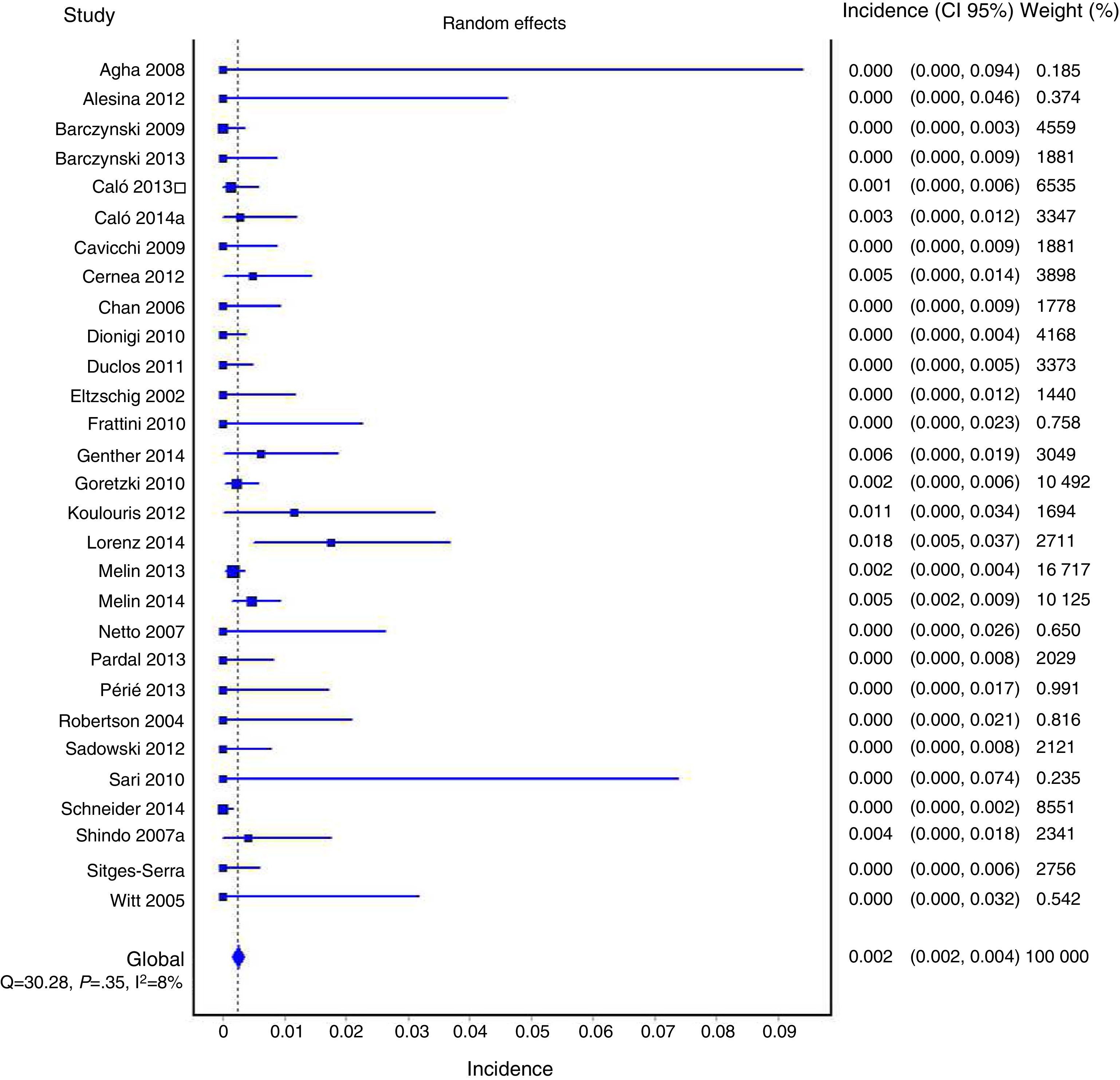
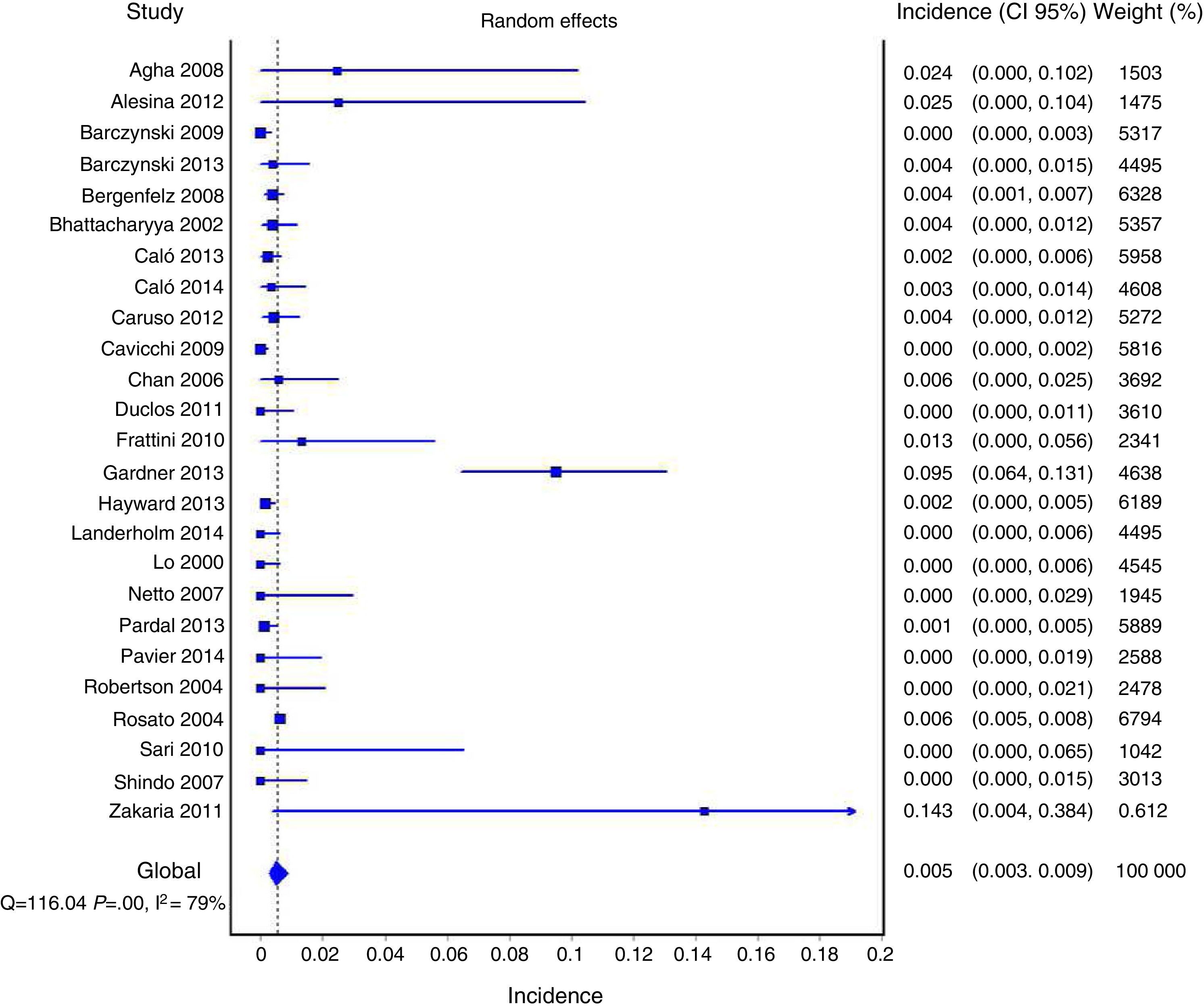
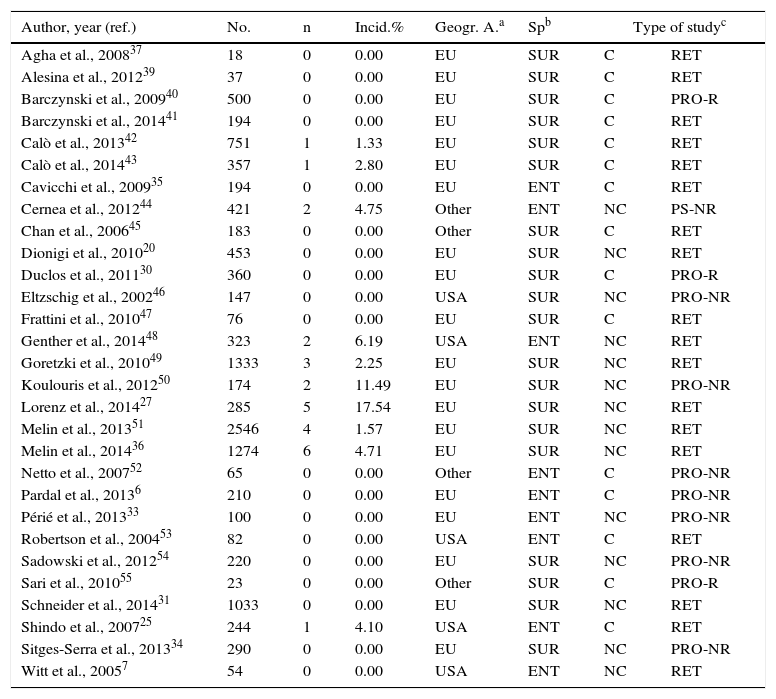
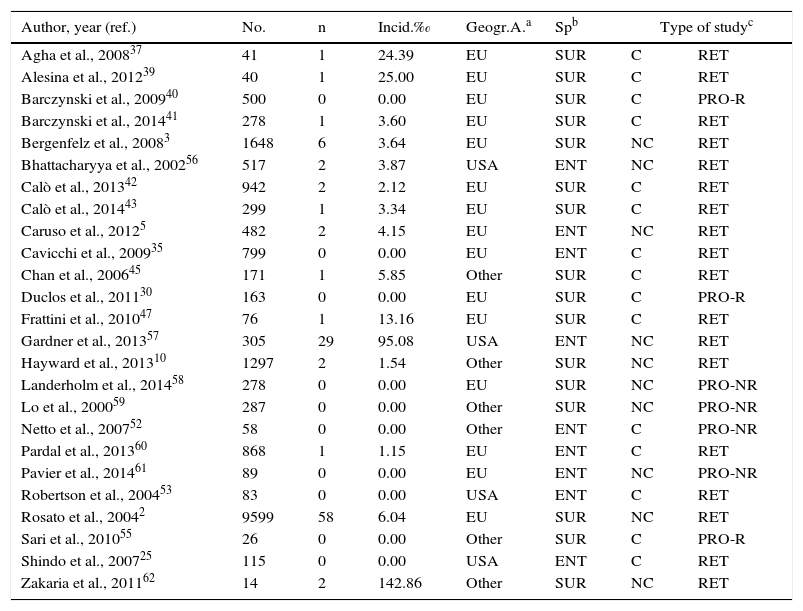
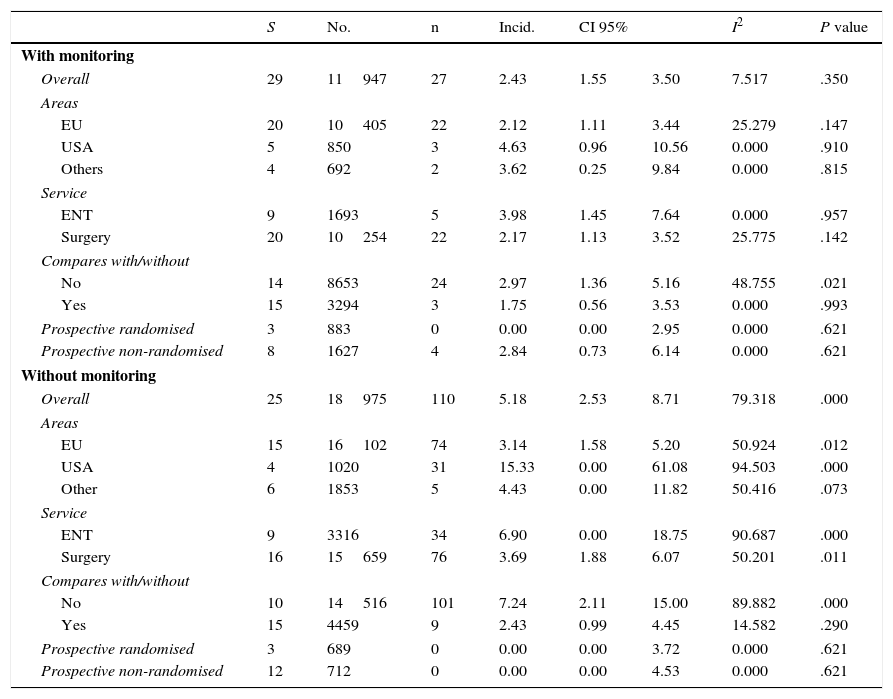
ResultsWe selected 40 articles and estimates of risk were identified in 54 case series (without NM, 25; with NM, 29) with 30922 patients.
The prevalence of BLP in the series with NM was lower compared to that without NM (2.43‰ [1.55–3.5‰] versus 5.18‰ [2.53–8.7‰]). This difference is equivalent to an absolute risk reduction of 2.75‰ with a number needed to treat of 364.13. The NM group was more homogeneous (I2=7.52%) than those without NM (I2=79.32%). The observed differences in the subgroup analysis were very imprecise because the number of observed paralysis was very low.
ConclusionsThe risk of bilateral paralysis is lower in studies with neuromonitoring.
El riesgo de parálisis laríngea bilateral (PLB) tras tiroidectomía total (TT) es bajo pero una de las mayores preocupaciones del cirujano y un incidente de seguridad grave que puede comprometer la vía aérea, precisar reintubación o traqueotomía y provocar secuelas graves o la muerte. No se ha demostrado que la neuromonitorización (NM) como herramienta diagnóstica precoz de lesión del nervio laríngeo recurrente (NLR) reduzca el riesgo. Objetivo: estimar el riesgo de PLB con y sin NM en TT mediante revisión sistemática y metaanálisis.
MétodoRevisión sistemática de ensayos clínicos, estudios de cohortes y series de casos de TT con y sin NM publicados en el periodo 2000–2014 en PubMed, Scopus (EMBASE) y Cochrane Library. Se exploró la heterogeneidad entre estudios y se estimaron riesgos ponderados agrupados siguiendo modelos de efectos aleatorios.
ResultadosSe seleccionaron 40 artículos con estimaciones del riesgo en 54 series (25 sin NM, 29 con NM) con 30.922 pacientes. La incidencia de PLB con NM resultó inferior que sin NM (2,43‰ [1,55–3,5‰] versus 5,18‰ [2,53–8,7‰]). Esta diferencia equivale a una reducción absoluta del riesgo de 2,75‰ y un número necesario de pacientes a tratar de 364,13. El grupo con NM resultó más homogéneo (I2=7,52%) que sin NM (I2=79,32%). Las diferencias del análisis por subgrupos fueron imprecisas por el escaso número de parálisis.
ConclusionesEl riesgo de PLB es menor en los estudios con neuromonitorización.