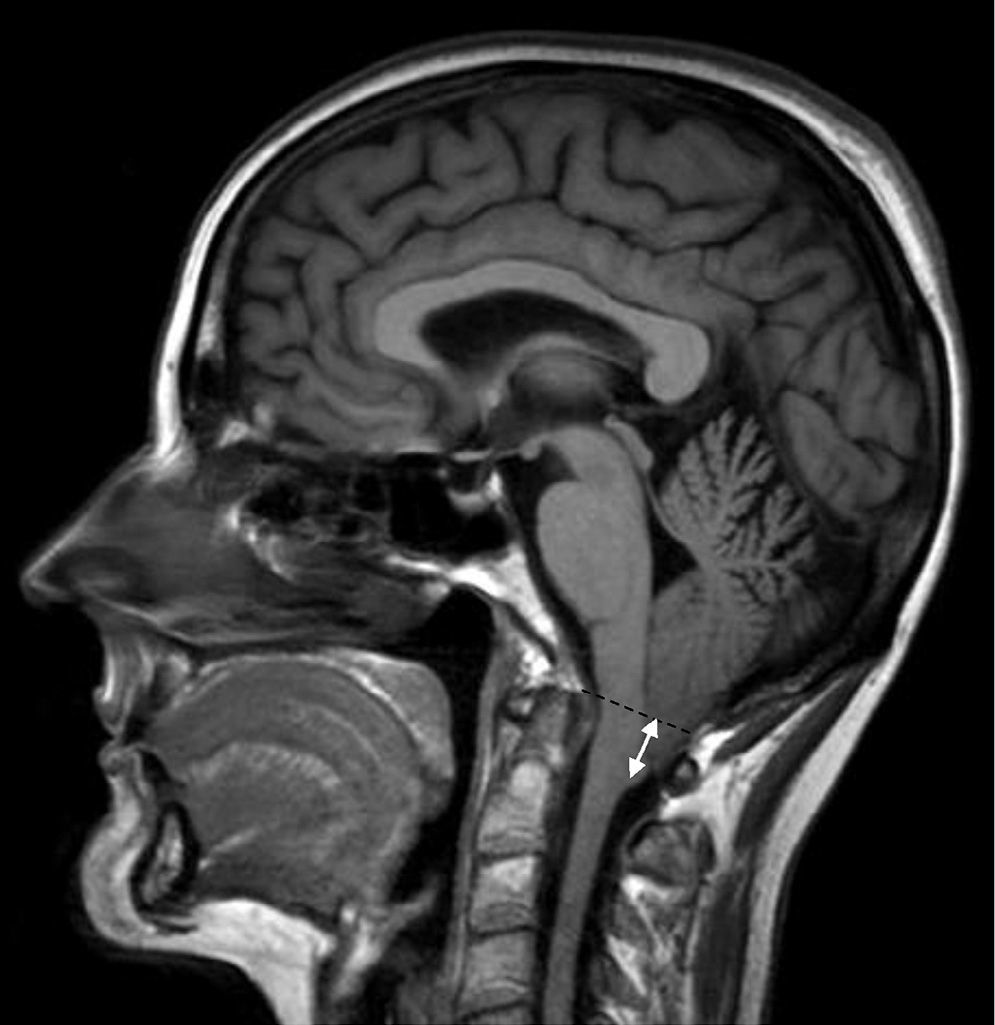
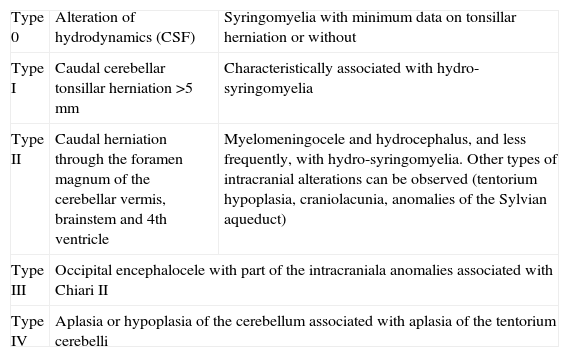
Chiari malformation is an alteration of the base of the skull with herniation through the foramen magnum of the brain stem and cerebellum. Although the most common presentation is occipital headache, the association of audio-vestibular symptoms is not rare. The aim of our study was to describe audio-vestibular signs and symptoms in Chiari malformation type I (CM-I).
Materials and methodsWe performed a retrospective observational study of patients referred to our unit during the last 5 years. We also carried out a literature review of audio-vestibular signs and symptoms in this disease.
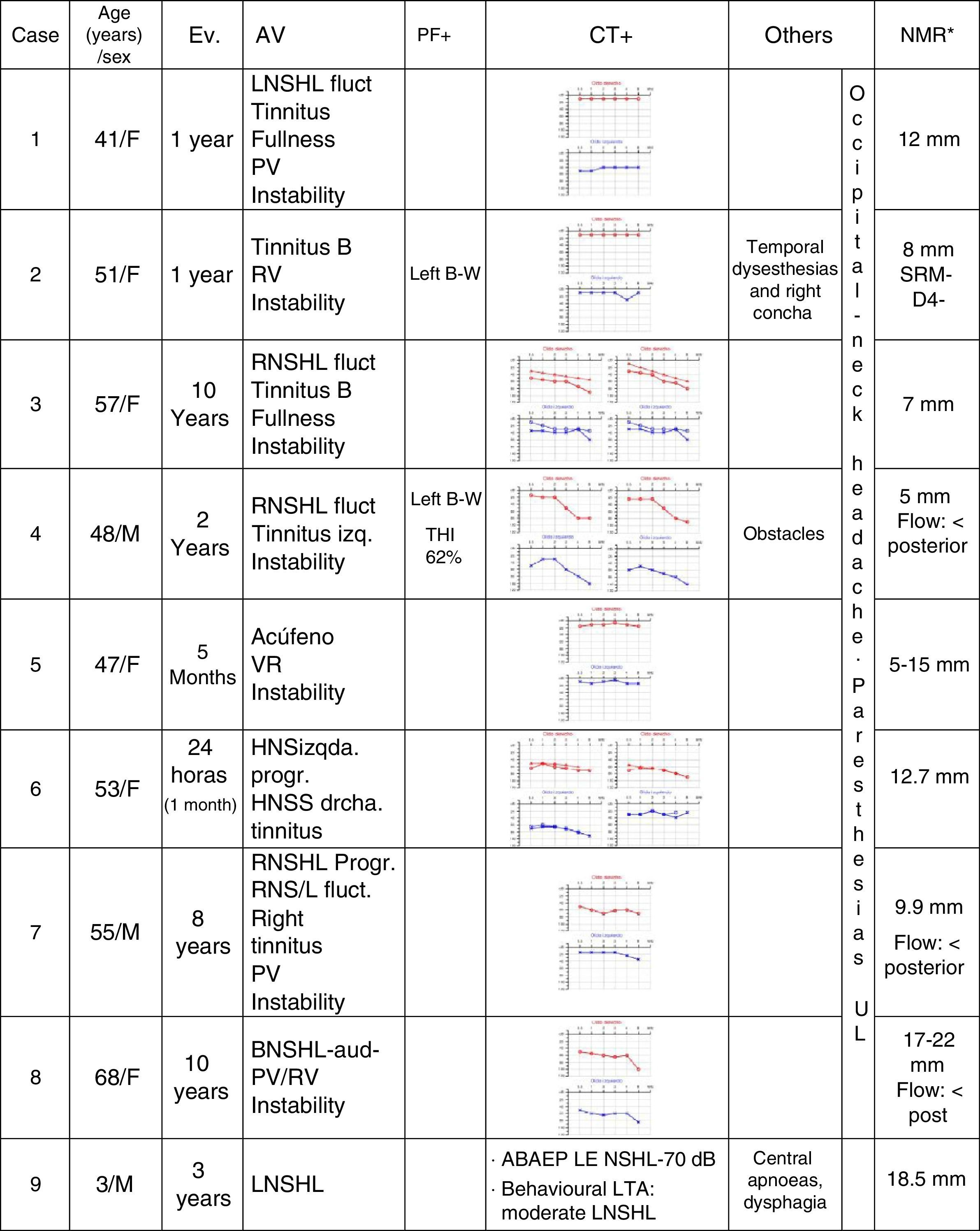
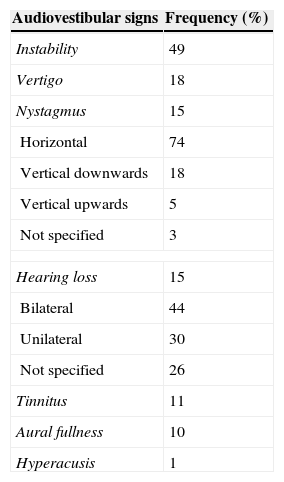
ResultsThere were 9 patients (2 males and 7 females), with an average age of 42.8 years. Five patients presented a Ménière-like syndrome; 2 cases, a recurrent vertigo with peripheral features; 1 patient showed a sudden hearing loss; and 1 case suffered a sensorineural hearing loss with early childhood onset. The most common audio-vestibular symptom indicated in the literature in patients with CM-I is unsteadiness (49%), followed by dizziness (18%), nystagmus (15%) and hearing loss (15%). Nystagmus is frequently horizontal (74%) or down-beating (18%). Other audio-vestibular signs and symptoms are tinnitus (11%), aural fullness (10%) and hyperacusis (1%). Occipital headache that increases with Valsalva manoeuvres and hand paresthesias are very suggestive symptoms.
ConclusionsThe appearance of audio-vestibular manifestations in CM-I makes it common to refer these patients to neurotologists. Unsteadiness, vertiginous syndromes and sensorineural hearing loss are frequent. Nystagmus, especially horizontal and down-beating, is not rare. It is important for neurotologists to familiarise themselves with CM-I symptoms to be able to consider it in differential diagnosis.
La malformación de Chiari es una alteración de la base del cráneo, en la que se produce herniación del cerebelo y del tronco cerebral a través del foramen magnum. Aunque su forma de presentación más frecuente es la cefalea occipitonucal, no es rara la asociación de síntomas audiovestibulares. El objetivo de nuestro estudio fue conocer las manifestaciones audiovestibulares en la malformación de Chiari tipo i (MCH-I).
Material y métodosSe realizó un estudio retrospectivo observacional de los pacientes remitidos a nuestra unidad en los últimos 5 años, así como una revisión bibliográfica de las manifestaciones audiovestibulares de esta enfermedad.
ResultadosSe presentan 9 pacientes (2 varones y 7 mujeres) de 42,8 años de edad media. Cinco de los pacientes consultaron con un síndrome menieriforme, 2 casos como vértigo recurrente de características periféricas, otro como hipoacusia súbita y el último caso como hipoacusia neurosensorial de inicio en la infancia. La manifestación audiovestibular más frecuentemente descrita en la literatura en pacientes es la inestabilidad (49%), seguida de vértigo (18%), nistagmo (15%) e hipoacusia (15%). Dentro del nistagmo, el más frecuente es el nistagmo horizontal (74%) seguido del vertical hacia abajo (18%). Otras manifestaciones audiovestibulares son acúfenos (11%), plenitud ótica (10%) e hiperacusia (1%). La cefalea occipitonucal que aumenta con las maniobras de Valsalva y las parestesias en las manos son muy sugestivos de esta enfermedad.
ConclusionesLa aparición de síntomas audiovestibulares en la MCH-I hace que sea relativamente frecuente su derivación al otoneurólogo. Estos pacientes presentan inestabilidad, síndrome vertiginoso e hipoacusia neurosensorial. No es rara la presencia de nistagmo, sobre todo horizonal y vertical hacia abajo. Es importante la familiarización de los otoneurólogos con la sintomatología de esta enfermedad de cara a su diagnóstico diferencial.