Several authors have found increased anxiety in patients the day before an intervention and its correlation with anxiety levels the postoperative period.
In this study, we determined a number of problems to which patients who underwent total laryngectomy often objected: the tracheostomy, being left without a voice and it being an aggressive, major surgery.
Our objective was to assess the degree of anxiety and fears of the patient prior to total laryngectomy.
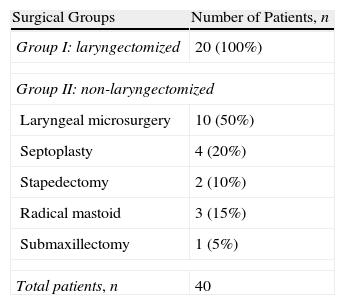
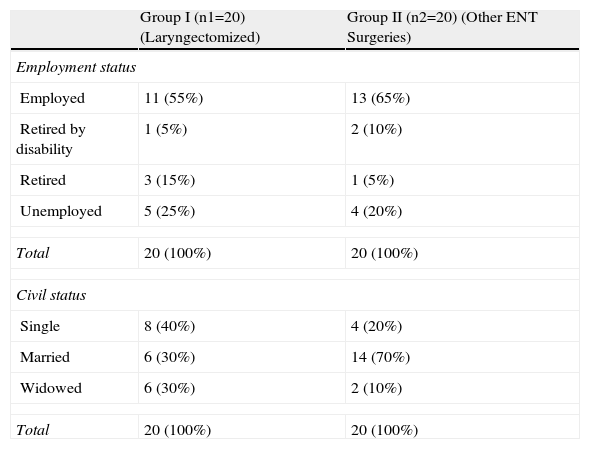
Material and methodsWe compared 2 groups of 20 patients who underwent operation for total laryngectomy and for other ENT pathologies.
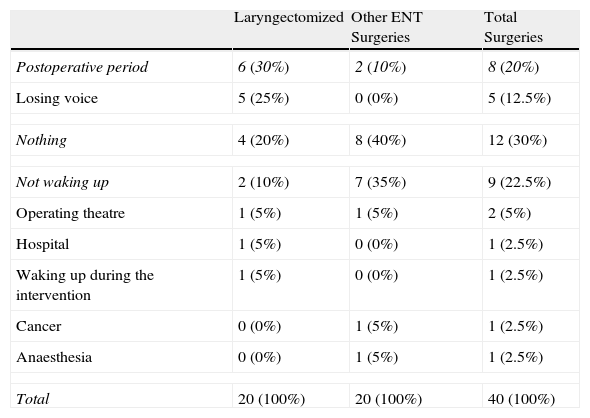
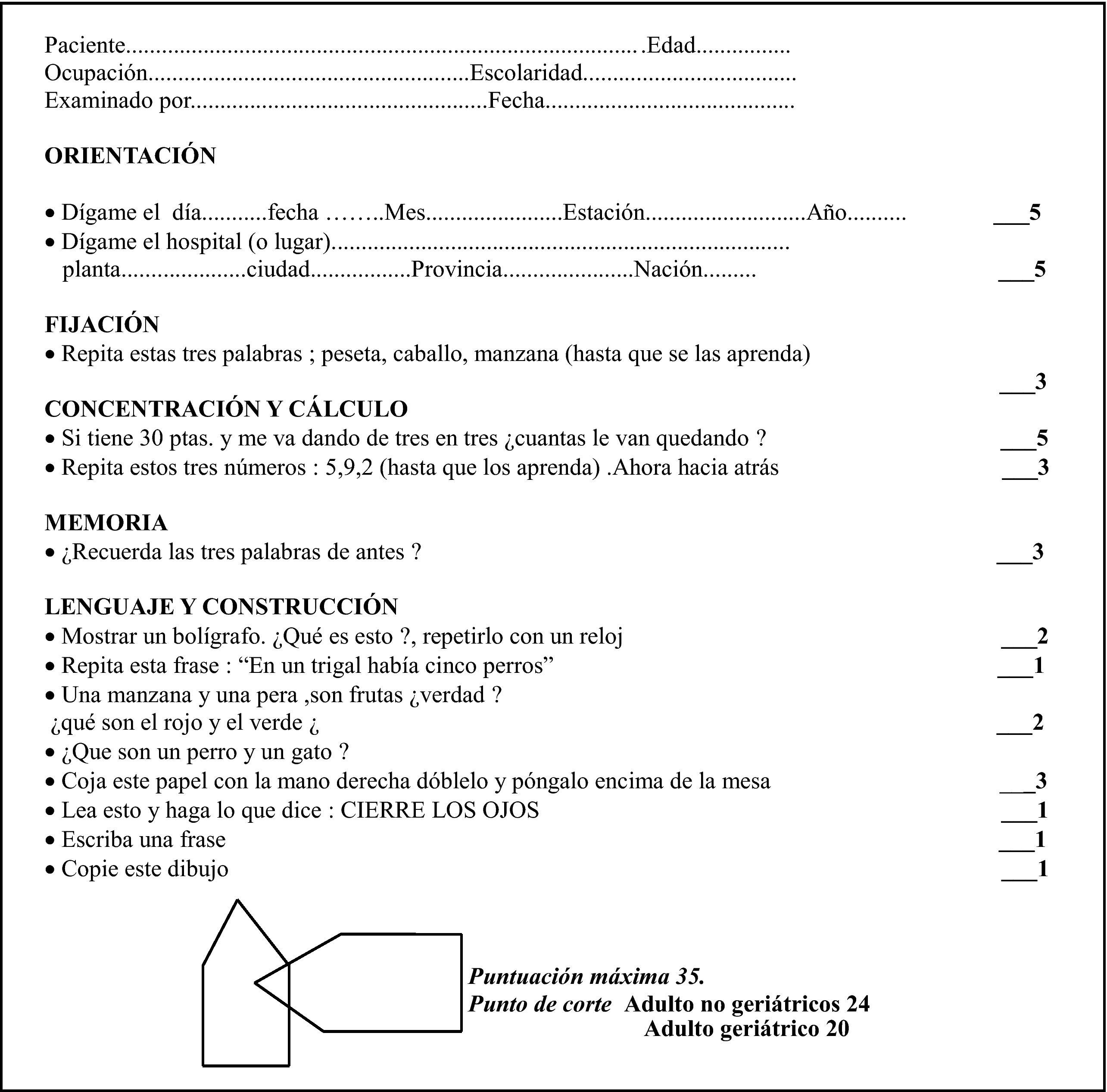
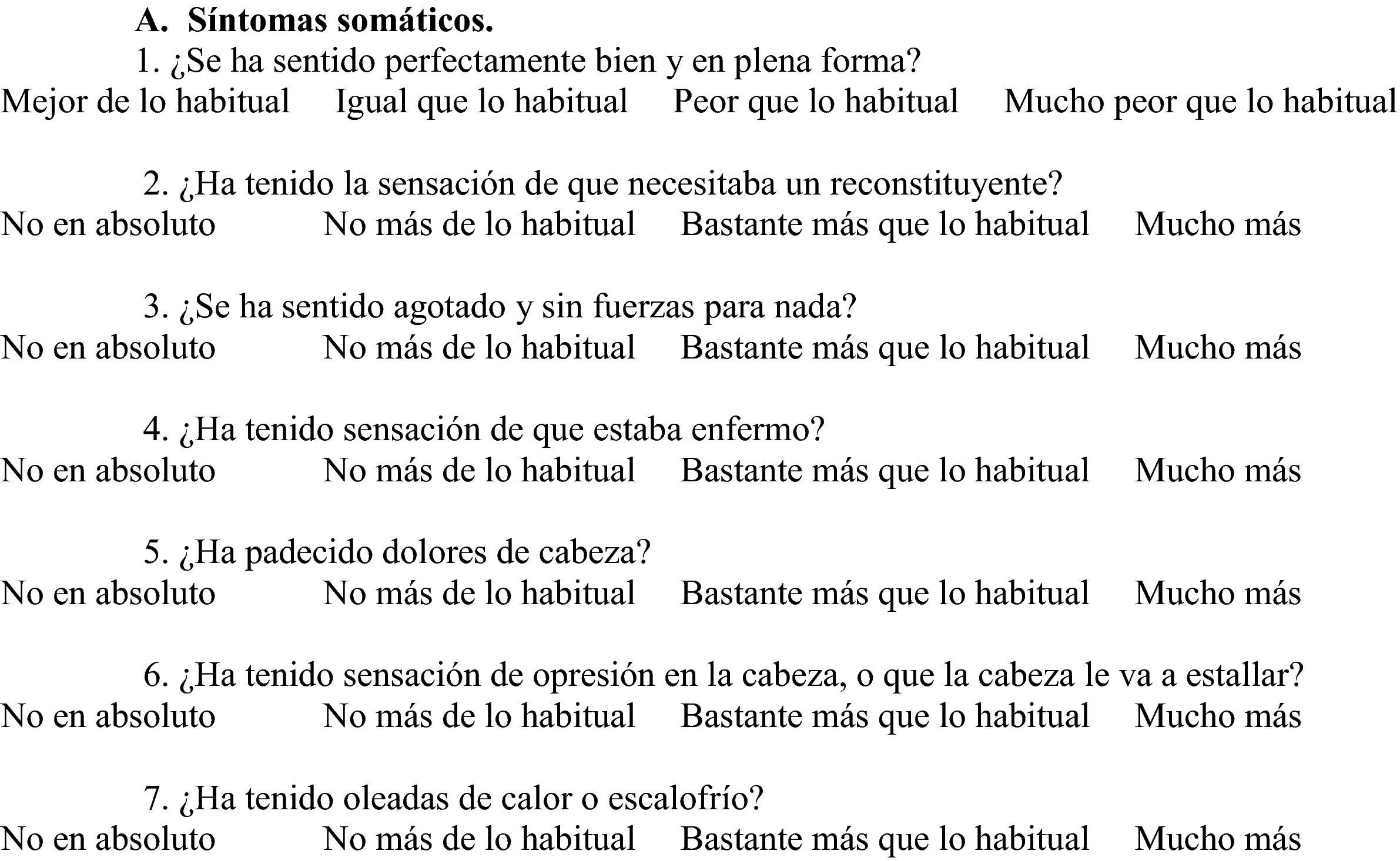
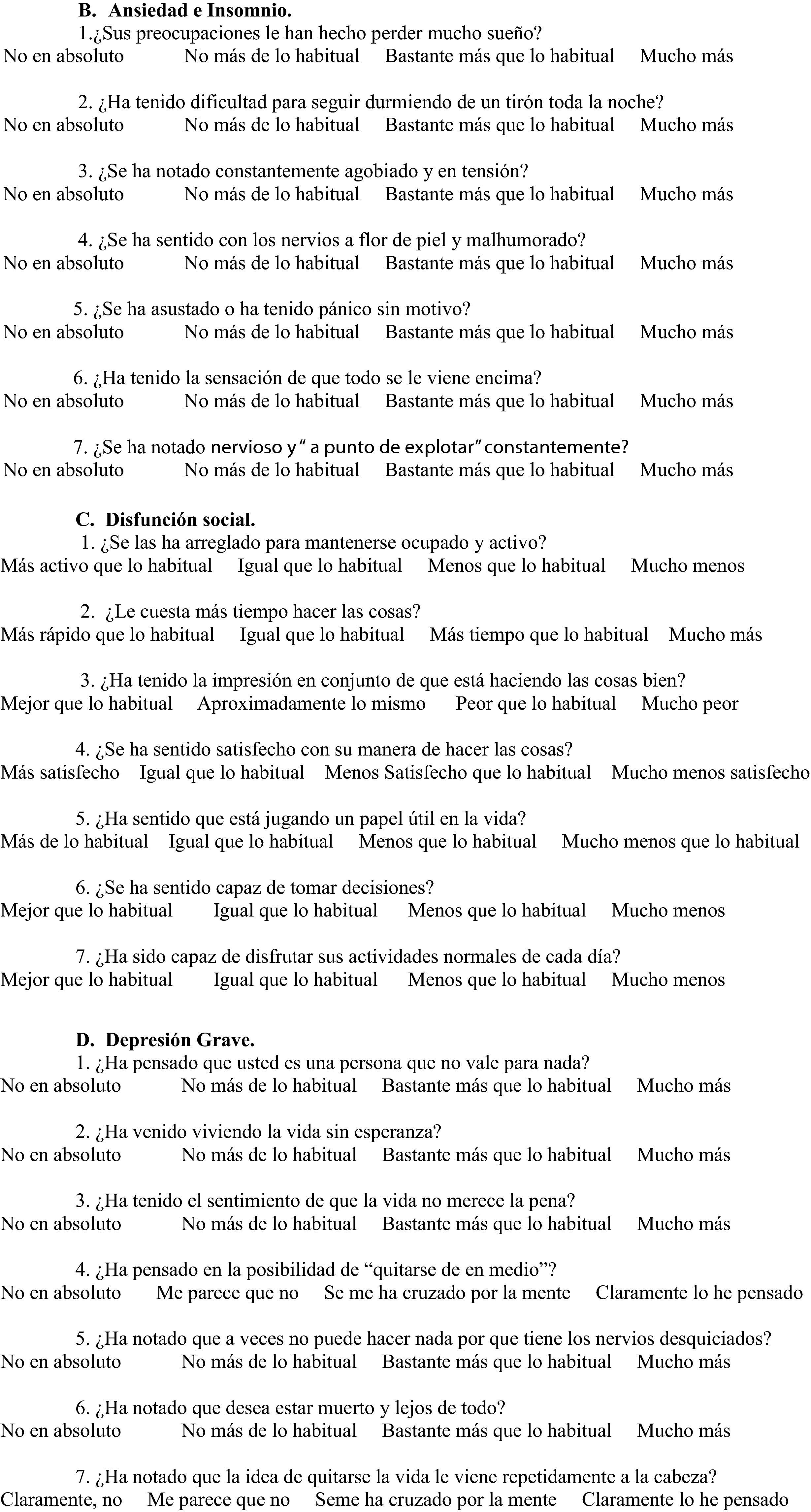
On the day before the operation, we collected demographic and medical data and administered the Spanish versions of the Folstein Mini-Mental State Examination (MMSE) and the Goldberg General Health Questionnaire (GHQ-28). We also investigated whether the patients had any fear or fear of surgery and what that fear was.
ResultsCompletion of the MMSE revealed cognitive impairment in only 1 patient. We subsequently conducted the GHQ-28 and found psychological distress in 20%–25% of our cases. When the different fears in both groups were compared by χ2, the results were not statistically significant.
ConclusionsTotal laryngectomy causes the loss of oral communication and impairs self-image, contributing to a strong emotional reaction. It is essential to have effective rehabilitation, which considers all aspects of health-sickness, such as the recovery of spoken language, social aspects, and the psychological characteristics, vital for proper comprehensive patient management.
Diferentes autores han puesto en evidencia el aumento de ansiedad en los pacientes el día anterior a una intervención y su correlación con los niveles de ansiedad en el post-operatorio.
En este trabajo estudiamos una serie de problemas que a menudo se obvian en el paciente intervenido de laringectomía total: la traqueotomía, el quedarse sin voz y el ser una agresiva e importante intervención quirúrgica.
Nuestro objetivo es valorar el grado de ansiedad y los miedos del paciente previo a la laringectomía total.
Material y métodosSe comparan 2 grupos de 20 pacientes que fueron intervenidos de laringectomía total y de otras enfermedades de ORL.
El día anterior a la operación, recogíamos sus datos sociodemográficos y médico-quirúrgicos, y se les aplicaba el Mini-Examen Cognoscitivo (MEC) de Folstein y el Cuestionario de Salud General de Goldberg (GQH-28) en sus versiones españolas. Exploramos si tenían algún temor o miedo ante la intervención y en qué consistía ese miedo.
ResultadosTras la realización del MEC, sólo un paciente presentó deterioro cognitivo. Posteriormente realizábamos el GHQ-28 y nos encontramos con un malestar psicológico entre el 20 y el 25% de los casos. Al comparar mediante el X2 los diferentes miedos en los 2 grupos los resultados no son estadísticamente significativos.
ConclusionesLa laringectomía total provoca la pérdida de la comunicación oral y la distorsión de la autoimagen, lo que contribuye a una fuerte alteración emocional. Es necesaria una rehabilitación efectiva, que considere todos los aspectos relacionados con el proceso salud-enfermedad desde antes de la cirugía como la recuperación del lenguaje hablado, los aspectos sociales y sus características psicológicas, las cuales son vitales para el adecuado manejo integral del paciente.