Participants with Joint Hypermobility Syndrome (JHS) often suffer from anxiety, stress related illnesses and also from dysautonomia. The autonomic nervous system (ANS) is hypothesized to play a key role in the relationship between these variables. However, to date, no studies have assessed body awareness and the reactivity of autonomically-regulated organs in JHS using the Body Perception Questionnaire.
MethodA cross sectional study including 117 nonclinical youngsters (mean age 16.96±0.87 years old) assessed JHS in relation to body perception. JHS screening was done using the self-reported Screening Questionnaire for Collagen condition and Hypermobility assessment (SQCH) and body perception was assessed using the Spanish version of the Body Perception Questionnaire (BPQ).
ResultsThe JHS was found in 33.3% of the sample and it was significantly higher in females (χ2=12.15; p=<.001). Participants with JHS had higher scores in body awareness (p=.012), stress response (p=.007), ANS reactivity (p=.01), and in the health history inventory (p=<.001). In this last subscale, higher frequency of anxiety (p=<.001), unhappiness (p=<.001), depression (p=<.001), bulimia (p=.012), anorexia (p=.023), eczema (p=.003), and severe menstrual cramps (in females only) (p=.016) were found among the JHS participants. Moreover, JHS participants made significantly more visits to mental health professionals (p=.019) than their non JHS counterparts.
ConclusionsParticipants with JHS have a body perception profile characterized by higher body awareness and stress response and greater ANS reactivity. These participants also have higher frequency of anxiety, depression, bulimia, anorexia, unhappiness, severe menstrual cramps (in females only) and eczema. These findings support the hypothesis that the ANS and body perception may play a key role in the development of anxiety and somatic illnesses among participants with JHS, but this needs to be further evaluated in subsequent studies.
Las personas con síndrome de hipermovilidad articular (SHA) padecen a menudo ansiedad, estrés relacionado con la enfermedad y también disautonomía. Se ha conjeturado que el sistema nervioso autónomo juega un papel clave en la relación entre estas variables, pero hasta la fecha ningún estudio ha evaluado la conciencia corporal y la reactividad de los órganos regulados autonómicamente en el SHA utilizando el cuestionario de imagen corporal.
MétodoEstudio transversal que incluyó a 117 jóvenes no clínicos (edad media 16,96±0,87años) en quienes se valoró el SHA en relación con la imagen corporal. Se realizó un cribado de SHA utilizando el cuestionario autoinformado de cribado para la valoración del estado de colágeno e hipermovilidad (SQCH), evaluándose la percepción corporal mediante la versión española del cuestionario de imagen corporal (BPQ).
ResultadosSe encontró SHA en el 33,3% de la muestra, siendo significativamente superior en las mujeres (χ2=12,15; p≤0,001). Las personas con SHA reflejaron mayores puntuaciones en cuanto a conciencia del cuerpo (p=0,012), respuesta al estrés (p=0,007), reactividad del sistema nervioso autónomo (p=0,01) e inventario de antecedentes de salud (p≤0,001). En esta última subescala se encontró una mayor frecuencia de ansiedad (p≤0,001), infelicidad (p≤0,001), depresión (p≤0,001), bulimia (p=0,012), anorexia (p=0,023), eccema (p=0,003) y dolores menstruales severos (solo en mujeres) (p=0,016) entre las personas con SHA. Además, las personas con SHA realizaron un número de visitas considerablemente superior a los profesionales sanitarios (p=0,019) que los participantes sin SHA.
ConclusionesLas personas con SHA tienen un perfil de percepción corporal caracterizado por una mayor conciencia sobre el cuerpo y una reactividad superior del sistema nervioso autónomo. Estos participantes también poseen una mayor frecuencia de ansiedad, depresión, bulimia, anorexia, infelicidad, dolores menstruales severos y eccema. Estos hallazgos respaldan la hipótesis de que el sistema nervioso autónomo y la imagen corporal pueden jugar un papel principal en el desarrollo de la ansiedad y las enfermedades somáticas entre las personas con SHA, aunque esto debe evaluarse en mayor profundidad en estudios futuros.
The term Joint Hypermobility Syndrome (JHS) is characterized by increased distensibility of the joints in passive movements as well as a hypermobility in active movements along with several extra articular symptoms. The literature shows that JHS is closely associated with anxiety disorders and this correlation constitutes a specific phenotype for a homogeneous type of anxiety in adults and in the elderly (Bulbena-Cabré et al., 2016, 2017; Bulbena, Pailhez, Bulbena-Cabre, Mallorqui-Bague, & Baeza-Velasco, 2015). Specifically, JHS has been associated with higher frequency and intensity of fears and greater severity of anxiety, higher somatic complaints and higher frequency of the so-called endogenous anxiety disorders (panic, agoraphobia and social phobia) (Bulbena, Gago, Sperry, & Berge, 2006; Bulbena-Cabré et al., 2016). Moreover, participants with JHS frequently present with stress-sensitive illnesses such as fibromyalgia, irritable bowel disease, temporomandibular joint disorder and chronic fatigue syndrome (Grahame, 2008).
While the association between anxiety disorders and JHS is well established, the underlying mechanisms are still unclear. Some biological hypotheses have been proposed to explain this association including genetic risks, interceptive sensitivity, somatosensory amplification, emotion processing variances, and autonomic nervous system dysfunction. In the area of genetics, one study found a cytogenetic anomaly (DUP-25) common to these two phenomena (Gratacòs et al., 2001), although to date this study has not been replicated (Henrichsen et al., 2004; Tabiner et al., 2003). The perception and interpretation of physiological excitation plays a role in anxiety disorders (Craig, 2003; Damasio, Everitt, & Bishop, 1996) and JHS participants have more intense interoception (Mallorqui-Bague et al., 2014) and somatosensory amplification (Baeza-Velasco, Gely-Nargeot, Bulbena-Vilarrasa, & Bravo, 2011). Neuroimaging studies (Eccles et al., 2012; Mallorqui-Bague et al., 2014) have shown significant emotion processing differences in JHS, which could in part explain the vulnerability for anxiety and other somatic symptoms.
Another important biological hypothesis is the autonomic nervous system dysfunction. Dysautonomia have symptoms that overlap with anxiety and JHS. Critchley, Eccles, and Garfinkel (2013) extensively studied visceral inputs because of their influence on thoughts, feelings and behavior. Consistent Chritchley's views, the Polyvagal Theory (Porges, 1995, 2011) introduced a new perspective relating autonomic function to behavior that included an appreciation of autonomic nervous system as a “system,” the identification of neural circuits involved in the regulation of autonomic state that also influence responses to environmental stimuli and an interpretation of autonomic reactivity as adaptive within the context of the phylogeny of the vertebrate autonomic nervous system. Following this line of research, Porges developed the Body Perception Questionnaire (BPQ), an instrument to assess subjective experiences of body awareness and autonomic reactivity (Porges, 1993). Compared to other scales that measure subjective experiences of body perception, the BPQ was developed with a foundation in the peripheral neural pathways that transmit bodily sensations to the brain, which provides valuable information about the reactivity of autonomically-regulated organs. The BPQ has been used in several peer review studies to obtain objective reports of bodily reactions and states (Critchley, Wiens, Rothstein, & Dolan, 2004; Mehling et al., 2009) but to date this instrument has not been used in JHS research.
MethodIn this study, we evaluated a sample of nonclinical youngsters to assess JHS in relation to the level of awareness of body processes, the subjective experience of autonomic nervous system reactivity, and the frequency of autonomic related illnesses. This cross-sectional study was conducted in a high school in Barcelona (Spain) and a total of 117 participants (33 males (28.2%) and 84 females (71.7%) with ages ranging from 16 to 18y/o were included in the study. All incoming students were eligible to participate and no exclusion criteria were applied. Participation was voluntary without any economic compensation and informed consent was obtained from participants after the study procedures were fully explained.
Socio-demographic data was obtained through a socio-demographic questionnaire (including visits to Psychiatrist/Psychologist). The mean age was 16.96 (SD±0.87) years old and 41 (35%) participants were from 11th grade and 76 (65%) from 12th grade and all of them were Caucasians. In terms of visits to a mental health professional, 32 participants (27.35%) admitted to seeking mental health help and 85 (72.65%) denied it.
The JHS was screened with the self-reported Screening Questionnaire for Collagen condition and Hypermobility assessment (SQCH). It is a 7 item questionnaire that includes the basis of the 5 item self-reporting questionnaire of Hakim and Grahame (2003) and 2 extra-articular features (easy bruising and hypertrophic scarring). This questionnaire has adequate clinimetric properties and has been validated for clinical use (Bulbena et al., 2014). The questionnaire is scored by adding the points of each item (ranging from 0 to 7), with cut-off scores to diagnose JHS set at ≥3/7.
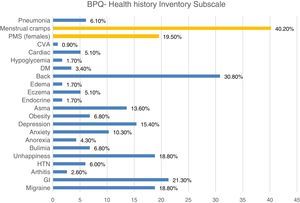
Body perception was evaluated using the Spanish version of the Body Perception Questionnaire (BPQ). It has a total of 5 dimensions including body awareness (45 items), stress response (10 items), autonomic nervous system (ANS) reactivity (27 items), stress style (12 items, subgroup 1 and 2) and health history inventory (27 items). All ratings except for the Health History Inventory dimension are made on a five-point ordinal scale spanning never (0), occasionally (1), sometimes (2), usually (3), and always (4). The health history inventory also used a five-point ordinal scale but slightly different spanning never (0), mild (1), moderate (2), severe (3) and debilitating (4). Total final score of each dimension is showed as the mean score of each category. The health history inventory included some autonomic-related illnesses including migraine headaches, gastric distress or digestive problems, arthritis, hypertension, hopelessness, unhappiness, clinical depression, bulimia, anorexia, obesity, asthma, endocrine problems (e.g., thyroid, adrenal, or gonadal hormone dysfunction), eczema, edema, back problems, diabetes, epilepsy, cancer, hypoglycemia, heart disease, stroke, gastric & duodenal ulcers, psychiatric disorders, pneumonia, heart attack, and motion sickness. Premenstrual syndrome, severe menstrual cramps and post-partum depression are also items of the health history inventory applied only to females.
Statistical analysis: Descriptive statistics were used to report frequencies, means and standard deviations (SD). The Student tests and ANOVA were used for continuous data and χ2 tests for qualitative data. Statistical significance was determined by two-tailed p<.05. All statistical analyses were conducted with SPSS – IBM version 22 for Macintosh.
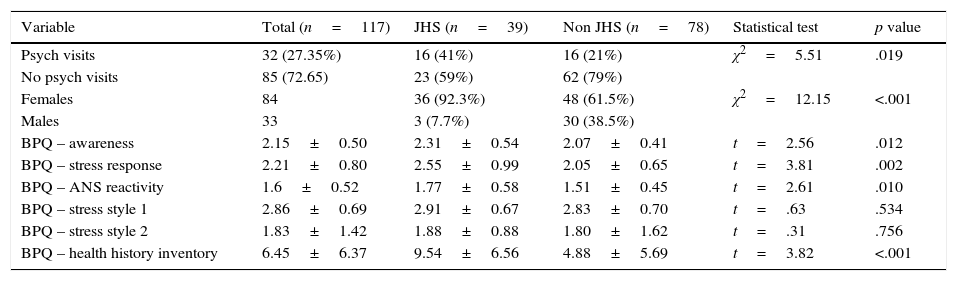
ResultsIn this sample, 33.3% of the participants met criteria for JHS (score ≥3/7 SQCH) with a significantly higher proportion of females in this group (p<.001). Based on JHS scores, participants were classified into the JHS and the non JHS groups and different socio-demographic and BPQ variables were compared between these two groups. The JHS group reported significantly more visits to the psychiatrist (p=.019) and scored significantly higher in the Body awareness (p=.012), stress response (p=.002), ANS reactivity (p=.01), and in the health history inventory (p=<.001) compared to the non-JHS group, see full results in Table 1.
Group differences (JHS vs. non JHS) in socio-demographic and BPQ scores in the sample.
| Variable | Total (n=117) | JHS (n=39) | Non JHS (n=78) | Statistical test | p value |
|---|---|---|---|---|---|
| Psych visits | 32 (27.35%) | 16 (41%) | 16 (21%) | χ2=5.51 | .019 |
| No psych visits | 85 (72.65) | 23 (59%) | 62 (79%) | ||
| Females | 84 | 36 (92.3%) | 48 (61.5%) | χ2=12.15 | <.001 |
| Males | 33 | 3 (7.7%) | 30 (38.5%) | ||
| BPQ – awareness | 2.15±0.50 | 2.31±0.54 | 2.07±0.41 | t=2.56 | .012 |
| BPQ – stress response | 2.21±0.80 | 2.55±0.99 | 2.05±0.65 | t=3.81 | .002 |
| BPQ – ANS reactivity | 1.6±0.52 | 1.77±0.58 | 1.51±0.45 | t=2.61 | .010 |
| BPQ – stress style 1 | 2.86±0.69 | 2.91±0.67 | 2.83±0.70 | t=.63 | .534 |
| BPQ – stress style 2 | 1.83±1.42 | 1.88±0.88 | 1.80±1.62 | t=.31 | .756 |
| BPQ – health history inventory | 6.45±6.37 | 9.54±6.56 | 4.88±5.69 | t=3.82 | <.001 |
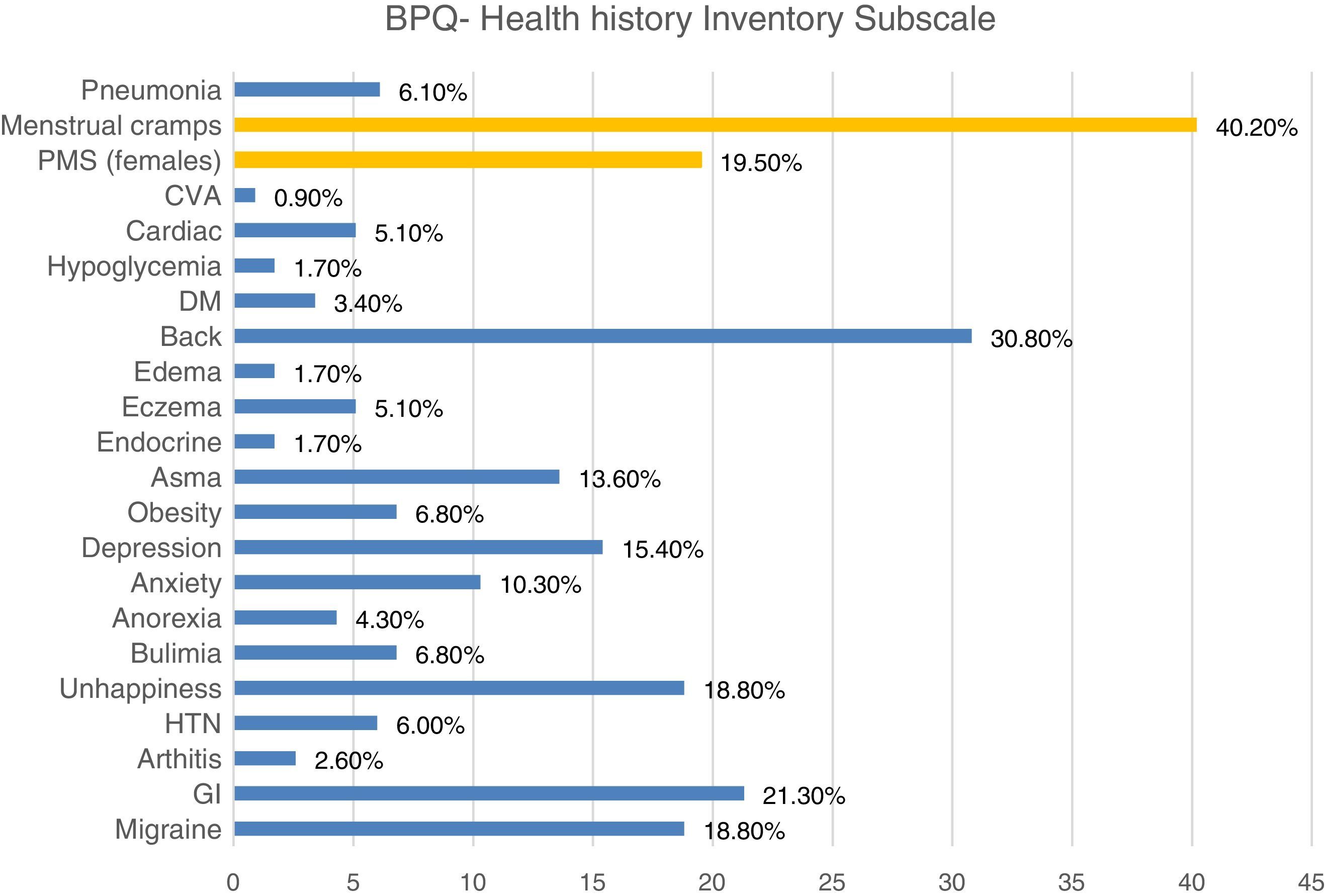
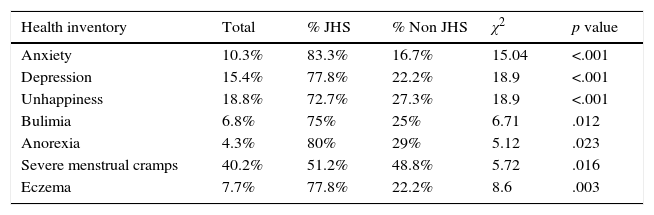
The health history inventory included the autonomic-related illnesses and the frequencies of each category are shown in Fig. 1. The most frequent medical complaints among this nonclinical sample were back problems (30.80%), gastrointestinal problems (21.30%), migraines (18.80%), unhappiness (18.50%), and premenstrual syndrome (19.50%) and menstrual cramps among females (40.20%). The frequencies of each variable were compared between groups and the JHS participants had significantly higher percentages of anxiety (p=<.001), depression (p=<.001), unhappiness (p=<.001), bulimia (p=.012), anorexia (p=.023), severe menstrual cramps (p=.016), and eczema (p=.003), as shown in Table 2. Non-significant results were not included in the table.
Group differences in the Health History Inventory Subscale.
| Health inventory | Total | % JHS | % Non JHS | χ2 | p value |
|---|---|---|---|---|---|
| Anxiety | 10.3% | 83.3% | 16.7% | 15.04 | <.001 |
| Depression | 15.4% | 77.8% | 22.2% | 18.9 | <.001 |
| Unhappiness | 18.8% | 72.7% | 27.3% | 18.9 | <.001 |
| Bulimia | 6.8% | 75% | 25% | 6.71 | .012 |
| Anorexia | 4.3% | 80% | 29% | 5.12 | .023 |
| Severe menstrual cramps | 40.2% | 51.2% | 48.8% | 5.72 | .016 |
| Eczema | 7.7% | 77.8% | 22.2% | 8.6 | .003 |
In this novel study, we evaluated JHS and body perception in a sample of nonclinical youngsters in order to define body perception profiles in JHS.
The literature shows that JHS is usually more prevalent in pediatric and young populations ranging from 3 to 30%. Several factors are known to influence the prevalence old JHS including age, gender and ethnicity (Hakim & Grahame, 2003). Among this sample, the prevalence of JHS was slightly higher (33%) which could be explained by the higher frequency of females. The sample was homogenous in terms of age and race but females, besides being overrepresented, were significantly more hypermobiles. This is in line with other studies that have estimated that JHS is more frequent among females (ratio 3:1) (Bulbena et al., 2017).
Participants with JHS had significantly higher scores in most of the BPQ subscales including body awareness, stress response, reactivity of ANS, and the health history inventory. No significant differences were found in the stress style 1 and 2 subscales. The BPQ was developed to specifically assess subjective experiences of the function and reactivity of target organs and structures that are innervated by the ANS. As mentioned above, it is based on the Polyvagal Theory (Porges, 2007, 2011) which has provided a framework to generate hypotheses regarding the functional organization of the neural pathways that underlie unconsciously-appraised bodily states and their reactivity. The ANS has been proposed as one of the key underlying mechanisms behind the association between JHS and anxiety. Augmented or disordered awareness of such bodily signals is a feature of multiple clinical disorders such as anxiety, panic attacks, and depression (Cameron, 2001; Domschke, Stevenes, Pfleiderer, & Gerlach, 2010; Wiebking et al., 2015). In JHS, Mallorqui-Bague et al. (2014) studied a small sample of healthy volunteers and found that interoceptive sensitivity mediated the relationship between state anxiety and hypermobility.
Following the accumulated evidence on this topic over the past 30 years, our group described the “Neuroconnective phenotype” (Bulbena et al., 2017) in which the solid correlation between JHS and anxiety is in the core and several pathophysiological dimensions are described (somatosensory, psychopathological, somatic illnesses, behavioral patterns, and somatic symptoms domains). Specifically, the somatosensory dimension implies that patients with this phenotype often suffer from dysautonomia and have a greater sensitivity to the inner and external sensory stimuli, and thus, our findings are in agreement with this theory. However, clinical research and treatment often focus on psychological experiences or brain structures (i.e., amygdala), overlooking the dynamic embodied experiences that are part of affective processes and clinical problems. Subsequent studies should consider the bodily and somatic dimensions along with the psychopathological and cognitive areas of this phenotype for earlier prevention and development of more specific treatments.
Participants with JHS reported significantly more visits to mental health professionals and had also significantly higher rates of self-reported anxiety, depression, unhappiness, bulimia, anorexia, severe menstrual cramps, and eczema. Even though we did not assess the prevalence of any psychiatric illness in this sample, the self-reported results on the health history inventory of the participants are congruent with prior research. The anxiety-JHS profile has been proved to be stable across several areas of the psychopathology including depression, substance abuse, eating, and neuro-developmental disorders (Bulbena-Cabré et al., 2016). Therefore, it is not surprising to find people with JHS seeking more mental health help compared to people without JHS. In terms of eating disorders, participants with JHS have higher frequency of eating disorders and Baeza-Velasco (Baeza-Velasco, Van den Bossche, Grossin, & Hamonet, 2016; Bulbena et al., 2017) proposed a model of eating disorders in JHS hypothesizing that both articular (i.e. temporomandibular joint dysfunction) and extra-articular features (i.e. gastrointestinal sensitivities, food allergies) play a role in developing and maintaining these eating patterns. The high incidence of food sensitivities among people with JHS is suggestive of histamine hyper-reactivity and several allergic related problems have been described in JHS such as eczema (Hauser & Phillips, 2011). Gynecological aspects of JHS have been largely ignored in the past, but it is now accepted that women with JHS/EDS-HT commonly suffer from irregular menses, meno/metrorrhagias, and severe dysmenorrhea, also known as severe muscle cramps. Together, these findings strengthen the hypothesis that the JHS phenotype constitutes a multisystemic condition and thus a multidimensional approach should be granted in this type of patients.
This study has limitations. First, the study was conducted in a small, homogenous sample in terms of race, years of education and age and, thus, the results cannot be extrapolated to the entire population. Another limitation is that medical and psychiatric manifestations were based on self-report and no objective measures were applied to ensure proper validity of the diagnosis.
ConclusionsParticipants with JHS have an atypical body perception profile characterized by higher awareness, stress response, and ANS reactivity. They also report higher frequency of autonomic related illnesses including anxiety, depression, bulimia, anorexia, unhappiness, severe menstrual cramps (in females only) and eczema and are more likely to seek mental health help compared to controls. These findings support the hypothesis that the ANS and body perception may play a key role in the development of anxiety and somatic illnesses among participants with JHS. The documentation of shared common abnormalities in both the ANS and the collagen structure may represent a diathesis not yet identified, but worthy to investigate by subsequent studies.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestNone of the authors have any conflicts of interest.