We compared the Geriatric Trauma Outcome Score (GTOS) with the probability of survival using the TRISS methodology (PS-TRISS) in geriatric severe trauma patients admitted to Intensive Care Units (ICU) participating in the Spanish trauma ICU registry (RETRAUCI).
MethodsRetrospective analysis from the RETRAUCI. Quantitative data were reported as median (Interquartile Range (IQR)), and categorical data as number (percentage). We analyzed the validity of the GTOS and PS-TRISS to predict survival. Discrimination was analyzed using receiver operating characteristics curves. Calibration was analyzed using the Hosmer–Lemeshow goodness-of-fit test. A P value <.05 was considered statistically significant.
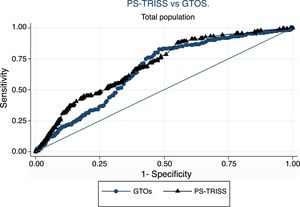
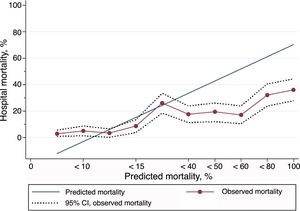
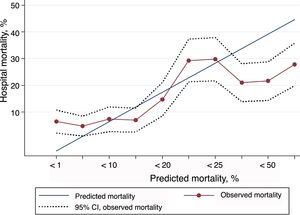
ResultsThe cohort included 1417 patients aged ≥65 years. Median age was 75.5 (70.5–80.5), 1003 patients were male (68.2%) and median Injury Severity Score was 18 (13–25). Mechanical ventilation was required in 61%. Falls were the mechanism of injury in 659 patients (44.8%). In-hospital mortality rate was 18.2%. The areas under the curve were: PS-TRISS 0.69 (95% CI 0.66–0.73), and GTOS 0.66 (95% CI 0.62–0.70); P<.05. Both scores overestimated mortality in the upper range of predicted mortality.
ConclusionsIn our sample of geriatric severe trauma patients, the accuracy of GTOS was lower than the accuracy of the PS-TRISS to predict in-hospital survival. The calibration of both scores for the geriatric population was deficient.
Comparamos el Geriatric Trauma Outcome score (GTOS) con la probabilidad de supervivencia empleando la metodología TRISS (PS-TRISS) en pacientes traumáticos ancianos ingresados en las Unidades de Cuidados Intensivos (UCI) participantes en el registro de traumatismo en UCI (RETRAUCI).
MétodosAnálisis retrospectivo del RETRAUCI. Los datos cuantitativos se expresan como mediana (rango intercuartil), los datos categóricos como número (porcentaje). Analizamos la validez del GTOS y la PS-TRISS para la predicción de supervivencia. La discriminación se evaluó mediante curvas receiver operating characteristics. La calibración de los modelos se analizó mediante el test de bondad de ajuste de Hosmer-Lemeshow. Un valor de p < 0,05 se consideró estadísticamente significativo.
ResultadosLa cohorte incluyó a 1.417 pacientes ≥65 años. Mediana edad 75,5 (70,5–80,5) años, varones 1.003 (68,2%), mediana Injury Severity Score 18 (13–25). Ventilación mecánica, 61%. Las caídas fueron el mecanismo de lesión en 659 pacientes (44,8%). Mortalidad hospitalaria: 18,2%. El área bajo la curva para PS-TRISS fue 0,69 (IC del 95% 0,66–0,73) y para GTOS 0,66 (IC del 95% 0,62–0,70); p<0,05. Ambos scores sobrestimaron la mortalidad en el rango alto de mortalidad predicha.
ConclusionesEn nuestra muestra de pacientes traumáticos ancianos la precisión de GTOS fue inferior a la de la metodología TRISS en la predicción de la supervivencia hospitalaria. Ambos scores tuvieron una mala calibración en la población anciana.
The progressive aging of the populations of developed countries has led to a significant increase in the number of elderly patients who are treated after severe trauma. This number is expected to continue increasing in the coming decades.1,2 According to results from the pilot phase of the ICU trauma registry (RETRAUCI), more than 20% of trauma patients admitted to the Intensive Care Units (ICU) in Spain are over 65 years of age.3 These patients present different baseline characteristics. These are patients with a lower physiological reserve against trauma aggression, in whom the predominant mechanisms of injury is accidental low-energy falls, complicated by the habitual use of antiplatelet agents and anticoagulants.4 The prediction of the final outcome of these patients is extremely important, since mortality increases progressively with age.4 Knowing the probability of survival at admission to the ICU can help make complex decisions in this population, including the limitation of life support (LLS). This calculation has usually been determined with the complex Trauma and Injury Severity Score (TRISS) method, but in recent years a new useful score has been developed in the elderly population, the Geriatric Trauma Outcome Score (GTOS), which is simpler and easier to use 24h after admission.
The aim of our study was to compare the probability of survival using the TRISS methodology (PS-TRISS) with the GTOS in elderly traumatic patients admitted to the Spanish ICU participating in the RETRAUCI.
MethodsThe RETRAUCI included its first patient on November 23, 2012, and was approved by the ethics committees of the participating hospitals. It is a multi-center registry with voluntary participation and implementation in 49 centers throughout the country promoted by the Neurointensive and Trauma Workgroup of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC).
Inclusion and exclusion criteria: there is controversy regarding what age should be used as a cut-off point to define senior patients. A recent consensus document has reported the age of 65 as the most commonly used among its participants,5 and this has been the cut-off point used in our study. Thus, we retrospectively analyzed patients aged 65 or older included between November 2012 and May 2017, with complete data, who had been admitted with trauma injuries to a participating adult ICU. These senior patients were followed until hospital discharge to analyze the outcome of hospital admission, coded as a dichotomous variable (alive or dead).
Excluded from the study were patients with:
- -
Missing data to calculate the TRISS or GTOS
- -
Unknown results at discharge
Scores: the probability of survival using the TRISS methodology was calculated from Revised Trauma Score data (respiratory rate, systolic blood pressure and Glasgow Coma scale score), obtained in the initial patient analysis before starting resuscitation. The data used to calculate the Injury Severity Score (ISS), and with it the PS-TRISS, were documented by each researcher according to the updated version of the Abbreviated Injury Scale (AIS) from 2008.6 The data used to calculate the GTOS were collected after admission to the ICU by the main researcher at each hospital, following the formula described in the original study.7 Its calculation involved an increasing score with age, adding 2.5×ISS, and finally 22 points are assigned in case of having received blood products within the first 24h. The final score corresponded with a survival probability assigned in a simple normogram.7
Statistical AnalysisQuantitative data were documented as median (25th–75th interquartile ranges) and the categorical data as number (percentage). The comparison among the groups with categorical variables was conducted with the Chi-squared test.
To analyze the validity of both models, we studied the discrimination and calibration in the sample of senior patients. We analyzed the discrimination of the model using receiver operating characteristic (ROC) curves and analyzed the area under the curve (AUC) and its 95% confidence interval (95% CI). Using the Youden index, the cut-off point that maximized sensitivity and specificity was determined, calculating the positive predictive value, the negative predictive value and the precision for said cut-off point. Furthermore, the calibration of a prognostic model evaluated the agreement between the probability observed and predicted by the model in different mortality ranges. The Hosmer–Lemeshow (HL) goodness-of-fit test was applied. The sample was divided into 10 groups with a similar number of observations for predicted mortality. For each group, the observed and predicted mortality were obtained. For the predicted mortality, the weighted average was used for each group.8 In a complementary manner, the standardized mortality ratio (SMR) was used to assess the calibration, calculated by means of the quotient between the observed and predicted mortality. A value of one represented perfect calibration. Values lower than one were interpreted as an overestimation of mortality (observed mortality lower than predicted mortality) and values greater than one identified models that underestimate mortality (observed mortality greater than predicted mortality). To calculate the confidence intervals of the standardized mortality ratio, the Byar approximation method was used.
A value of P<.05 was considered statistically significant. The statistical analysis was performed with STATA 12 (StataCorp 2011, College Station, TX; StataCorp LP). OpenEPI 3 (OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version, http://www.OpenEpi.com) was used to calculate the confidence intervals of the standardized mortality ratio.
ResultsThe cohort consisted of 5882 patients, 1417 of whom (24.1%) were aged ≥65 years and constituted the study population. The median age was 75.5 (70.5–80.5) years and there were 1003 males (68.2%). The median ISS was 18 (13–25). Accidental falls were the main mechanism of injury in up to 659 patients (44.8%). 71% (1004 patients) presented traumatic brain injury (TBI), and 61% required mechanical ventilation. Within the first 24h, 435 patients (30.7%) underwent urgent surgical procedures, the most frequent being neurosurgical. During hospital admission, 181 patients (12.8%) required other non-urgent surgical procedures. Hospital mortality reached 18.2%.
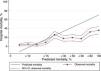
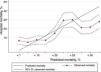
Excluded from the study were 193 patients with incomplete data for the calculation of PS-TRISS and GTOS or with unknown discharge outcome. Thus, 1224 patients (86.4%) were finally analyzed. The AUC for the calculation of the probability of survival was: PS-TRISS 0.69 (95% CI 0.66–0.73, sensitivity 88.1%, specificity 45.8%, positive predictive value 24.5%, negative predictive value 94.9%, accuracy 52.8%, Youden index 0.33); GTOS 0.66 (95% CI 0.62–0.70, sensitivity 83.4%, specificity 51.7%, positive predictive value 26.1%, negative predictive value 93.8%, precision 57.1%, Youden index 0.35); P<.05 (Fig. 1). The results of the HL goodness-of-fit test for the PS-TRISS (χ2 value 245.07, P value <.005) and the GTOS (χ2 value 58.86, P value <.005) are shown in Tables 1 and 2. The correlation between mortality observed and predicted by PS-TRISS and GTOS is shown in Figs. 2 and 3. Both scores overestimated mortality in the upper range of predicted mortality. The standardized mortality ratios were 0.58 (95% CI 0.51–0.67) and 0.85 (95% CI 0.74–0.97) for PS-TRISS and GTOS, respectively.
Hosmer–Lemeshow Goodness-of-Fit Analysis of the PS-TRISS.
| Decile predictive of mortality (%) | Number of patients | Survivors observed | Survivors expected | Deaths observed | Deaths expected | |
|---|---|---|---|---|---|---|
| 1 | 1.6–3.2 | 143 | 139 | 138.567 | 4 | 4.433 |
| 2 | 3.4–5.7 | 138 | 131 | 131.514 | 7 | 6.486 |
| 3 | 5.7–6.7 | 121 | 117 | 113.861 | 4 | 7.139 |
| 4 | 7.1–10.6 | 127 | 116 | 116.332 | 11 | 10.668 |
| 5 | 10.7–13.1 | 131 | 97 | 116.197 | 34 | 14.803 |
| 6 | 13.2–21.4 | 142 | 117 | 115.73 | 25 | 26.27 |
| 7 | 21.5–36.7 | 143 | 115 | 96.382 | 28 | 46.618 |
| 8 | 36.8–55.3 | 122 | 101 | 62.464 | 21 | 59.536 |
| 9 | 55.4–76.9 | 121 | 82 | 40.051 | 39 | 80.949 |
| 10 | 77–100 | 130 | 83 | 12.87 | 47 | 117.13 |
| 1318 | 1098 | 943.968 | 220 | 374.032 |
Hosmer–Lemeshow Goodness of Fit Test for the Geriatric Trauma Outcome Score.
| Decile predictive of mortality (%) | Number of patients | Survivors observed | Survivors expected | Deaths observed | Deaths expected | |
|---|---|---|---|---|---|---|
| 1 | 1.3–4.2 | 124 | 116 | 119.784 | 8 | 4.216 |
| 2 | 4.3–5.9 | 126 | 120 | 119.7 | 6 | 6.3 |
| 3 | 6–8.2 | 123 | 114 | 114.39 | 9 | 8.61 |
| 4 | 8.3–10.5 | 128 | 119 | 115.84 | 9 | 12.16 |
| 5 | 10.7–14.1 | 122 | 104 | 106.628 | 18 | 15.372 |
| 6 | 14.3–17.7 | 126 | 89 | 105.966 | 37 | 20.034 |
| 7 | 18–22.4 | 124 | 87 | 98.828 | 37 | 25.172 |
| 8 | 22.8–30.3 | 128 | 101 | 95.616 | 27 | 32.384 |
| 9 | 30.8–46.8 | 125 | 98 | 79.125 | 27 | 45.875 |
| 10 | 47.3–99 | 122 | 88 | 43.066 | 34 | 78.934 |
| 1248 | 1036 | 998.943 | 212 | 249.057 |
In severe trauma disease, scores can be used to evaluate the quality of the care provided and to help establish patient prognosis as well as the decision-making process. This fact is especially relevant in patients over 65, where the comorbidity and the use of different treatments may further compromise their lower physiological reserve.1,2 The complex TRISS method integrates physiological/radiological information and has been used in severe traumatic disease as a standard methodology to evaluate the care provided to this population.6 However, it requires time and adjustment by coefficients that are not updated or adapted to the different geographical areas in which it is used.6 In addition, it was not designed and validated specifically for the elderly population, but for young patients with high-energy trauma. In this context, the GTOS7 has recently been published, which assesses age, ISS score and the need for blood products within the first 24h. Thus, a prediction of the chances of survival of elderly traumatic patients can be easily obtained with a precision similar or even superior to the TRISS.7,9,10 Therefore, we decided to analyze this new and simple score in the population of elderly trauma patients in the RETRAUCI.
The results of our study do not support the use of GTOS in place of the TRISS methodology because it was less accurate. The fundamental difference between our sample and previous studies lies in the greater severity of the patients, which probably justifies the differences found. In the original sample for the definition of GTOS, the mean age was 76.5±8.1 years, mean ISS was 12.4±9.8, and mortality was 10.8%.7 In the multicenter external validation of this score, the mean age was 77±8.1 years, mean ISS was 12.3±10.6 and mortality was 11%.9 In our series, mean age was 75.6±6.5 years, average ISS was 20.6±11, and mortality 18.2%.
Another factor that could vary among the populations studied is the presence of TBI. It is well known that this is a determining factor in the final outcome of elderly trauma patients in terms of mortality and severe neurological disability.11,12 Thus, TBI and neurological deterioration are factors associated with decision making for LLS in senior trauma patients in our environment, together with older age and higher score on the severity scales.13 In our sample, 71% of the patients presented TBI, reaching 58% of the sample of patients over 65, who presented a head injury AIS ≥3. In the original sample and in the multicenter external validation, this datum was not documented,7,9 so we cannot corroborate this hypothesis.
Given these data, we do not consider the GTOS an inferior scale compared to the TRISS method; however, it was designed for a different less severely injured population treated in the emergency department and in an initial care system for patients with different severe trauma. In our opinion, our results reflect the need to adapt and update the predictive scales to the study population,6,14 as deduced from the poor calibration shown by both scales in our elderly population. This is a common phenomenon in the context of the ICU.15
Our study has some limitations that should be reviewed: the first is the limited number of patients included for an analysis of these characteristics, despite being a multicenter registry. The second limitation is the voluntary nature of the registry, which means that the participating centers could be especially motivated, and this could potentially affect the mortality analysis. However, we believe that RETRAUCI adequately represents the healthcare reality of severe trauma in our country as it includes hospitals of different levels of care. The third limitation has to do with the calibration study. Although the HL test is widely accepted, some limitations have been identified. Mainly, the instability of the results according to the number of groups used, in addition to the arbitrariness in the number of groups chosen.16 Therefore, the analysis was complemented with the standardized mortality ratio. Finally, we should comment that a large number of elderly patients receive LLS, and this may influence the prognostic capacity of a score.17 This aspect has not been analyzed in our study.
In conclusion, in our sample of trauma patients over the age of 65 admitted to the ICU, GTOS was less accurate than the TRISS method to predict hospital survival. Both scores showed poor calibration in our senior population.
FundingThe registry received a grant from the Fundación Mutua Madrileña during the first 3 years from the development of an online data collection tool, given in the name of the main researcher of this project (Dr. Chico-Fernández, Referencia no. AP117892013).
Conflict of InterestsThe authors have no conflict of interests to declare regarding the manuscript.
The authors would like to acknowledge the following persons for their work developing and maintaining the database: Miguel Ángel Ferrero Fernández (Computer Engineer and Head of the Computer Department of the SEMICYUC).
Please cite this article as: Barea-Mendoza JA, Chico-Fernández M, Sánchez-Casado M, Molina-Díaz I, Quintana-Díaz M, Jiménez-Moragas JM, et al. Predicción de la supervivencia en pacientes traumáticos ancianos: comparación entre la metodología TRISS y el Geriatric Trauma Outcome Score. Cir Esp. 2018;96:357–362.