Rapid vaccination is the only way to fight against COVID-19.Vaccine hesitancy is the major barrier against this strategy. The main objective of this cross-sectional study was to analyze COVID-19 vaccine acceptance in the general population of West Bengal (India), as well as to investigate the factors that were independently associated with people's desire to receive the vaccine.
MethodsAn online questionnaire was distributed by email, Whatsapp, and other social media platforms, and the responses were analyzed using the SPSS (Version 20) software.
ResultsWe conducted a web-based survey in West Bengal, India (N = 803), and accumulated information on individuals' desire to adopt vaccine against COVID-19, views about the virus's effectiveness, and many knowledge-based socio-demographic factors that potentially impact the overall vaccination efforts. We found that, 12.08% of participants do not believe that vaccination against COVID-19 is necessary, but among the rest of the population, 44.33% of individuals are willing to be vaccinated once the vaccine is available, whereas 39.60% of the population responded that they will not be vaccinated immediately but will do so later.
ConclusionsDespite the participants' strong vaccine willingness, our findings revealed a troubling degree of lake of awareness and insignificant scientific knowledge about the COVID-19 pandemic and its associated vaccination programme. Vaccination hesitancy is not a barrier in this survey region, but poor vaccine availability and a lack of awareness campaigns may instill unfavorable beliefs in those who refuse to be vaccinated.
Objetivos: La rapidez de la vacunación es el único modo de luchar contra la COVID-19. Las dudas sobre la vacuna constituyen la mayor barrera contra esta estrategia. El objetivo principal de este estudio transversal fue analizar la aceptación de la vacuna contra la COVID-19 en la población general de Bengala occidental (India), así como investigar los factores asociados de manera independiente al deseo de recibir la vacuna por parte de las personas.
Métodos: Se distribuyó un cuestionario online por correo electrónico, Whatsapp, y otras plataformas de redes sociales, y se analizaron las respuestas utilizando el software SPSS (Versión 20).
Resultados: Realizamos una encuesta basada en web en Bengala occidental, India (N= 803), y acumulamos la información sobre el deseo de las personas de recibir la vacuna contra la COVID-19, las opiniones sobre la efectividad del virus, y muchos factores sociodemográficos basados en el conocimiento que tienen un impacto potencial en los esfuerzos globales sobre vacunación. Encontramos que el 12,08% de los participantes no creen en la necesidad de la vacunación contra la COVID-19 pero, entre el resto de la población, el 44,33% de los individuos desean ser vacunados una vez que se disponga de la vacuna, mientras que el 39,6% de la población respondió que no se vacunarían de inmediato, aunque lo harían más adelante.
Conclusiones: A pesar de la sólida voluntad de los participantes por la vacuna, nuestros hallazgos revelaron un grado preocupante de falta de concienciación y conocimiento científico insignificante acerca de la pandemia de COVID- 19 y su programa de vacunación asociado. Las dudas sobre la vacuna no son una barrera en la región de esta encuesta, pero la poca disponibilidad de la vacuna y la falta de campañas de concienciación puede infundir creencias desfavorables en aquellas personas que rechazan recibir la vacuna.
SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) or Coronavirus disease (COVID-19) is a devastating viral infection that still affects many places throughout the world.1 Along with supportive care and following government guidelines, there is an urgent need for massive vaccination to flatten the infectivity graph. On January 16, 2021, India initiated the world's largest COVID-19 vaccine programme to vaccinate its 900 million population.2 From the very beginning, only two COVID-19 vaccines, i.e., Covishield (Oxford-AstraZeneca vaccine) and Covaxin, the first indigenous vaccine produced by Bharat Biotech, have been approved for restricted emergency use in priority-based vaccination programmes.3 A total of 30 million healthcare and frontline workers were scheduled to be vaccinated in phase one. The bulk population was covered beginning in May 2021, starting with the elderly and those with co-morbidities, as well as those in the age groups of 45 to 60 years and 18 to 44 years.3 India had given out 33.2 crore doses to 27.4 crore people as of June 30, 2021. However, only 4% of India's population is fully vaccinated, compared to 45% in the United States and 48% in the United Kingdom. Only approximately 5% of the population of India is fully immunized. According to experts, vaccination rates must spike by the end of the year in order for the majority of Indians to be protected from the virus, which has claimed the lives of over 4.34 lakh people.4 Different human characteristics that persuade vaccination acceptance rates, such as beliefs, perceptions, and behaviors, may also play a crucial role in reaching the acceptable levels of community immunity obligatory to prevent the pandemic's spread.5 COVID-19 prevention measures, including the use of masks and social distancing, have been demonstrated to be helpful in slowing the virus's spread, but the widespread use of preventive vaccination will be critical to the long-term containment of the COVID-19 pandemic.6 Evidence-based health communication techniques are required to effectively address vaccination reluctance and create vaccine trust. In preparation for the COVID-19 vaccine deployment, one key part of communication is to understand the function of emotion.7 Other major aspects of vaccine dissemination and education, such as building trust and credibility of health agencies and scientific experts, conveying the safety and stringent standards enforced in the vaccine development process and facilitating equitable vaccine information dissemination across the world, can benefit from a focus on emotion.8
The goal of this study was to assess COVID-19 vaccine acceptance in West Bengal's (India) general population, as well as to look into the characteristics that were independently linked to individuals desire to take the vaccination. This online survey study was conducted when there was massive confusion about the COVID-19 vaccine in various parts of the country. These abilities are equivalent to health literacy abilities, which encompass people's knowledge, motivation and ability to locate, absorb and use health information, which is critical in the event of a pandemic.
MethodsStudy design and collection of dataFrom 22th February 2021 to 22th March 2021, this online survey was conducted among the Bengalee people of West Bengal, India. West Bengal is India's fourth most populous state, with a population of about 91 million people.9 Considering the pattern of previous questions published in the prior literature,10 a set of questionnaire was created using the Google form web survey architecture and data was collected by online compilation of the Google forms. The link to the online survey was distributed among the members of the study group via electronic mail (e-mail), WhatsApp and personal contacts. In order to enhance the number of individuals who received the invitation to the current survey, participants were also invited to share the study link with their friends and family. As a result of sharing the survey links, more individuals were able to participate in the survey. Participants were given a brief summary of the survey and its purpose, as well as the study protocol and a declaration of confidentiality and privacy, before beginning the questionnaire.
The inclusion criteria for the study were voluntary participation, participants living in West Bengal, India and also limited to subjects above the age of 18 years. Participants suffering from COVID-19, post COVID-19 complications and past history of COVID-19 were excluded from the study. The participants received no remuneration for their participation in the study. The Helsinki Declaration was also followed when conducting this survey.
Statistical analysisThe required sample size for the current study was calculated using a single population proportion with the following assumptions: 37% vaccine hesitancy in India according to a nationwide survey on COVID-19 vaccination hesitancy across 27 Indian states and union territories,11 95% confidence interval, 4% marginal error and a population of West Bengal of 91,276,115 (Census of India 2011).9 As a result, the study requires 672 participants (rounded to 680) in order to make adequate inferences about West Bengal's total population.
To summarize the data, categorical variables were summarized using frequency; percentage and Chi-square test were used to analyze differences. To account for the possibility of confounding, univariate and multivariate logistic regression analyses were used to examine the variables that affected the participants' knowledge of the COVID-19 vaccine and its acceptance. The participants' sexes, ages and educational levels were used as independent variables in logistic regression analyses. The results of logistic regression analyses were expressed as crude odd ratios (COR) and adjusted odd ratios (AOR) with 95% confidence intervals (95% CI). The Statistical Package for Social Sciences (SPSS, Version 20) was used to conduct all of the analyses. The standard statistically significant p value of 0.05 was used in this entire study.
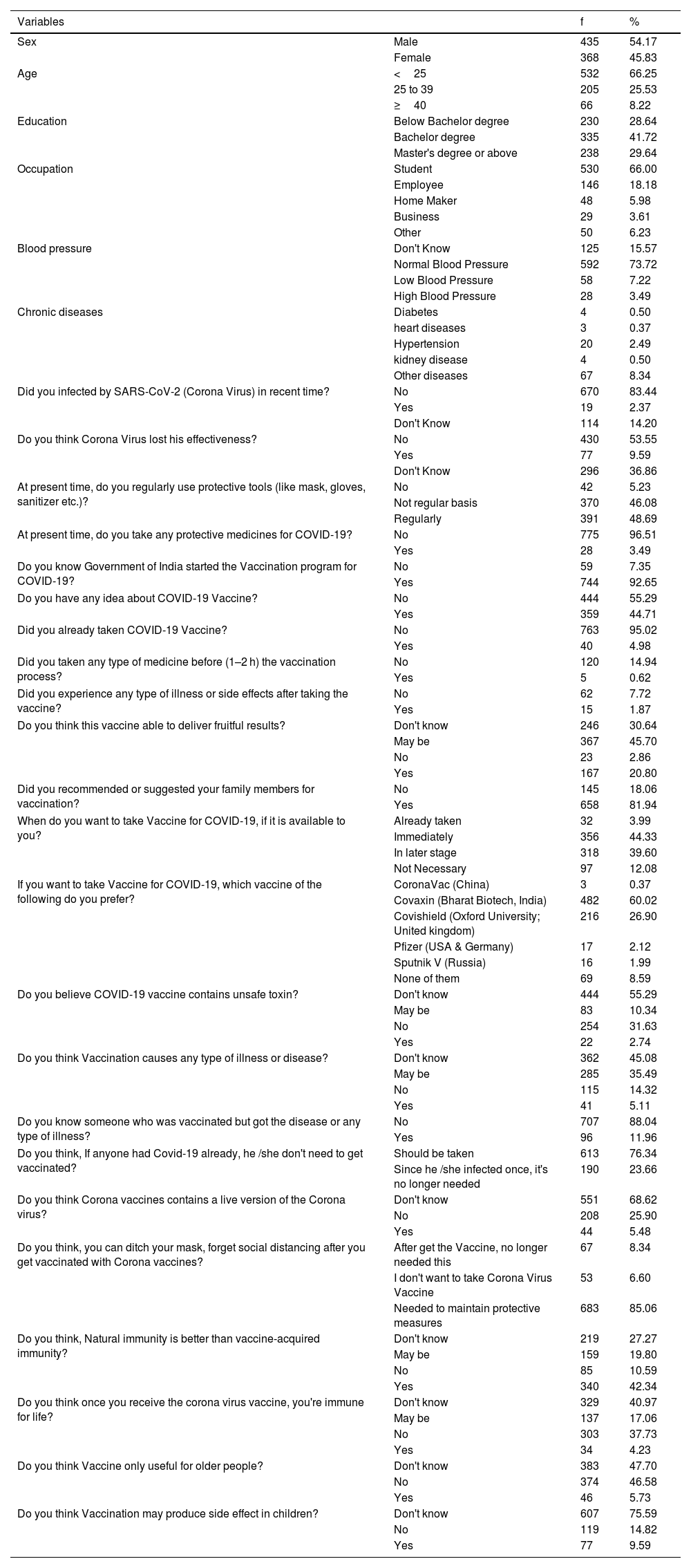
ResultsThere were a total of 803 individuals in this study, with 435 (54.17%) male and 368 (45.83%) female participants. The characteristics of the respondents divided into various groups (age, qualification, occupation, health problems, etc.) were presented in Table 1(Table 1). Among the entire participants, 66.25% of the individuals were under the age of 25 years and 41.72% were graduates or students in the process of graduating. Whereas, 25.53% of participants belonged in the middle age categories (25–39 years) and only 8.22% were represented by the upper 40 years of age limits. In terms of occupation, a large number of participants (66%) were students and a very small percentage of people listed their occupation as business (3.61%). As seen in Table 1, a small percentage of individuals had ongoing health issues such as high blood pressure and various chronic diseases. Despite the pandemic's severe stages, 83.44% of the total studied population said they had not been impacted by SARS-CoV-2 in the recent past. However, a small percentage of the participants (14.20%) stated that they had not been able to determine if they were COVID positive or not in recent times. Some tricky questions were asked to identify the COVID-19 associated knowledge among the participants. Different awareness-associated questions were asked to determine the participants' COVID-19 related expertise. In relation to this, 53.55% of the investigated populations effectively claimed that they did not believe the COVID-19 risk factor had been eliminated, while 36.86% of the people stated that they had no knowledge of the presence or lack of Corona virus effectiveness. Approximately 48.69% of participants used preventive measures (masks, sanitizers, social distancing, etc.) on a daily basis, while 46.08% did not follow the COVID protective guidelines on a regular basis. Surprisingly, 5.23% of those polled stated that they had taken no precautions in preparation for this catastrophic epidemic (Table 1).
Descriptive characteristics of the study participants.
| Variables | f | % | |
|---|---|---|---|
| Sex | Male | 435 | 54.17 |
| Female | 368 | 45.83 | |
| Age | <25 | 532 | 66.25 |
| 25 to 39 | 205 | 25.53 | |
| ≥40 | 66 | 8.22 | |
| Education | Below Bachelor degree | 230 | 28.64 |
| Bachelor degree | 335 | 41.72 | |
| Master's degree or above | 238 | 29.64 | |
| Occupation | Student | 530 | 66.00 |
| Employee | 146 | 18.18 | |
| Home Maker | 48 | 5.98 | |
| Business | 29 | 3.61 | |
| Other | 50 | 6.23 | |
| Blood pressure | Don't Know | 125 | 15.57 |
| Normal Blood Pressure | 592 | 73.72 | |
| Low Blood Pressure | 58 | 7.22 | |
| High Blood Pressure | 28 | 3.49 | |
| Chronic diseases | Diabetes | 4 | 0.50 |
| heart diseases | 3 | 0.37 | |
| Hypertension | 20 | 2.49 | |
| kidney disease | 4 | 0.50 | |
| Other diseases | 67 | 8.34 | |
| Did you infected by SARS-CoV-2 (Corona Virus) in recent time? | No | 670 | 83.44 |
| Yes | 19 | 2.37 | |
| Don't Know | 114 | 14.20 | |
| Do you think Corona Virus lost his effectiveness? | No | 430 | 53.55 |
| Yes | 77 | 9.59 | |
| Don't Know | 296 | 36.86 | |
| At present time, do you regularly use protective tools (like mask, gloves, sanitizer etc.)? | No | 42 | 5.23 |
| Not regular basis | 370 | 46.08 | |
| Regularly | 391 | 48.69 | |
| At present time, do you take any protective medicines for COVID-19? | No | 775 | 96.51 |
| Yes | 28 | 3.49 | |
| Do you know Government of India started the Vaccination program for COVID-19? | No | 59 | 7.35 |
| Yes | 744 | 92.65 | |
| Do you have any idea about COVID-19 Vaccine? | No | 444 | 55.29 |
| Yes | 359 | 44.71 | |
| Did you already taken COVID-19 Vaccine? | No | 763 | 95.02 |
| Yes | 40 | 4.98 | |
| Did you taken any type of medicine before (1–2 h) the vaccination process? | No | 120 | 14.94 |
| Yes | 5 | 0.62 | |
| Did you experience any type of illness or side effects after taking the vaccine? | No | 62 | 7.72 |
| Yes | 15 | 1.87 | |
| Do you think this vaccine able to deliver fruitful results? | Don't know | 246 | 30.64 |
| May be | 367 | 45.70 | |
| No | 23 | 2.86 | |
| Yes | 167 | 20.80 | |
| Did you recommended or suggested your family members for vaccination? | No | 145 | 18.06 |
| Yes | 658 | 81.94 | |
| When do you want to take Vaccine for COVID-19, if it is available to you? | Already taken | 32 | 3.99 |
| Immediately | 356 | 44.33 | |
| In later stage | 318 | 39.60 | |
| Not Necessary | 97 | 12.08 | |
| If you want to take Vaccine for COVID-19, which vaccine of the following do you prefer? | CoronaVac (China) | 3 | 0.37 |
| Covaxin (Bharat Biotech, India) | 482 | 60.02 | |
| Covishield (Oxford University; United kingdom) | 216 | 26.90 | |
| Pfizer (USA & Germany) | 17 | 2.12 | |
| Sputnik V (Russia) | 16 | 1.99 | |
| None of them | 69 | 8.59 | |
| Do you believe COVID-19 vaccine contains unsafe toxin? | Don't know | 444 | 55.29 |
| May be | 83 | 10.34 | |
| No | 254 | 31.63 | |
| Yes | 22 | 2.74 | |
| Do you think Vaccination causes any type of illness or disease? | Don't know | 362 | 45.08 |
| May be | 285 | 35.49 | |
| No | 115 | 14.32 | |
| Yes | 41 | 5.11 | |
| Do you know someone who was vaccinated but got the disease or any type of illness? | No | 707 | 88.04 |
| Yes | 96 | 11.96 | |
| Do you think, If anyone had Covid-19 already, he /she don't need to get vaccinated? | Should be taken | 613 | 76.34 |
| Since he /she infected once, it's no longer needed | 190 | 23.66 | |
| Do you think Corona vaccines contains a live version of the Corona virus? | Don't know | 551 | 68.62 |
| No | 208 | 25.90 | |
| Yes | 44 | 5.48 | |
| Do you think, you can ditch your mask, forget social distancing after you get vaccinated with Corona vaccines? | After get the Vaccine, no longer needed this | 67 | 8.34 |
| I don't want to take Corona Virus Vaccine | 53 | 6.60 | |
| Needed to maintain protective measures | 683 | 85.06 | |
| Do you think, Natural immunity is better than vaccine-acquired immunity? | Don't know | 219 | 27.27 |
| May be | 159 | 19.80 | |
| No | 85 | 10.59 | |
| Yes | 340 | 42.34 | |
| Do you think once you receive the corona virus vaccine, you're immune for life? | Don't know | 329 | 40.97 |
| May be | 137 | 17.06 | |
| No | 303 | 37.73 | |
| Yes | 34 | 4.23 | |
| Do you think Vaccine only useful for older people? | Don't know | 383 | 47.70 |
| No | 374 | 46.58 | |
| Yes | 46 | 5.73 | |
| Do you think Vaccination may produce side effect in children? | Don't know | 607 | 75.59 |
| No | 119 | 14.82 | |
| Yes | 77 | 9.59 |
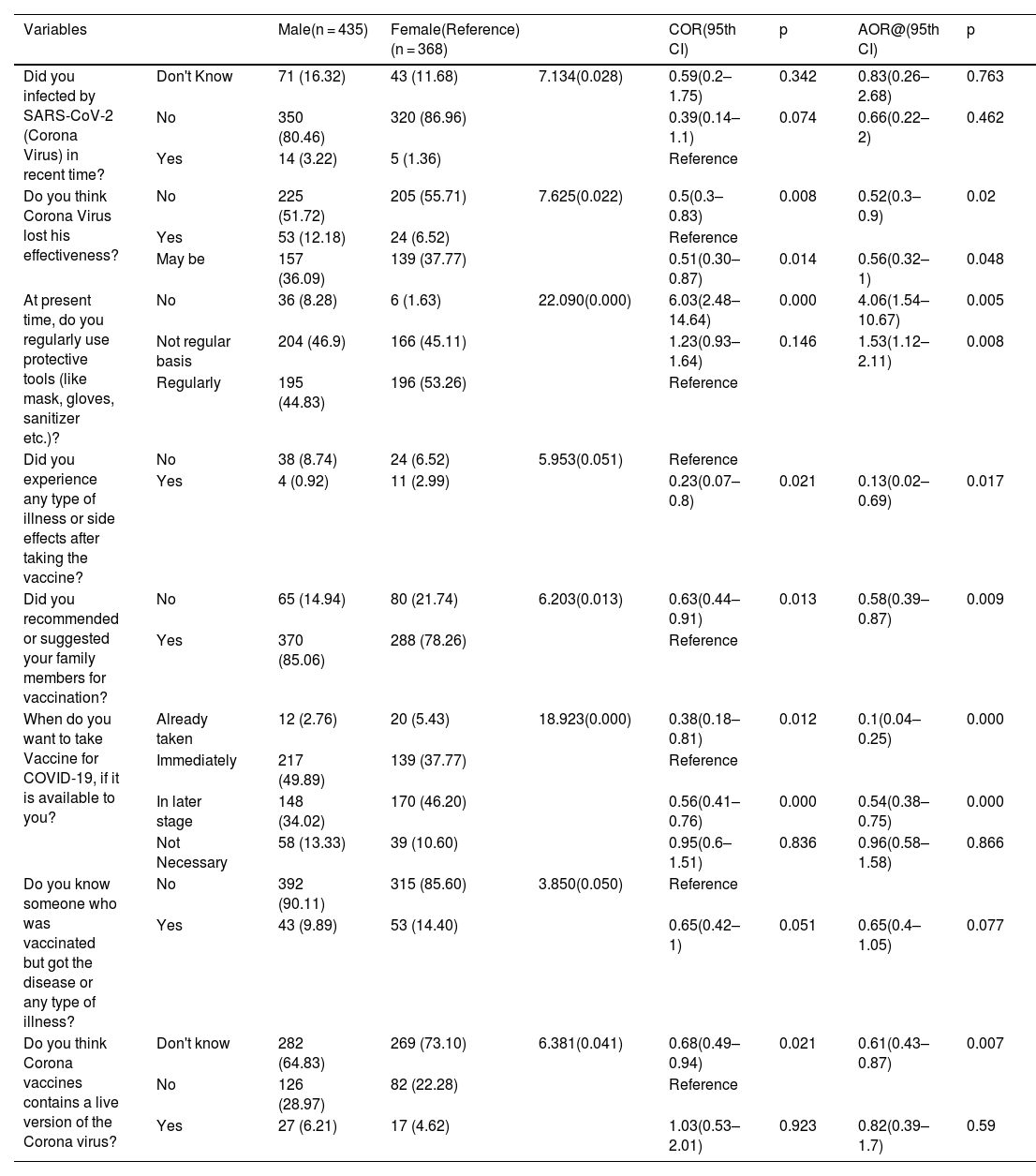
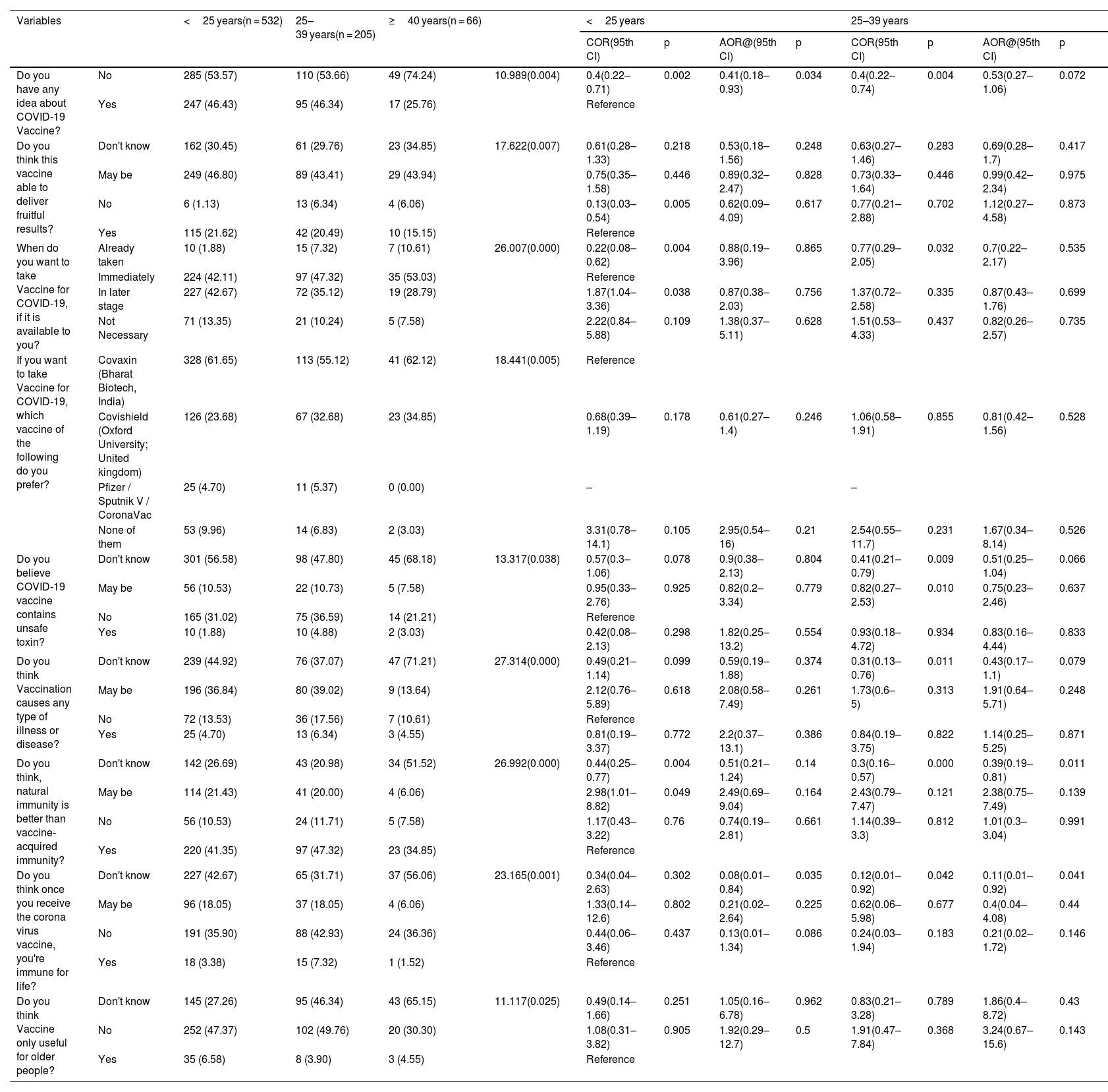
Both bivariate and multivariate logistic regression analyses were used to explore the COVID-19 vaccine's associated socio-demographic and behavioral significant factors among Bengal's population (Table 2,Table 3, & table S1). Female participants had more sensible knowledge about COVID-19 disease effectiveness than male participants (AOR: 0.52; CI: 0.3–0.9) and they also adhered to COVID-19 protective protocols far better than male participants. Despite the fact that higher educated individuals know about it, the corona virus hasn't lost its power (55% of máster's degree holders), they have failed to uphold government guidelines addressing COVID-19 disease on a regular basis (49.58% of máster's degree holders) (table S1). Males were shown to be more interested in becoming vaccinated than females, with the majority of males stating that they would take the vaccine as soon as it became available. While females expressed some hesitation about the vaccination, they made it apparent that they were interested in receiving the vaccine at a later stage rather than right away (AOR: 0.54; CI: 0.38–0.75) (Table 2). When it came to getting the COVID-19 vaccine, a substantial percentage of middle-aged people (>40 years) were eager to have it as soon as it became available, compared to the lower and above 25-year-old age groups of participants. It was also found that in both age groups, relatively few people stated that they did not wish to receive any form of vaccine (≤ 25 year AOR: 1.38; CI: 0.37–5.11; ≥25 year AOR: 0.82; CI: 0.26–2.57) (Table 3). According to the responses of the overall investigated population, a big majority of people had conflicting beliefs and had very little scientific understanding regarding the COVID-19 vaccination. They strongly said that they had no idea whether the corona vaccine contained any dangerous toxins or not (Table 3).
Associations between sex and COVID-19 vaccine awareness.
| Variables | Male(n = 435) | Female(Reference)(n = 368) | COR(95th CI) | p | AOR@(95th CI) | p | ||
|---|---|---|---|---|---|---|---|---|
| Did you infected by SARS-CoV-2 (Corona Virus) in recent time? | Don't Know | 71 (16.32) | 43 (11.68) | 7.134(0.028) | 0.59(0.2–1.75) | 0.342 | 0.83(0.26–2.68) | 0.763 |
| No | 350 (80.46) | 320 (86.96) | 0.39(0.14–1.1) | 0.074 | 0.66(0.22–2) | 0.462 | ||
| Yes | 14 (3.22) | 5 (1.36) | Reference | |||||
| Do you think Corona Virus lost his effectiveness? | No | 225 (51.72) | 205 (55.71) | 7.625(0.022) | 0.5(0.3–0.83) | 0.008 | 0.52(0.3–0.9) | 0.02 |
| Yes | 53 (12.18) | 24 (6.52) | Reference | |||||
| May be | 157 (36.09) | 139 (37.77) | 0.51(0.30–0.87) | 0.014 | 0.56(0.32–1) | 0.048 | ||
| At present time, do you regularly use protective tools (like mask, gloves, sanitizer etc.)? | No | 36 (8.28) | 6 (1.63) | 22.090(0.000) | 6.03(2.48–14.64) | 0.000 | 4.06(1.54–10.67) | 0.005 |
| Not regular basis | 204 (46.9) | 166 (45.11) | 1.23(0.93–1.64) | 0.146 | 1.53(1.12–2.11) | 0.008 | ||
| Regularly | 195 (44.83) | 196 (53.26) | Reference | |||||
| Did you experience any type of illness or side effects after taking the vaccine? | No | 38 (8.74) | 24 (6.52) | 5.953(0.051) | Reference | |||
| Yes | 4 (0.92) | 11 (2.99) | 0.23(0.07–0.8) | 0.021 | 0.13(0.02–0.69) | 0.017 | ||
| Did you recommended or suggested your family members for vaccination? | No | 65 (14.94) | 80 (21.74) | 6.203(0.013) | 0.63(0.44–0.91) | 0.013 | 0.58(0.39–0.87) | 0.009 |
| Yes | 370 (85.06) | 288 (78.26) | Reference | |||||
| When do you want to take Vaccine for COVID-19, if it is available to you? | Already taken | 12 (2.76) | 20 (5.43) | 18.923(0.000) | 0.38(0.18–0.81) | 0.012 | 0.1(0.04–0.25) | 0.000 |
| Immediately | 217 (49.89) | 139 (37.77) | Reference | |||||
| In later stage | 148 (34.02) | 170 (46.20) | 0.56(0.41–0.76) | 0.000 | 0.54(0.38–0.75) | 0.000 | ||
| Not Necessary | 58 (13.33) | 39 (10.60) | 0.95(0.6–1.51) | 0.836 | 0.96(0.58–1.58) | 0.866 | ||
| Do you know someone who was vaccinated but got the disease or any type of illness? | No | 392 (90.11) | 315 (85.60) | 3.850(0.050) | Reference | |||
| Yes | 43 (9.89) | 53 (14.40) | 0.65(0.42–1) | 0.051 | 0.65(0.4–1.05) | 0.077 | ||
| Do you think Corona vaccines contains a live version of the Corona virus? | Don't know | 282 (64.83) | 269 (73.10) | 6.381(0.041) | 0.68(0.49–0.94) | 0.021 | 0.61(0.43–0.87) | 0.007 |
| No | 126 (28.97) | 82 (22.28) | Reference | |||||
| Yes | 27 (6.21) | 17 (4.62) | 1.03(0.53–2.01) | 0.923 | 0.82(0.39–1.7) | 0.59 |
@after adjusting the effect of age, education, and occupation.
Associations between age and COVID-19 vaccine awareness.
| Variables | <25 years(n = 532) | 25–39 years(n = 205) | ≥40 years(n = 66) | <25 years | 25–39 years | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| COR(95th CI) | p | AOR@(95th CI) | p | COR(95th CI) | p | AOR@(95th CI) | p | ||||||
| Do you have any idea about COVID-19 Vaccine? | No | 285 (53.57) | 110 (53.66) | 49 (74.24) | 10.989(0.004) | 0.4(0.22–0.71) | 0.002 | 0.41(0.18–0.93) | 0.034 | 0.4(0.22–0.74) | 0.004 | 0.53(0.27–1.06) | 0.072 |
| Yes | 247 (46.43) | 95 (46.34) | 17 (25.76) | Reference | |||||||||
| Do you think this vaccine able to deliver fruitful results? | Don't know | 162 (30.45) | 61 (29.76) | 23 (34.85) | 17.622(0.007) | 0.61(0.28–1.33) | 0.218 | 0.53(0.18–1.56) | 0.248 | 0.63(0.27–1.46) | 0.283 | 0.69(0.28–1.7) | 0.417 |
| May be | 249 (46.80) | 89 (43.41) | 29 (43.94) | 0.75(0.35–1.58) | 0.446 | 0.89(0.32–2.47) | 0.828 | 0.73(0.33–1.64) | 0.446 | 0.99(0.42–2.34) | 0.975 | ||
| No | 6 (1.13) | 13 (6.34) | 4 (6.06) | 0.13(0.03–0.54) | 0.005 | 0.62(0.09–4.09) | 0.617 | 0.77(0.21–2.88) | 0.702 | 1.12(0.27–4.58) | 0.873 | ||
| Yes | 115 (21.62) | 42 (20.49) | 10 (15.15) | Reference | |||||||||
| When do you want to take Vaccine for COVID-19, if it is available to you? | Already taken | 10 (1.88) | 15 (7.32) | 7 (10.61) | 26.007(0.000) | 0.22(0.08–0.62) | 0.004 | 0.88(0.19–3.96) | 0.865 | 0.77(0.29–2.05) | 0.032 | 0.7(0.22–2.17) | 0.535 |
| Immediately | 224 (42.11) | 97 (47.32) | 35 (53.03) | Reference | |||||||||
| In later stage | 227 (42.67) | 72 (35.12) | 19 (28.79) | 1.87(1.04–3.36) | 0.038 | 0.87(0.38–2.03) | 0.756 | 1.37(0.72–2.58) | 0.335 | 0.87(0.43–1.76) | 0.699 | ||
| Not Necessary | 71 (13.35) | 21 (10.24) | 5 (7.58) | 2.22(0.84–5.88) | 0.109 | 1.38(0.37–5.11) | 0.628 | 1.51(0.53–4.33) | 0.437 | 0.82(0.26–2.57) | 0.735 | ||
| If you want to take Vaccine for COVID-19, which vaccine of the following do you prefer? | Covaxin (Bharat Biotech, India) | 328 (61.65) | 113 (55.12) | 41 (62.12) | 18.441(0.005) | Reference | |||||||
| Covishield (Oxford University; United kingdom) | 126 (23.68) | 67 (32.68) | 23 (34.85) | 0.68(0.39–1.19) | 0.178 | 0.61(0.27–1.4) | 0.246 | 1.06(0.58–1.91) | 0.855 | 0.81(0.42–1.56) | 0.528 | ||
| Pfizer / Sputnik V / CoronaVac | 25 (4.70) | 11 (5.37) | 0 (0.00) | – | – | ||||||||
| None of them | 53 (9.96) | 14 (6.83) | 2 (3.03) | 3.31(0.78–14.1) | 0.105 | 2.95(0.54–16) | 0.21 | 2.54(0.55–11.7) | 0.231 | 1.67(0.34–8.14) | 0.526 | ||
| Do you believe COVID-19 vaccine contains unsafe toxin? | Don't know | 301 (56.58) | 98 (47.80) | 45 (68.18) | 13.317(0.038) | 0.57(0.3–1.06) | 0.078 | 0.9(0.38–2.13) | 0.804 | 0.41(0.21–0.79) | 0.009 | 0.51(0.25–1.04) | 0.066 |
| May be | 56 (10.53) | 22 (10.73) | 5 (7.58) | 0.95(0.33–2.76) | 0.925 | 0.82(0.2–3.34) | 0.779 | 0.82(0.27–2.53) | 0.010 | 0.75(0.23–2.46) | 0.637 | ||
| No | 165 (31.02) | 75 (36.59) | 14 (21.21) | Reference | |||||||||
| Yes | 10 (1.88) | 10 (4.88) | 2 (3.03) | 0.42(0.08–2.13) | 0.298 | 1.82(0.25–13.2) | 0.554 | 0.93(0.18–4.72) | 0.934 | 0.83(0.16–4.44) | 0.833 | ||
| Do you think Vaccination causes any type of illness or disease? | Don't know | 239 (44.92) | 76 (37.07) | 47 (71.21) | 27.314(0.000) | 0.49(0.21–1.14) | 0.099 | 0.59(0.19–1.88) | 0.374 | 0.31(0.13–0.76) | 0.011 | 0.43(0.17–1.1) | 0.079 |
| May be | 196 (36.84) | 80 (39.02) | 9 (13.64) | 2.12(0.76–5.89) | 0.618 | 2.08(0.58–7.49) | 0.261 | 1.73(0.6–5) | 0.313 | 1.91(0.64–5.71) | 0.248 | ||
| No | 72 (13.53) | 36 (17.56) | 7 (10.61) | Reference | |||||||||
| Yes | 25 (4.70) | 13 (6.34) | 3 (4.55) | 0.81(0.19–3.37) | 0.772 | 2.2(0.37–13.1) | 0.386 | 0.84(0.19–3.75) | 0.822 | 1.14(0.25–5.25) | 0.871 | ||
| Do you think, natural immunity is better than vaccine-acquired immunity? | Don't know | 142 (26.69) | 43 (20.98) | 34 (51.52) | 26.992(0.000) | 0.44(0.25–0.77) | 0.004 | 0.51(0.21–1.24) | 0.14 | 0.3(0.16–0.57) | 0.000 | 0.39(0.19–0.81) | 0.011 |
| May be | 114 (21.43) | 41 (20.00) | 4 (6.06) | 2.98(1.01–8.82) | 0.049 | 2.49(0.69–9.04) | 0.164 | 2.43(0.79–7.47) | 0.121 | 2.38(0.75–7.49) | 0.139 | ||
| No | 56 (10.53) | 24 (11.71) | 5 (7.58) | 1.17(0.43–3.22) | 0.76 | 0.74(0.19–2.81) | 0.661 | 1.14(0.39–3.3) | 0.812 | 1.01(0.3–3.04) | 0.991 | ||
| Yes | 220 (41.35) | 97 (47.32) | 23 (34.85) | Reference | |||||||||
| Do you think once you receive the corona virus vaccine, you're immune for life? | Don't know | 227 (42.67) | 65 (31.71) | 37 (56.06) | 23.165(0.001) | 0.34(0.04–2.63) | 0.302 | 0.08(0.01–0.84) | 0.035 | 0.12(0.01–0.92) | 0.042 | 0.11(0.01–0.92) | 0.041 |
| May be | 96 (18.05) | 37 (18.05) | 4 (6.06) | 1.33(0.14–12.6) | 0.802 | 0.21(0.02–2.64) | 0.225 | 0.62(0.06–5.98) | 0.677 | 0.4(0.04–4.08) | 0.44 | ||
| No | 191 (35.90) | 88 (42.93) | 24 (36.36) | 0.44(0.06–3.46) | 0.437 | 0.13(0.01–1.34) | 0.086 | 0.24(0.03–1.94) | 0.183 | 0.21(0.02–1.72) | 0.146 | ||
| Yes | 18 (3.38) | 15 (7.32) | 1 (1.52) | Reference | |||||||||
| Do you think Vaccine only useful for older people? | Don't know | 145 (27.26) | 95 (46.34) | 43 (65.15) | 11.117(0.025) | 0.49(0.14–1.66) | 0.251 | 1.05(0.16–6.78) | 0.962 | 0.83(0.21–3.28) | 0.789 | 1.86(0.4–8.72) | 0.43 |
| No | 252 (47.37) | 102 (49.76) | 20 (30.30) | 1.08(0.31–3.82) | 0.905 | 1.92(0.29–12.7) | 0.5 | 1.91(0.47–7.84) | 0.368 | 3.24(0.67–15.6) | 0.143 | ||
| Yes | 35 (6.58) | 8 (3.90) | 3 (4.55) | Reference | |||||||||
@after adjusting the effect of sex, education, and occupation.
According to our survey, 92.65% of the population was aware of the government's vaccination policy and 44.53% of individuals very much wanted to get the vaccine as soon as possible, but they were unable to draw any conclusions about vaccine efficacy. Despite their lack of understanding regarding the corona vaccination, several participants were reported to have gotten it for their family members (81.94%). In terms of vaccination choice, the majority of people (60.02%) voted to use Covaxin (Bharat Biotech, India) instead of other vaccines (Table 1). Despite suggesting a negative or positive response, the participants did not show any constrictive points when it came to negative beliefs. Instead, they preferred to stand in a neutral posture. Both the male and female groups significantly indicated that they were unaware that the COVID vaccine contained a live variant of the coronavirus (AOR: 0.61; CI: 0.43–0.87) (Table 2). Surprisingly, educated participants gave identical responses to vaccination knowledge, while the majority of masters and graduate individuals did not produce any constrictive responses when it came to scientific information (Below Graduate AOR: 2.4; CI: 1.53–3.77; Graduate AOR: 1.81; CI: 1.19–2.74) (table S1).
DiscussionMany scientific laboratories and academic organizations are working to develop new types of vaccine to combat the new coronavirus, which has killed over half a million people and damaged economies around the world.12 It is well known that, if vaccination rates are insufficient, herd immunity will not develop and the most vulnerable population groups will not be protected.13 As a result, it's vital to know whether the general public intends to get vaccinated against COVID-19 ahead of time so that public health professionals may develop and implement targeted programmes to raise public awareness about the importance of vaccination. The goal of this study was to monitor the acceptance rate of the COVID-19 vaccination in the general population of West Bengal (India) and to observe if there was a link between vaccine acceptance and vaccine awareness.
According to the findings of this study, the targeted community had a very low degree of vaccine hesitancy, which is significantly correlated with earlier scientific studies, in which researchers clearly stated that a far from universal enthusiasm to embrace COVID-19 vaccination is reason for worry. Asian countries with significant trust in central governments tended to have high levels of acceptance (China, South Korea and Singapore).14 Acceptance was also found to be rather high in middle-income nations such as Brazil, India and South Africa.15 Differences in vaccine coverage between nations could potentially postpone worldwide control of the pandemic and the accompanying societal and economic recovery unless and until the roots of such extensive diversity in readiness to take a COVID-19 vaccine are properly understood and addressed.14-16 Our study demonstrated a higher rate of COVID-19 vaccine willingness among the examined population of West Bengal, India, which is shown to be strongly, associated with Gautam et al., (2020) findings. According to Gautam et al., 77.27% of the investigated populations were extremely likely to take the COVID-19 vaccination, with only 5.3% of those who did not wish to receive the vaccine and 12.24% of those who were unsure whether to take it or not.17 Similarly, Bhartiya et al., made a comparable observation, which is significantly associated with our finding that 79% of people wanted to be vaccinated after the vaccine became available.18
Despite a high level of willingness to get the COVID-19 vaccinations, we found that our study population had a relatively poor level of vaccine knowledge, which may be a significant cause of vaccine hesitation among those who do not want to accept the vaccine. Furthermore, a variety of unfavorable beliefs and inaccurate scientific facts about COVID-19 and its accompanying vaccination campaign may also play a notable role in stifling vaccination willingness among those individuals. Similar findings were previously seen in China, the United States and Egypt among people who refused to accept the COVID -19 vaccines.19–21 People's psychological urge to interpret the unexpected events related to the COVID-19 epidemic has resulted in widespread unfavorable beliefs.22 Furthermore, the conspiracy hypothesis has been linked to vaccination apprehension among the Saudi populace, such as during the H1N1 pandemic and influenza vaccine.23
Building public trust in vaccination programmes requires obvious and dependable communication from government leaders. Explaining how vaccines operate as well as how they are created, from recruiting to authorization, depending on safety and effectiveness is part of this.8 Based on our study, female participants have more practical knowledge of the pandemic than male participants, but males have a stronger readiness to receive the vaccine as soon as it becomes available. Similarly, in contrast to younger people, middle-aged people are more likely to receive vaccines. Females were far more likely than males to remember the pandemic guidelines, but it was surprisingly noted that highly qualified participants did not follow COVID principles on a regular basis. Moreover, the majority of people are willing to get vaccinated, but many are extremely confused regarding vaccine efficacy. A large number of those polled suggested their family members get the vaccine, but they did not have significant knowledge of its effectiveness. Effective seminars and justified explanations of vaccine efficacy, COVID rule implementation, and population broad coverage are the only ways to raise community awareness.
Similar suggestions were previously reported by Bhowmick et al., who found a significant communication gap regarding COVID-19 awareness as well among the studied people.24 It will also be critical to build public trust in regulatory agency evaluations of vaccination protection and usefulness. As has been found with persuading people to comply with COVID-19 control measures, credible and culturally aware health communication is critical in promoting beneficial health behaviors.25,26
According to the 2011 Census report of India, there are 94 crore people above the age of 18 years, with a total population of 136 crore.9 Only 11.40% of the adult population had been vaccinated as of the end of the first week of August 2020.27 Vaccine hesitation is not a factor in West Bengal's and India's low vaccination rates; instead, our survey results show that a lack of vaccine availability is a key factor. As per this research, the majority of people want vaccines as soon as possible, thus the government has to devise a more effective approach for dealing with this extremely sensitive topic. Wouters et al. previously reported that Vietnam (98%), India (91%), China (91%), Denmark (87%) and South Korea (87%) had the highest vaccine acceptance rates, while Serbia (38%), Croatia (41%), France (44%), Lebanon (44%) and Paraguay had the lowest (51%). In this report, they also suggested that the lack of COVID vaccine availability has a detrimental impact on vaccination programmes and that this could be one of the major causes of poor vaccination rates in developing countries; this conclusion is significantly associated with our findings.28 Not only do vaccine mandates mislead the general public, but a lack of social awareness regarding vaccination programmes and SARS-CoV-2 also negatively influences the general public.29 The government should take appropriate steps to address these issues.
The Web-based survey method is not a good alternative to field-based study. There are some limitations to this study, which include lower response rates, limited access to the internet / devices and lack of follow-up data.
ConclusionIn conclusion, only a small percentage of the investigated population had received vaccines in recent times, but the vast majority of the population desired to be vaccinated as soon as feasible. In West Bengal, a far lower percentage of ordinary people appear to be cagey about the COVID-19 vaccination program, which was directly reflected in the reduced hesitation rate. Despite their great desire to receive the vaccine, the majority of people have very poor awareness of the COVID-19 vaccine. Various negative beliefs and a lack of factual understanding cause a great deal of uncertainty among those who refuse to be vaccinated. According to this finding, highly qualified people do not follow COVID guidelines on a regular basis, but they are aware of the consequences. The effectiveness of the COVID vaccination was found to have a very poor level of awareness and scientific knowledge, raising questions about the government policy associated with the vaccine promotion programme. Government agencies, health care providers, and other authorities should find this report beneficial in reducing the impact of vaccine reluctance. We tried to provide a thorough understanding of West Bengal's current COVID-19 vaccination status, which may pave the way for formulating a new vaccination strategy in the upcoming days.
Authorship statementSKD, AP and SSK outlined the entire study design and ground work; SS and JB involved in data collection and communication; SS, AP and JB performed data analysis and SS, AP, SKD and KMA participated in data analysis and manuscript writing; SSK, BG, KMA performed review and editing; AP and SKD supervised the entire research work. All authors approved the final version of the manuscript.
Ethical approvalThis study involved secondary data analyses of data that was collected by online survey method using Google form. The data collection method was not invasive and had been performed in accordance with the declaration of Helsinki. The complete study design was approved by the Institutional Ethics Committee (Human) University of Gour Banga, Malda, West Bengal, India (Approval no. UGB/IEC (Human)/0001–21).
FundingNo funding was received for conducting this study.
The authors are appreciative to all of the study participants and questioner distributors for their active engagement and commitment to this survey-based research.