Trigeminal neuralgia (TN) is a neuropathic pain, usually unilateral, affecting one or more trigeminal nerve innervation territories. The current study aimed to evaluate the effectiveness of acupuncture in TN pain control.
MethodsAn integrative review was developed on Medline (Pubmed), LILACS (BVS) and Cochrane Library databases. Keywords “trigeminal neuralgia” AND “acupuncture” were combined in different ways to ensure a wide search of primary studies. Article reference lists were also screened. Inclusion criteria comprised clinical studies developed in humans, without date publication limit, published in languages English, Portuguese and Spanish, performing any type of acupuncture therapy for TN pain control.
ResultsAmong the six studies selected, most were randomized controlled clinical trials, developed in China. Only one study performed a retrospective cross-sectional. To assess pain, most used the VAS scale. There were very similar methods concerning points selection and treatment protocols. All studies found a significant decrease in pain frequency or intensity, disregarding the type of acupuncture applied.
ConclusionAcupuncture therapy seems to decrease frequency and intensity of TN pain episodes, alone or in combination with gold standard medications. However, there is a need for standardizing methodological issues and prospective evaluations.
La neuralgia del trigémino (NT) es un dolor neuropático, normalmente unilateral, que afecta a uno o más de los territorios de innervación del trigémino. El objetivo de este estudio fue evaluar la efectividad de la acupuntura para el control del dolor de la NT.
MétodosSe desarrolló una revisión integradora en las bases de datos de Medline (Pubmed), LILACS (BVS) y Cochrane Library. Se combinaron de diferentes modos las palabras clave “neuralgia del trigémino” Y “acupuntura” para garantizar una búsqueda amplia de los estudios primarios. También se supervisaron los listados de referencia de los artículos. Los criterios de inclusión incluyeron los estudios clínicos desarrollados en humanos, sin límite de fecha de publicación, publicados en inglés, portugués y español, en los que se realizó cualquier tipo de acupuntura para el control del dolor de la NT.
ResultadosEntre los seis estudios seleccionados, la mayoría eran ensayos clínicos controlados aleatorios desarrollados en China. Sólo un estudio realizó una retrospectiva transversal. Para evaluar el dolor, muchos estudios utilizaron la escala EVA. Se encontraron métodos muy similares en cuanto a la selección de los puntos y los protocolos de tratamiento. Todos los estudios hallaron una reducción significativa en cuanto a frecuencia o intensidad del dolor, independientemente del tipo de acupuntura aplicada.
ConclusiónLa acupuntura parece reducir la frecuencia e intensidad de los episodios de dolor en la NT, en solitario o en combinación con medicamentos de referencia. Sin embargo, son necesarias la estandarización de las cuestiones metodológicas y las evaluaciones prospectivas.
Trigeminal neuralgia (TN) is a chronic neuropathic disease affecting the fifth cranial nerve pair, restricted to one or more divisions of this nerve.1 Apart from TN related to multiple sclerosis, the pain usually affects one side of the face.2 It has an abrupt onset and typically lasts only a few seconds (2minutes at maximum). Patients may report their pain as arising spontaneously, but these pain paroxysms can always be triggered by innocuous mechanical stimuli or movements, and are described as a stabbing sensation, electric shock or penetrating.3,4 Chewing, brushing teeth, talking, touching the region and cold wind can trigger pain and be debilitating or disabling.5 Despite the low prevalence (0.03% to 0.3%), TN is the most common neuralgia of the head and neck.4,6 The condition generally affects woman and people over 60 years.6 The annual incidence in those over 80 it is equivalent to 25.9 per 100,000 people.1
The International Association for the Study of Pain defines trigeminal neuralgia as “sudden, usually unilateral, severe, brief, stabbing, recurrent episodes of pain in the distribution of one or more branches of the trigeminal nerve”.7 It can be classified into three diagnostic categories: classical, secondary, and idiopathic (ITN). Classical TN is related with vascular compression that is responsible for producing anatomical changes in the trigeminal nerve root.3 Secondary TN happens due to an underlying neurological disease as arteriovenous malformations, certain brain tumours or multiple sclerosis.1,8 ITN is defined when the etiology of TN remains uncertain and symptoms occur without secondary causes or vascular compression.1
The International Headache Society divides TN into two distinct categories. The typical, “classic” or type 1 causes intense facial pain whose painful episode lasts up to 2minutes, and may persist for several hours.1 The atypical or type 2 presents continuous facial pain, but unlike NT1, it is constant and less severe.1,3 These classifications are not related to the etiology of the disease.9
Treatment options include medication, surgery and complementary therapies.1 Carbamazepine and oxcarbazepine are the first line treatment choice.3 Surgical management may be indicated in cases of decreased therapeutic effect or intolerance to medications.10 However, the recurrence of pain after neurosurgical intervention is frequent.11 Acupuncture has been used to treat TN due the analgesic effect through the release of endorphins, enkephalins and serotonins. Manual acupuncture and electro-acupuncture seem to improve response rate and recurrence rate, with few side effects, those may include hematoma or ecchymosis around application of the needles, metal allergy or local infection.12,13 The present review aims to address the current evidence on the effectiveness of acupuncture therapy on TN pain control.
MethodsThis is an integrative literature review, one of the research methods used on Evidence-based Practice, which allows to incorporate evidence on practical decisions.14 This study followed five stages: 1) identification of the topic and choosing a guiding question; 2) establishment of criteria for inclusion and exclusion of articles; 3) definition of the information to be extracted from selected studies; 4) evaluation of the selected studies; 5) analysis and summary of results, and review presentation.15 The question guiding this review was: What scientific evidence is available in the literature on the effects of acupuncture for controlling pain related to TN?
Clinical studies performed in humans, with no publication date limit, applying any type of acupuncture therapy to control TN pain were included. Articles were indexed in MEDLINE – Medical Literature Analysis and Retrieval System Online (via PubMed), LILACS – Latin American Literature Health Sciences (via BVS), and Cochrane Library. To define keywords, we used PICO strategy, whose abbreviation stands for P (Patient/Problem), I (Intervention or indicators), C (comparison), and O (Outcomes). Keywords were combined in different ways, comprising: “trigeminal neuralgia” AND “acupuncture” on PubMed and Cochrane Library; “acupuncture therapy” AND “trigeminal neuralgia” and “acupuncture analgesia” AND “trigeminal neuralgia” on BVS.
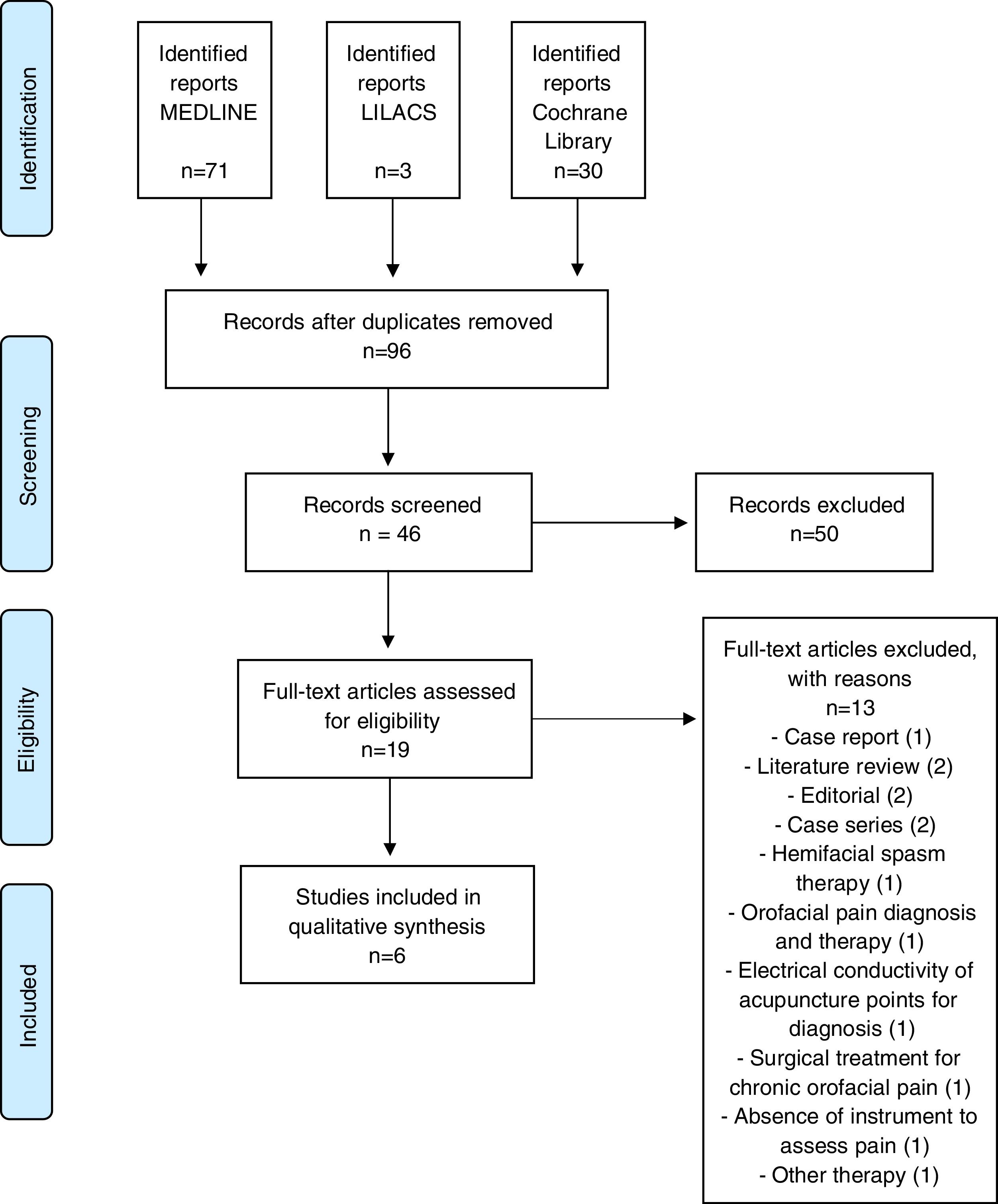
Papers published in Portuguese, English and Spanish were selected. Additionally, we performed a search on paper's reference lists. Revisions, editorials, reports or case series, studies in animals were excluded. Two independent reviewers performed searches. Articles were selected after evaluation of three steps: title, abstract and qualitative analysis of the full texts. The selection process can be seen in Figure 1 through the flowchart using PRISMA Standards.16
Identification of studies according PRISMA recommendation.16.
The final selection retrieved six studies, which were included for qualitative synthesis. In relation to countries where studies were developed, most were carried out in China (2), the remain countries contributed with one study (Brazil, South Korea, Israel, and Denmark).
Five studies were published between 2010 and 2019, and one in 1983. Regarding the study design, one was a retrospective cross-sectional study and five were clinical studies, of which four articles were controlled clinical trials.
Studies sample size presented a huge variation. The largest sample had 116 participants, and the smallest had three participants.17,18 Concerning individuals age range, all studies were conducted in adults (19-78 years).
Manual acupuncture was the only cited method. Acupoint LI4 was the main point utilized among studies.10,17–20 Acupoints ST2 and ST7 were used in four studies.10,17–19 Length of treatment varied from ten days to 18 months, and session's duration ranged from 15 to 30minutes in most studies.
Three instruments were identified to assess the degree of pain control, being the Visual Analogue Scale (VAS) the most used. Questionnaires and quantitative sensory tests were applied in two studies. All studies included found a significant decrease in pain frequency or intensity. The detailed information can be seen in Table 1.
Distribution of studies according authors, type of research, sample, pain evaluation, protocol and points used and main results.
| Author /year | Country | Study design | Sample | Instrument | Protocol | Points | Results |
|---|---|---|---|---|---|---|---|
| Jie Gao et al 2019.17 | China | Double-blind controlled clinical trial quasi-randomized. | 116 | VAS | 1 weekly session, 20 min/session for 10 weeks. | ST44, LI4, LI3, Yuyao; B2, GB14, SI18; ST2; ST3, ST7; ST6. | Significant decrease in average pain intensity. |
| Ichida et al 2017.10 | Brazil | Double-blind controlled clinical trial. | 90 | VAS+QST | 1 weekly session, 20min / session for 10 weeks. | LI4, LI3, ST44, B2, GB14, Yuyao, ST2, ST3, Sl18, ST6, ST7, and extra point in mandibular branch. | Significant decrease in average pain intensity. |
| He and Zhang 2012.19 | China | Randomized controlled clinical Trial. | 65 | VAS | 2 cycles of 10 days each, with alternate daily 30min sessions and an interval of 1 week between cycles. | ST7, B2, ST2, CV24, LG4 e LR3. | Significant decrease in the frequency and intensity of pain, except duration. |
| Ahn et al 2011.21 | South Korea | Randomized controlled clinical Trial pilot. | 49 | VAS | CA: TA: 6 sessions for 3 weeks, 20min / session. Until 12 sessions maximum for 6 weeks. EA: 2 sessions in the first week. 3 sessions after 1 week break. | TA: obligatory points (4 points of Korean Acupuncture of the five Elements) and individual points (0-4 points Ah-Shi, with an additional 2-5 points). EA: 3 cardinal points and 1-2 additional points. | TA or CA promoted reduction of pain, difference between therapies not significant. |
| Noiman et al 2010.20 | Israel | Retrospective cross-sectional study. | 4 | VAS | 6 to 10 weekly sessions, 30 min/session for 18 months. | LV3, LI4 and additional points on head and neck based on the clinical condition of each patient. | One TN's patient achieved significant pain improvement (25%). |
| Hansen and Hansen 1983.18 | Denmark | Randomized clinical Trial. | 3 | Questio-nnaire | 10 sessions, for 10 days, 15min per session | GB14, Taiyang, TH5, ST2, ST3, ST6, ST7, ST44 e LI4. | Pain reduction is significantly greater in the post-acupuncture periods compared to the post-placebo periods. |
Legend: TN=Trigeminal Neuralgia; VAS=Visual Analog Scale; QST=Quantitative Sensory Tests; CA: Combined Acupuncture; TA: Traditional Acupuncture; EA: ear acupuncture.
In this review we sought to evaluate the literature on the efficacy of acupuncture treatment in TN pain. All studies included demonstrated some level of decrease in pain intensity or frequency among TN patients. Overall, the results indicate that acupuncture therapy, compared to sham, shows better results in controlling TN pain.
In a study to verify a possible explanation for the analgesic power of acupuncture, Nappi et al (1982) reported that plasma liberation of beta-lipotrophin (ßLPH) and beta-endrophin (ßEF) after acupuncture may explain its analgesic effect. ßLPH is a precursor molecule of βEF and has a central effect similar to morphine.22 Thus, the application of acupuncture promoted an increase in TN patients’ plasma levels of these endogenous opiates, promoting some analgesic effect after the intervention.23
More recently, a review of electroacupuncture indicated this treatment seems to block pain by activating a variety of bioactive chemicals through peripheral, spinal, and supraspinal mechanisms. These include opioids, which desensitize peripheral nociceptors and reduce proinflammatory cytokines peripherally and in the spinal cord, and serotonin and norepinephrine, which decrease spinal N-methyl-D-aspartate receptor subunit GluN1 phosphorylation.24
In follow-up studies, it is observed that acupuncture therapy maintains a reduction in pain intensity for weeks or months after the intervention.10,11 In only one study, it was found that the group exposed to sham acupuncture (superficial acupuncture) had a statistically significant increase in the doses of carbamazepine for additional pain control.10
Carbamazepine is the gold standard medication but has substantial side effects: tiredness, nausea, dizziness, low concentration, somnolence, confusion and loss of appetite.1,4 Other complications may include agranulocytosis, aplastic anaemia and drug interactions through the induction of hepatic cytochrome P450.1 Transient leukopenia and thrombocytopenia may happen in 10% of patients.4
No study has reported side effects related to acupuncture, which can be a therapeutic advantage, especially in the elderly and people sensitive to medications.1
It is also important to note that half of the studies presented sham acupuncture (superficial acupuncture) as a control.10,17–19 It is known that this type of control generates bias, as the literature points that superficial needling, sham acupuncture point or simulation insertion of a needle without perforation of the skin can contribute to pain relief and therapeutic effect.25,26 These findings are supported by a recent systematic review, the authors found there is insufficient evidence to support or refute the use of acupuncture for neuropathic pain in general, or for any specific neuropathic pain condition when compared with sham acupuncture or other active therapies.27
All studies had a small sample size, which may compromise the interpretation of the results of the present study, but we might consider the low prevalence of TN. Concerning the most used instrument, the literature points out that the results obtained through the EVA are valid and reliable.28 Double blind controlled clinical trial articles can be questioned as to the methodology used, because the acupuncturist knows the therapy he is offering to the patient.1,4
In addition, it is known that the context of pain treatment alters the perception of pain. The relationship established between professional and patient as well as the frequent consultations carried out during the studies can generate a placebo effect. This is a result of the expectations and mental states from the patient's involvement in the treatment process.29
ConclusionAcupuncture therapy seems to decrease frequency or intensity of TN pain episodes, alone or in combination with gold standard medications. However, there is a need for standardizing methodological issues and prospective evaluations.
Declarations of interestNone.