The diagnosis process of soft tissue sarcomas of the musculoskeletal system (SPBAL) continues to be complex, with cases of unplanned excisions (“whoops” surgeries). This study evaluates the frequency of these type of procedures, trying to identify patient characteristics, tumours, surgical treatment and final results.
Material and methods131 patients treated surgically between October 2018 and December 2021 of a SPBAL were retrospectively reviewed. Patients with SPBAL located in the viscera, mediastinum, heart, retroperitoneum, peritoneum and genital tract were excluded. Differences between patients with planned and unplanned excisions were assessed with Chi2 tests and a Cox multivariate regression model.
ResultsUnplanned excisions of SPBAL have taken place in 18% of the patients in our area, mainly in tumours of less than 5cm and located superficial to the fascia. 29.2% of these patients did not have a previous imaging test. It has not been shown that a “whoops” surgery can lead to a decrease in survival or a higher rate of recurrences.
ConclusionsWe recommend carrying out an imaging test always prior to the removal of any type of soft tissue tumour, as well as adherence to the referral guidelines to reference centres.
El proceso diagnóstico de los sarcomas de partes blandas del aparato locomotor (SPBAL) sigue siendo comprometido, con casos de resecciones no planificadas (cirugías whoops). Este estudio evalúa la frecuencia de este tipo de procedimientos, tratando de identificar características de los pacientes, tumores, tratamiento quirúrgico y resultados.
Material y métodosSe revisan de forma retrospectiva 131 pacientes tratados de forma quirúrgica en nuestro centro entre octubre de 2018 y diciembre de 2021 de un SPBAL. Se excluyen los pacientes con SPBAL localizados en las vísceras, el mediastino, el corazón, el retroperitoneo, el peritoneo y el aparato genital. Las diferencias entre pacientes con resecciones planificadas y no planificadas fueron evaluadas con pruebas Chi cuadrado y un modelo de regresión multivariado de Cox.
ResultadosLas resecciones no planificadas de SPBAL han tenido lugar en un 18% de los pacientes de nuestra área, principalmente en tumores de menos de 5cm y localizados superficiales a la fascia. El 29,2% de estos pacientes no disponía de una prueba de imagen previa. No se ha demostrado que una cirugía whoops pueda suponer una disminución de la supervivencia o una mayor tasa de recidivas.
ConclusionesRecomendamos la realización de una prueba de imagen siempre previa a la extirpación de cualquier tipo de tumoración de tejidos blandos, así como la adherencia a las guías de remisión a centros de referencia.
Soft tissue sarcomas of the musculoskeletal system (SPBAL) are an extremely heterogeneous group of malignant tumours, accounting for less than 1% of malignant neoplasms in adults, with an incidence of two to three cases per 100,000 population in most European countries.1
We should bear in mind that benign soft tissue tumours are about 100 times more common than malignant tumours, the proportion being even higher in some locations such as the extremities.2 This discrepancy in presentation means that there is a high risk that a SPBAL can be mistaken for a benign tumour and resected without prior imaging study or biopsy. An excision with inadequate margins is known in the English-speaking literature as a “whoops procedure”, and usually requires a second, more aggressive intervention, sometimes necessitating amputation.3 These procedures have also been associated with an increase in local recurrences, especially in high-grade SPBAL.4
The present study aims to identify how many of the patients referred to our centre have undergone a “whoops procedure”, and identify risk factors related to the patient and the characteristics of the tumour and its treatment, comparing them with patients treated at our centre who had not undergone unplanned excision.
Material and methodsThe musculoskeletal tumour unit has been the region's referral centre for the treatment of sarcomas of the musculoskeletal system since October 2018, and provides care to a population of 2,100,000 inhabitants.
The selection criteria for inclusion in the study were patients of any age, diagnosed with any type of SPBAL (excluding Kaposi's sarcoma) between October 2018 and 31 December 2021, who underwent surgery as part of their primary treatment, and assessed in our centre's musculoskeletal tumour unit. Patients with SPBAL located in the viscera, and those located in the mediastinum, heart, retroperitoneum, peritoneum, and genital tract were excluded.
The patients included were recruited by review of their medical records, according to the citation register of our centre's sarcoma committee agendas. The research ethics committee approved the study. All patients had been assessed prior to the therapeutic decision in our hospital, by the multidisciplinary committee on bone and soft tissue sarcomas.
The primary endpoint of the study is a prior unplanned excision of a soft tissue tumour with a subsequent diagnosis of soft tissue sarcoma of the musculoskeletal system versus the total number of SPBALs in the same time period and population. Secondary variables were sex, age of the patient at diagnosis, location of the tumour (trunk/upper extremities/lower extremities), clinical size of the tumour measured on the basis of the largest diameter or by pathological anatomy or imaging test (less than or equal to 5cm, greater than 5cm or unknown), type of incision (longitudinal/transverse/oblique/S-shaped/unknown), depth (to the fascia: superficial/deep/unknown), availability of preoperative imaging test and tumour type, according to the World Health Organisation (WHO) classification.2 Local recurrence was also assessed by magnetic resonance imaging (MRI) and anatomopathological findings after the second excision or biopsy, the margins obtained (R0, R1, R2) in the second operation, as well as survival in months from diagnosis. All our patients underwent margin revision surgery, as well as radiotherapy and chemotherapy in those cases for whom, as recommended by the centre's musculoskeletal tumour committee, based on current scientific evidence. During excision surgery, the aim was to obtain a wide margin (2–3cm) of healthy tissue around the tumour, and the use of natural barriers as margins (fascia, perineurium, periosteum, adventitia). The surgeries were performed by a multidisciplinary team including orthopaedic surgeons, plastic surgeons, general surgeons, and vascular surgeons.
Categorical variables were assessed using the χ2 test. Trends by year for unplanned excision were analysed using the χ2 test applied to Pearson's correlation coefficient. Independent predictors for unplanned excisions were identified using a multivariable logistic regression model, selected based on a p-value<.05 in the univariable analysis. Survival was evaluated with Kaplan–Meier curves and the Cox regression method. The results of the logistic regression analyses are expressed as hazard ratios, with their 95% confidence intervals (95% CI). Results with a p-value<.05 are considered statistically significant. Analyses were performed using IBM SPSS v26 software (IBM Corp., Armonk, NY, USA).
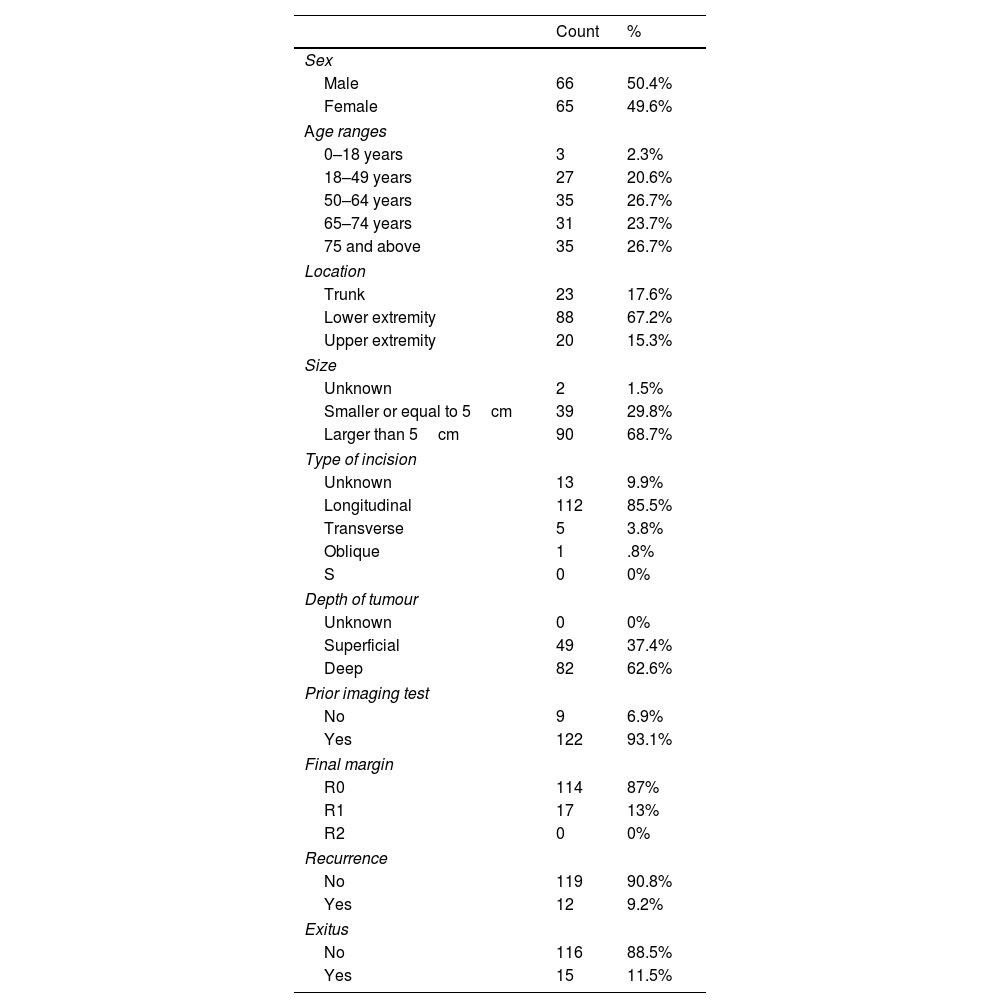
ResultsThe records of 131 patients were reviewed, of whom 24 (18.3%) had undergone an unplanned excision (Table 1). It was not necessary to exclude any patient because they failed to meet the inclusion criteria. The mean follow-up was 18 months, with a range between 1 and 41, and no patient was lost during this period. The gender distribution was very homogeneous, 66 males and 65 females. The most frequent age ranges were between 50 and 64 years and over 75 years, both at 26.7% of patients. The most common location (67.2%) was in the lower limbs. Most of the tumours recorded were larger than 5cm (68.7%), while the most common type of incision was longitudinal (85.5%). Most tumours were deep to the fascia (62.6%), and 122 of the 131 patients (93.1%) had an imaging test prior to surgery. Final margin and recurrence had similar frequencies (87 and 90.8%), and 15 of the patients died during follow-up (11.5%).
Absolute values and frequencies of the different variables.
| Count | % | |
|---|---|---|
| Sex | ||
| Male | 66 | 50.4% |
| Female | 65 | 49.6% |
| Age ranges | ||
| 0–18 years | 3 | 2.3% |
| 18–49 years | 27 | 20.6% |
| 50–64 years | 35 | 26.7% |
| 65–74 years | 31 | 23.7% |
| 75 and above | 35 | 26.7% |
| Location | ||
| Trunk | 23 | 17.6% |
| Lower extremity | 88 | 67.2% |
| Upper extremity | 20 | 15.3% |
| Size | ||
| Unknown | 2 | 1.5% |
| Smaller or equal to 5cm | 39 | 29.8% |
| Larger than 5cm | 90 | 68.7% |
| Type of incision | ||
| Unknown | 13 | 9.9% |
| Longitudinal | 112 | 85.5% |
| Transverse | 5 | 3.8% |
| Oblique | 1 | .8% |
| S | 0 | 0% |
| Depth of tumour | ||
| Unknown | 0 | 0% |
| Superficial | 49 | 37.4% |
| Deep | 82 | 62.6% |
| Prior imaging test | ||
| No | 9 | 6.9% |
| Yes | 122 | 93.1% |
| Final margin | ||
| R0 | 114 | 87% |
| R1 | 17 | 13% |
| R2 | 0 | 0% |
| Recurrence | ||
| No | 119 | 90.8% |
| Yes | 12 | 9.2% |
| Exitus | ||
| No | 116 | 88.5% |
| Yes | 15 | 11.5% |
The most frequently encountered tumour types (Table 2) were atypical lipomatous tumours (20.6%), followed by undifferentiated pleomorphic sarcomas (19.1%). After these were myxofibrosarcoma (10.7%) and pleomorphic liposarcoma (7.6%), and then a great heterogeneity of tumour types.
Tumour types according to WHO classification and their frequency.
| Whoops | Total | ||
|---|---|---|---|
| No | Yes | ||
| Tumour type | |||
| Pleomorphic LPS | |||
| Count | 9 | 1 | 10 |
| % of total | 6.9% | .8% | 7.6% |
| Undifferentiated LPS | |||
| Count | 4 | 0 | 4 |
| % of total | 3.1% | 0% | 3.1% |
| Synovial sarcoma | |||
| Count | 3 | 2 | 5 |
| % of total | 2.3% | 1.5% | 3.8% |
| Undifferentiated spindle cell sarcoma | |||
| Count | 2 | 1 | 3 |
| % of total | 1.5% | .8% | 2.3% |
| Malignant peripheral nerve sheath tumour | |||
| Count | 3 | 0 | 3 |
| % of total | 2.3% | 0% | 2.3% |
| Epithelioid sarcoma | |||
| Count | 3 | 1 | 4 |
| % of total | 2.3% | .8% | 3.1% |
| MFS | |||
| Count | 12 | 2 | 14 |
| % of total | 9.2% | 1.5% | 10.7% |
| UPS | |||
| Count | 18 | 7 | 25 |
| % of total | 13.7% | 5.3% | 19.1% |
| ALT | |||
| Count | 25 | 2 | 27 |
| % of total | 19.1% | 1.5% | 20.6% |
| Malignant schwannoma | |||
| Count | 0 | 1 | 1 |
| % of total | 0% | .8% | .8% |
| Leiomyosarcoma | |||
| Count | 1 | 3 | 4 |
| % of total | .8% | 2.3% | 3.1% |
| Myxoid LPS | |||
| Count | 9 | 0 | 9 |
| % of total | 6.9% | 0% | 6.9% |
| Dermatofibrosarcoma protuberans | |||
| Count | 7 | 1 | 8 |
| % of total | 5.3% | .8% | 6.1% |
| Solitary fibrous tumour | |||
| Count | 5 | 1 | 6 |
| % of total | 3.8% | .8% | 4.6% |
| Fibrosarcoma | |||
| Count | 0 | 1 | 1 |
| % of total | 0% | .8% | .8% |
| Pleomorphic rhabdomyosarcoma | |||
| Count | 1 | 0 | 1 |
| % of total | .8% | 0% | .8% |
| Alveolar sarcoma | |||
| Count | 1 | 0 | 1 |
| % of total | .8% | 0% | .8% |
| Round cell sarcoma | |||
| Count | 1 | 0 | 1 |
| % of total | .8% | 0% | .8% |
| Fibromyxoid sarcoma | |||
| Count | 1 | 0 | 1 |
| % of total | .8% | 0% | .8% |
| Small cell undifferentiated sarcoma | |||
| Count | 1 | 0 | 1 |
| % of total | .8% | 0% | .8% |
| Pleomorphic myxoid sarcoma | |||
| Count | 1 | 0 | 1 |
| % of total | .8% | 0% | .8% |
| Atypical spindle cell lipomatous tumour | |||
| Count | 0 | 1 | 1 |
| % of total | 0% | .8% | .8% |
| Total | |||
| Count | |||
| 107 | 24 | 131 | |
| % of total | |||
| 81.7% | 18.3% | 100% | |
ALT: atypical lipomatous tumour; LPS: liposarcoma; MFS: myxofibrosarcoma; UPS: undifferentiated pleomorphic sarcoma; WHO: World Health Organisation.
Of the 18.3% of patients who underwent unplanned excision, a statistical association p<.01 was found with different variables (Table 3). The size was smaller than or equal to 5cm in 54.3% of unplanned excisions compared to 24.3% of planned excisions. Tumour depth was 62.5% superficial in the whoops excisions, compared to 31% in the conventional excisions; 29.2% of the unplanned excisions had no previous imaging test, compared to 1.9% of the planned excisions. No statistical association was found with other variables, such as sex, age, location, final margin, recurrence rate, or exitus. There was also no preference for any tumour type with respect to the unplanned excisions.
Analysis of the different variables with respect to whether or not an unplanned resection (whoops procedure) was performed.
| Whoops | |||||
|---|---|---|---|---|---|
| No | Yes | ||||
| n | % | n | % | p | |
| Sex | |||||
| Male | 54 | 50.5% | 12 | 50% | .97 |
| Female | 53 | 49.5% | 12 | 50% | |
| Age ranges | |||||
| 0–18 years | 2 | 1.9% | 1 | 4.2% | .73 |
| 18–49 years | 24 | 22.4% | 3 | 12.5% | |
| 50–64 years | 28 | 26.2% | 7 | 29.2% | |
| 65–74 years | 26 | 24.3% | 5 | 20.8% | |
| 75 and above | 27 | 25.2% | 8 | 33.3% | |
| Location | |||||
| Trunk | 19 | 17.8% | 4 | 16.7% | .11 |
| Lower extremity | 75 | 70.1% | 13 | 54.2% | |
| Upper extremity | 13 | 12.1% | 7 | 29.2% | |
| Size | |||||
| Unknown | 0 | 0% | 2 | 8.3% | <.01 |
| Small or equal to 5cm | 26 | 24.3% | 13 | 54.2% | |
| Larger than 5cm | 81 | 75.7% | 9 | 37.5% | |
| Type of incision | |||||
| Unknown | 5 | 4.7% | 8 | 33.3% | <.01 |
| Longitudinal | 101 | 94.4% | 11 | 45.8% | |
| Transverse | 1 | .9% | 4 | 16.7% | |
| Oblique | 0 | 0% | 1 | 4.2% | |
| S | 0 | 0% | 0 | 0% | |
| Depth of tumour | |||||
| Unknown | 0 | 0% | 0 | 0% | <.01 |
| Superficial | 34 | 31.8% | 15 | 62.5% | |
| Deep | 73 | 68.2% | 9 | 37.5% | |
| Prior imaging test | |||||
| No | 2 | 1.9% | 7 | 29.2% | <.01 |
| Yes | 105 | 98.1% | 17 | 70.8% | |
| Final margin | |||||
| R0 | 94 | 87.9% | 20 | 83.3% | .55 |
| R1 | 13 | 12.1% | 4 | 16.7% | |
| R2 | 0 | 0% | 0 | 0% | |
| Recurrence | |||||
| No | 99 | 92.5% | 20 | 83.3% | .16 |
| Yes | 8 | 7.5% | 4 | 16.7% | |
| Exitus | |||||
| No | 96 | 89.7% | 20 | 83.3% | .38 |
| Yes | 11 | 10.3% | 4 | 16.7% | |
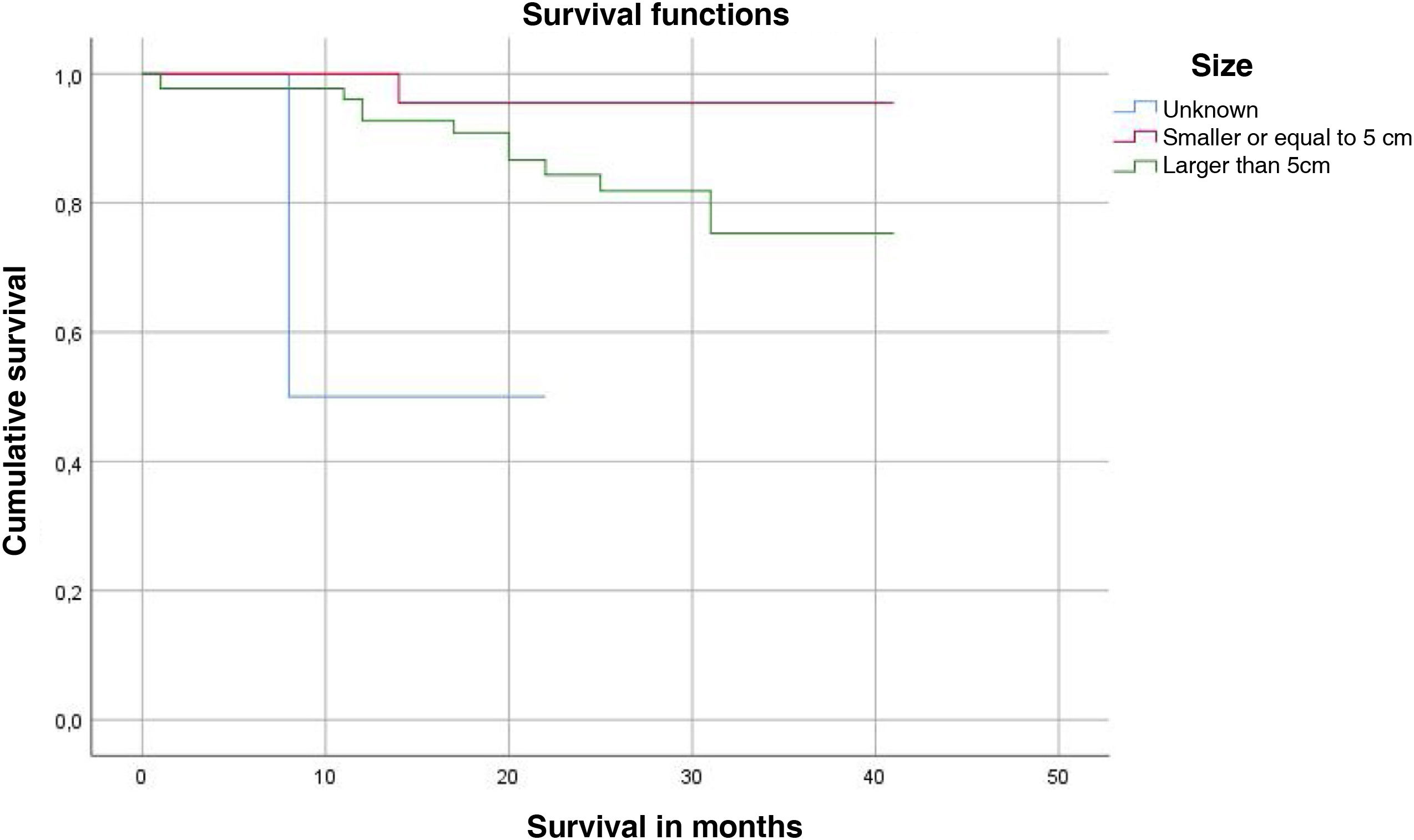
Having undergone a whoops procedure did not affect overall survival, nor did local recurrence, but a tumour size of less than 5cm implied better survival (log-rank p<.05) (Fig. 1). A statistically significant association (p<.05) was also found between tumour size larger than 5cm and the risk of local recurrence.
With respect to multivariate analysis, statistical significance (p<.001) was only found in the absence of a prior imaging test (HR 11.44, 95% CI 4.38–29.88).
DiscussionUnplanned excisions of SPBALs are a classic problem in the literature. The rate of these surgeries seems to coincide with other similar modern studies,1,4 levels that have been progressively decreasing with respect to more distant investigations.1 There are several reasons attributed to these changes. Firstly, large population-based studies1 link them to the diagnostic progress of expert multidisciplinary teams, resulting in very few unplanned excisions performed in-house, while most come from external centres. Secondly, the creation and dissemination of referral guidelines based on simple and easy-to-use criteria also seem to play a major role in reducing the number of cases.
Undoubtedly, despite measures to centralise the treatment of SPBALs in specialised centres,5 unplanned surgeries will continue to take place. Soft tissue tumours are overwhelmingly benign, and it is almost inevitable that small, superficial lesions, with no other clinical signs to indicate SPBAL, will be excised without oncological margins, eventually manifesting as malignant neoplasms. On the other hand, large tumours are often referred to expert centres and unplanned excisions are largely avoided.6
Our study reminds us that there are still important steps to be taken in medical education. A large proportion of the whoops procedures referred to our centre had not been preceded by an imaging test.
Fortunately, unplanned excisions do not seem to imply an unfavourable prognosis, unlike that indicated by the more classic publications.7 Since the article by Giuliano et al.,8 margin revision surgery has become the standard treatment for high-grade tumours, and has even been associated with improved survival,6 which we were not able to demonstrate in our review. It is not clear, however, that this increase in survival is associated with better function,3 even in combination with radiotherapy,9 there might even be greater morbidity, although no significant differences have been found between the two groups in the studies published on this subject.10 In contrast, there is no consensus on what to do in cases where the tumour is small and low grade. The tendency not to perform margin revision, or at least to delay it, seems to increase the risk for local recurrence, which does not seem to affect patient survival.11,12 In fact, Lewis et al.6 indicate in their study that the presence of residual tumour in second surgeries has not been associated with a worse prognosis.13 Therefore, the association between local recurrence and patient survival remains unclear in patients with sarcomas of the musculoskeletal system,14 in contrast to patients with retroperitoneal sarcoma,15 in whom recurrence can lead to death.
Our review also has limitations. It is a retrospective study, with patients selected as our centre was being developed as a referral centre for the autonomous community, not a population-based study, in the context of a transition period in which it is quite possible that patients were treated in their hospitals of origin without being referred to our centre. All our patients underwent margin revision surgery, without it being possible to compare results with adjuvant treatment or expectant management. It should also be noted that the follow-up time was not long, and that due to the rarity of SPBAL the number of patients evaluated was small.
ConclusionsA total 18% of patients in our area underwent an unplanned excision of SPBAL, mainly in tumours smaller than 5cm and located superficial to the fascia; 70% of these patients did not have a prior imaging test. Whoops surgery leading to decreased survival, or a higher recurrence rate was not demonstrated. We recommend that an imaging test should always be performed prior to excision of any type of soft tissue tumour, and the referral guidelines should be adhered to.
Level of evidenceLevel of evidence iv.
FundingNo funding was received for this work.
Conflict of interestsThe authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.