Subtalar dislocations are a rare entity (<1%) in traumatic foot injuries. There is a loss of anatomical relationship between the talus, calcaneus and scaphoid. There are only small-published series.
Material and methodsWe present a series of patients (N=13) with subtalar dislocations in which a descriptive analysis of the main epidemiological, clinical and radiological variables was carried out, from which an urgent treatment algorithm is proposed. Cases with fractures of the neck of the talus, body of the calcaneus, or isolated Chopart fracture-dislocations were excluded.
ResultsThe median age was 48.5 years with a predominance of males (69.23%). Five patients suffered falls or sprained ankles and the other eight suffered high-energy mechanisms. The medial dislocations (nine) predominated over the lateral ones (four). In addition, four patients presented open dislocations, two of them type IIIC that required amputation. CT scans were requested in 76.93% of patients and 10 presented associated bone lesions of the foot. Open reduction surgery was performed in all open lesions and in one case in which closed reduction failed. Five patients required a delta-type external fixator. Subchondral articular sclerosis was observed in 77.77% of cases; although only one required subtalar arthrodesis.
ConclusionsSubtalar dislocations are a traumatic emergency that require early reduction and subsequent immobilisation. Transarticular temporary external fixation is a good immobilisation option in open dislocations. They are serious lesions with a high probability of early osteoarthritis.
Las luxaciones periastragalinas son una entidad poco frecuente (<1%) de las lesiones traumáticas del pie. Se produce una pérdida de relación anatómica entre astrágalo, calcáneo y escafoides. Solo hay pequeñas series publicadas.
Material y métodosPresentamos los casos de una serie de pacientes (n=13) con luxaciones periastragalinas en los que se realizó un análisis descriptivo de las principales variables epidemiológicas, clínicas y radiológicas, a partir de las cuales se propone un algoritmo de tratamiento urgente. Se excluyeron los casos con fracturas del cuello del astrágalo, del cuerpo del calcáneo o fracturas-luxación de Chopart aisladas.
ResultadosLa mediana de edad fue de 48,5 años, con predominio del sexo masculino (69,23%). Cinco pacientes sufrieron caídas-entorsis sobre el tobillo y los 8 restantes, mecanismos de alta energía. Las luxaciones mediales (9) predominaron sobre las laterales (4). Además, 4 pacientes presentaron luxaciones abiertas, 2 de ellas tipo IIIC, que precisaron amputación. Se solicitó TC en el 76,93% de los pacientes, y 10 presentaron lesiones óseas asociadas del pie. Se realizó cirugía mediante reducción abierta en todas las lesiones abiertas y en un caso en el que fracasó la reducción cerrada. Cinco pacientes precisaron fijador externo tipo delta. Se objetivó esclerosis subcondral articular en el 77,77% de los casos, si bien solo uno precisó artrodesis subtalar.
ConclusionesLas luxaciones periastragalinas son una urgencia traumatológica y precisan una reducción precoz e inmovilización posterior. La fijación externa temporal transarticular es una buena opción de inmovilización en luxaciones abiertas. Son lesiones graves con alta probabilidad de artrosis precoz.
Astragalo-scapofocalcaneal, subtalar, or peri-talar dislocations are a rare condition (<1%) among traumatic injuries of the foot.1 A loss of the anatomical relationship between the talocalcaneal and taloscaphoid joints while maintaining the congruence of the tibiotalar joint occurs as a result of high-energy accidents (falls from heights, traffic accidents, and athletic activities).2 Seventy-five percent are medial dislocations associated with high-energy mechanisms and associated injuries such as fractures of the malleoli, scaphoid, or fifth metatarsal.3 They are a traumatic emergency and require early diagnosis, either closed or open reduction, and subsequent immobilisation.4
This is not an injury that orthopaedic surgeons encounter on a regular basis, but due to its potential complications, especially if an incorrect diagnosis and/or treatment is carried out, being knowledgeable about how to urgently manage these injuries is important. Only clinical cases or small case series (10–25 patients) have been published in the international literature.5–7 The aim is to provide a descriptive analysis of the main epidemiological, clinical, and radiological variables in order to propose an emergency treatment algorithm.
Material and methodsThis is a descriptive observational study of a series of patients (N=13) with subtler dislocations. The inclusion criteria for inclusion were all those subjects with subtalar dislocations who were seen in our hospital between 2016 and 2021. All patients were initially seen in the emergency department by orthopaedic and trauma surgeons, taking the corresponding anamnesis and carrying out the corresponding physical examination. Special attention was paid to the description of the initial deformity and to rule out possible neurovascular involvement. All participants underwent anteroposterior and oblique radiographs of the foot, as well as anteroposterior and lateral radiographs of the ankle. Computed tomography (CT) was requested in those cases in which the clinical situation did not initially preclude it. Advanced imaging scans, such as magnetic resonance imaging (MRI), were not performed as per protocol.
Patients with subtalar dislocations sustained in a high-energy accident and other associated injuries were managed by the team of intensive care specialists in accordance with the Advanced Trauma Life Support (ATLS) protocol. Individuals were excluded if they had fractures of the neck of the talus, body of the calcaneus, or isolated Chopart fracture-dislocations, if they were minor, or if they had not received a correct follow-up. Authorisation was requested of and granted by the Clinical Research Ethics Committee (CREC).
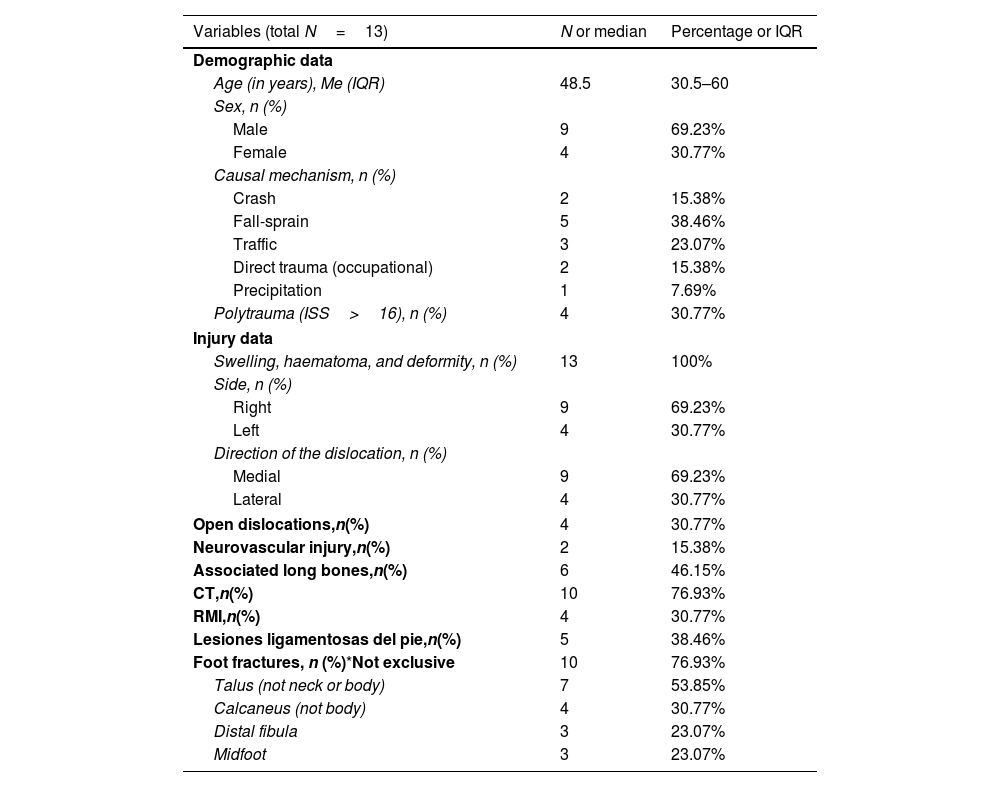
The epidemiological, clinical, radiological, perioperative, and follow-up variables were collected for each patient, as detailed in Tables 1–3; the following are of note given their relevance: sex, age, mechanism of injury, subtype of dislocation, open fracture and/or neurovascular injury, associated fractures of the foot, imaging tests, type of emergency treatment, immobilisation time, total follow-up, and complications or re-interventions.
Demographic, clinical data, and injury pattern of the patients included in the study.
| Variables (total N=13) | N or median | Percentage or IQR |
|---|---|---|
| Demographic data | ||
| Age (in years), Me (IQR) | 48.5 | 30.5–60 |
| Sex, n (%) | ||
| Male | 9 | 69.23% |
| Female | 4 | 30.77% |
| Causal mechanism, n (%) | ||
| Crash | 2 | 15.38% |
| Fall-sprain | 5 | 38.46% |
| Traffic | 3 | 23.07% |
| Direct trauma (occupational) | 2 | 15.38% |
| Precipitation | 1 | 7.69% |
| Polytrauma (ISS>16), n (%) | 4 | 30.77% |
| Injury data | ||
| Swelling, haematoma, and deformity, n (%) | 13 | 100% |
| Side, n (%) | ||
| Right | 9 | 69.23% |
| Left | 4 | 30.77% |
| Direction of the dislocation, n (%) | ||
| Medial | 9 | 69.23% |
| Lateral | 4 | 30.77% |
| Open dislocations,n(%) | 4 | 30.77% |
| Neurovascular injury,n(%) | 2 | 15.38% |
| Associated long bones,n(%) | 6 | 46.15% |
| CT,n(%) | 10 | 76.93% |
| RMI,n(%) | 4 | 30.77% |
| Lesiones ligamentosas del pie,n(%) | 5 | 38.46% |
| Foot fractures, n (%)*Not exclusive | 10 | 76.93% |
| Talus (not neck or body) | 7 | 53.85% |
| Calcaneus (not body) | 4 | 30.77% |
| Distal fibula | 3 | 23.07% |
| Midfoot | 3 | 23.07% |
ISS: Injury Severity Score; Me: median; IQR: interquartile range; MRI: magnetic resonance imaging; CT: computed tomography.
Data are expressed as n (%) or median (interquartile range).
Perioperative data of the patients included in the study.
| Variables (total N=13) | N or median | Percentage or IQR |
|---|---|---|
| Time to reduction in hours, Me (IQR) | 4 | 3–5 |
| Place of reduction and anaesthesia, n (%) | ||
| Emergency room (intra-articular anaesthesia) | 3 | 23.07% |
| Operating theatre | 10 | 76.93% |
| General anaesthesia | 7 | 53.85% |
| Spinal anaesthesia | 3 | 23.07% |
| Prior attempt at closed reduction, n (%) | 3 | 23.07% |
| Type of treatment, n (%) | ||
| Conservative (splint or walker) | 7 | 53.84% |
| Surgical, *Not exclusive | 6 | 46.15% |
| Open reduction+EF | 3 | 23.07% |
| Open reduction+IF | 1 | 7.69% |
| Open reduction+IF+EF | 1 | 7.69% |
| Closed reduction+EF | 1 | 7.69% |
EF: external fixation; IF: internal fixation; Me: median; IQR: interquartile range.
Data are expressed as n (%) or median (interquartile range).
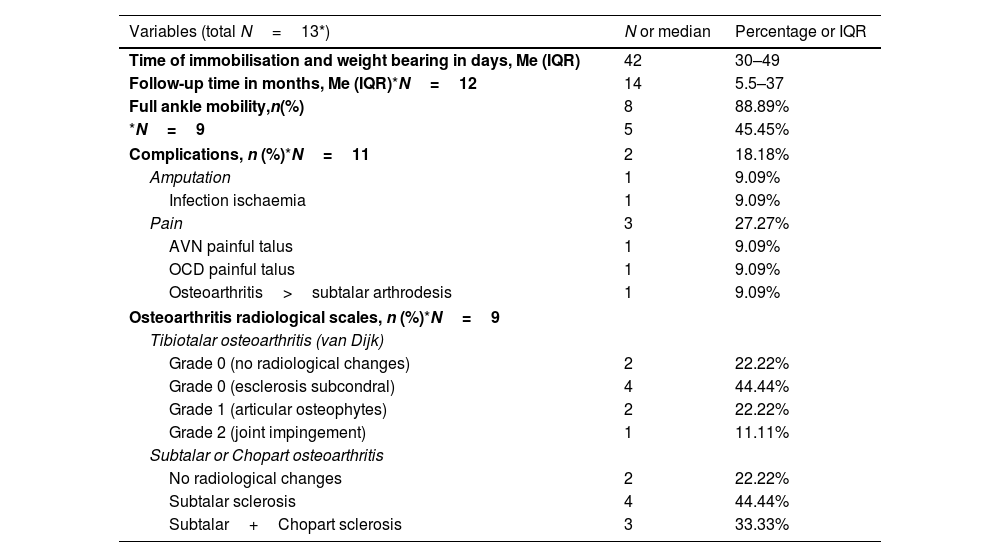
Clinical and radiological data available at last follow-up and complications of the patients included in the study.
| Variables (total N=13*) | N or median | Percentage or IQR |
|---|---|---|
| Time of immobilisation and weight bearing in days, Me (IQR) | 42 | 30–49 |
| Follow-up time in months, Me (IQR)*N=12 | 14 | 5.5–37 |
| Full ankle mobility,n(%) | 8 | 88.89% |
| *N=9 | 5 | 45.45% |
| Complications, n (%)*N=11 | 2 | 18.18% |
| Amputation | 1 | 9.09% |
| Infection ischaemia | 1 | 9.09% |
| Pain | 3 | 27.27% |
| AVN painful talus | 1 | 9.09% |
| OCD painful talus | 1 | 9.09% |
| Osteoarthritis>subtalar arthrodesis | 1 | 9.09% |
| Osteoarthritis radiological scales, n (%)*N=9 | ||
| Tibiotalar osteoarthritis (van Dijk) | ||
| Grade 0 (no radiological changes) | 2 | 22.22% |
| Grade 0 (esclerosis subcondral) | 4 | 44.44% |
| Grade 1 (articular osteophytes) | 2 | 22.22% |
| Grade 2 (joint impingement) | 1 | 11.11% |
| Subtalar or Chopart osteoarthritis | ||
| No radiological changes | 2 | 22.22% |
| Subtalar sclerosis | 4 | 44.44% |
| Subtalar+Chopart sclerosis | 3 | 33.33% |
Me: median; AVN: avascular necrosis; OCD: osteochondritis dissecans; IQR: interquartile range.
Data are expressed as n (%) or median (interquartile range).
The Van Dijk radiological scale8 was used to assess tibiotalar joint arthropathy. To this end, two authors conducted a systematic review of the most recent radiographs available at follow-up. They also looked for signs of radiological osteoarthritis in the subtalocalcaneal or talocalcaneal and astragalo-scaphoid or talonavicular joints.
Surgery and in-office follow-up were performed by trauma surgeons or orthopaedic surgeons with expertise in foot and ankle surgery. Only one attempt at closed reduction was permissible in the emergency under intra-articular anaesthesia with the twofold aim of reducing the dislocation in the shortest time possible without causing further damage by repeated unsuccessful reductions. Nevertheless, the presence of open dislocation or neurovascular complication was an absolute indication for open reduction in the operating theatre under anaesthesia. Following initial reduction, with or without surgical treatment, a period of immobilisation (splint, Walker, or external fixator) and relieving the limb of weight-bearing for 4–6 weeks until progressive ambulation was authorised. All the participants attended follow-up check-ups at the 1st, 2nd, 3rd, 6th, and 12th months. In two cases for whom no recent information was available due to loss of follow-up appointments, a search for information was undertaken using the HORUS computer platform of the Madrid Healthcare Service.
A descriptive analysis of the variables recorded in the study was performed. Categorical variables are expressed as absolute (n) and relative (%) frequencies. Continuous quantitative variables are expressed as median and interquartile range (IQR), assuming an abnormal distribution according to the Kolmogorov–Smirnov test given the small sample size. As this was a case series of a rare injury in traumatology, no sample size calculation was performed, but all available patients were recruited. Again, because of the small sample size, inferential analysis was not possible.
ResultsThe median age of the study sample was 48.5 years and was predominantly male (69.23%), as indicated in Table 1, which reflects the epidemiological and clinical data and the injury pattern. In terms of the causal mechanism of injury, five patients suffered falls-enthesis in the ankle and the remaining eight were high-energy mechanisms (five traffic accidents, two feet trauma-crushes, and one fall). Of these, four subjects were classified as polytrauma cases, defined as damage to more than two organs with at least one life-threatening injury and/or an Injury Severity Score (ISS) greater than 16. The patients had no known relevant personal history or cardiovascular risk factors, except for depression in the one case of autolytic fall.
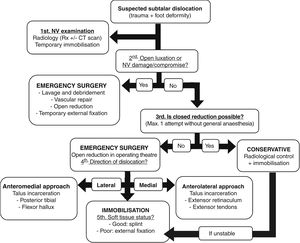
Swelling, haematoma, and deformity were a consistent feature of the physical examination of the patients (100%), with all open dislocations being associated with injury (4). According to the Gustilo and Anderson classification, we had two type IIIA and two type IIIC open dislocations, requiring the involvement of the plastic and/or vascular surgery teams. The two-type IIIC open dislocations correspond to the two cases listed in Table 1 with neurovascular injury (section of the anterior tibial bundle and section of the posterior tibial bundle). In terms of the subtype of periastragaline dislocations according to the direction of clinically and radiologically observed dislocation (Fig. 1), there was a predominance of medial dislocations (9) over lateral dislocations (4).
32-Year-old man with pain and deformity in the right foot after forced inversion. The protrusion of the lateral aspect of the talus into the skin can be seen (A). The anteroposterior radiograph shows loss of subtalar congruence, with the calcaneus in a medial position to the talus (B). Lateral radiograph shows loss of congruity at Chopart's joint (C).
CT scans were ordered in 76.93% of the cases and 10 patients had associated bone injuries of the foot, with fractures of the posteromedial (3), lateral (3), or anteromedial dome (1) of the talus being the most common; fractures of the anterior tuberosity (1), posterior tuberosity (1), or sustentaculum tali (2) of the calcaneus; fractures of the fibula (3) of the supra (1), trans (1) and infrasyndesmal (1) types, and, finally, the three fractures sustained by the midfoot (two fractures of the base of the 5th metatarsal, as well as one fracture of the lateral wedge) of the calcaneus (2). Only four patients underwent MRI; however, ligament injuries were diagnosed in 38.46% of the study population (100% in the case of those who had an MRI), most notably ruptures of the anterior capsule, the lateral ankle complex, and deltoid ligament, the astragalo-scapholunate ligament, and the interosseous ligament.
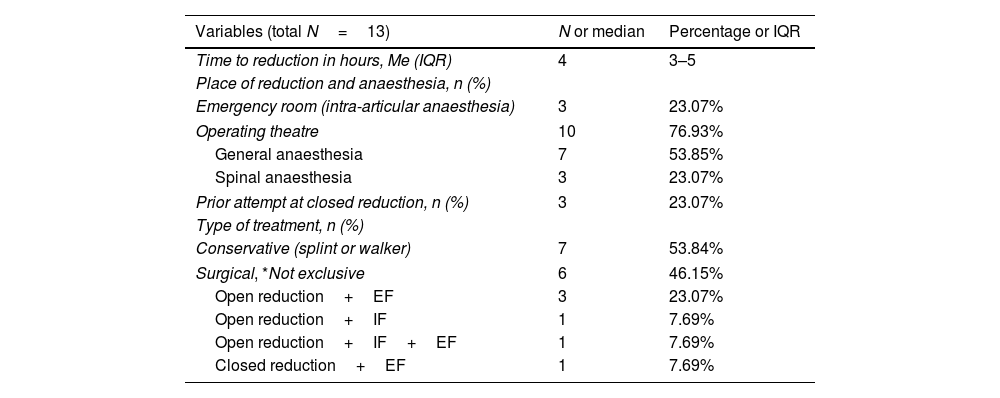
Median peritalar dislocation reduction was performed at 4h (3–5h of IQR) from the initial trauma, under general (7) or spinal (3) anaesthesia when carried out in the operating theatre (76.93%) or under intra-articular anaesthesia if reduction was achieved in the emergency department (23.07%). Surgery was required in six cases (46.15%) for different reasons (Table 2). On the one hand, four open dislocations required lavage, debridement, joint dislocation reduction, primary wound closure, and internal or external fixation. Conversely, of the two closed dislocations with unsuccessful attempts at closed reduction in the emergency department, one required, open reduction (Fig. 2) and, the other, closed reduction; in both cases in association with an external fixation (EF) device.
43-Year-old man with pain and deformity in his right foot after a traffic accident. A medial skin fold-groove suggestive of incarceration of tendon structures is seen in the context of a lateral subtalar dislocation (A). The anteroposterior radiograph shows a loss of subtalar congruity (B). An open reduction through a medial approach was required due to the incarceration of the posterior tibial tendon around the neck of the talus. After the reduction, an external fixator was implanted to control the stability and evolution of the soft tissues (C).
Of these six patients who needed some form of surgical fixation, the majority option in 5/6 cases was a delta-mounted external fixator. Internal fixation (IF) or percutaneous fixation was used in 2/6 cases: one patient needed K-wires in the astragalo-scaphoid joint and a transindesmal screw, in addition to EF; in the other patient, internal fixation was performed exclusively with a Steinmann pin in the subtalar joint and three k-wires (two in the talonavicular joint and one in the calcaneocuboid joint). As for the remaining seven cases (53.84%), closed reduction was undertaken in the ED or operating theatre with immobilisation with Walker or suropedic splinting (Table 2).
The median immobilisation time until full weight bearing was 42 days (30–49 days IQR), as indicated in Table 3. With a median follow-up of 14 months (5.5–37 months IQR), the nine patients in whom ankle mobility could be assessed (excluding two cases because of loss of data and another two in whom it was not applicable due to amputation) achieved functional joint range and ambulation after the 3rd month, except for one case with a dorsal flexion deficit of 10° and subtalar stiffness.
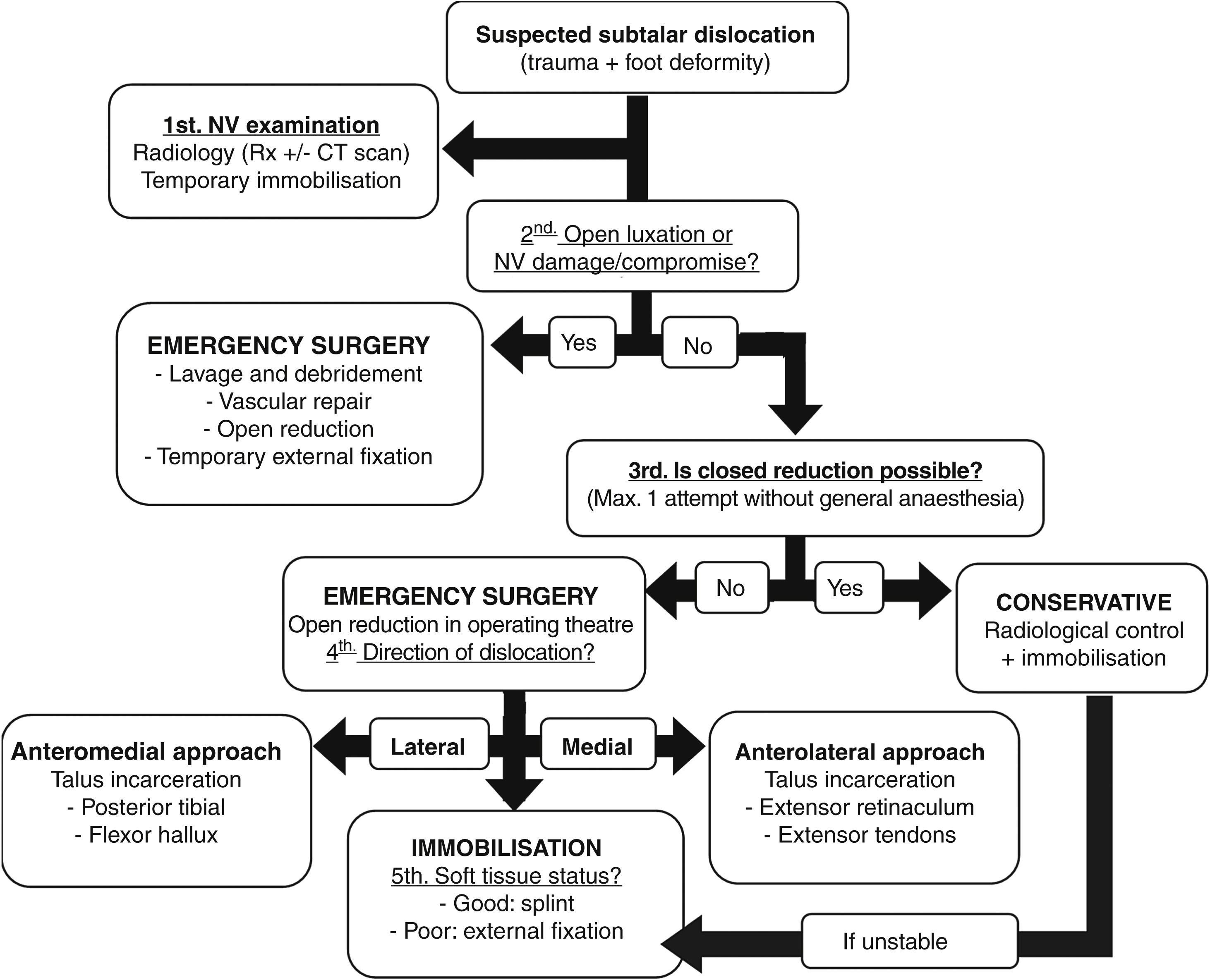
There was a high percentage of complications in five of the eleven patients (45.45%) who were followed up. The two cases with neurovascular injury (IIIC) required reintervention and infratuberosity amputations of the tibia; in one patient, for infection after fasciotomies performed for compartment syndrome and, in the other case, for ischaemia after failure of saphenous revascularisation. In the other three cases with persistent pain, avascular necrosis (AVN) of the talus, osteochondritis dissecans (OCD) of the talus, and subtalar osteoarthritis with significant pain and functional limitation requiring subtalar arthrodesis with cannulated screws were diagnosed. Regarding the radiological scales, subchondral tibiotalar, subtalar, or Chopart subchondral sclerosis was observed in 77.77% of the cases, although only one required subtalar arthrodesis. Based on all these data and the literature, we proposed an algorithm for urgent treatment of peritalar dislocations (Fig. 3).
DiscussionPeritalar dislocations typically occur in young males in the context of high-energy accidents.6 In this regard, the main differences between our series and the data reported in the literature are a slightly higher median age and a lower rate of high-energy accidents, with a group of five older patients with low-energy falls and sprains.2 A complete neurovascular examination is mandatory, as neurovascular lesions have been reported in up to 70% of lateral peritalar dislocations.3 In our series, the anterior tibial artery was severed in a medial peritalar dislocation, while the posterior tibial artery section occurred in a lateral dislocation.
Malgaigne et al. described sub-variants based on the position of the calcaneus relative to the talus.9 The mechanism of injury is caused by indirect forces resulting in reproducible ligamentous and capsular damage.2 Supination or forced inversion of the forefoot with the rearfoot in plantar flexion results in medial dislocation,7 the most commonly observed pattern in our series (69.23%) in line with the rest of the literature, with figures close to 70–80%10,11 because this joint is more unstable in inversion, while pronation or eversion with dorsal flexion results in lateral dislocation.3,4
Despite the fact that anteroposterior and lateral radiography is a standard technique to diagnose this condition and associated injuries, CT scans are highly recommended for a full study of the injury, either pre- or post-reduction. These dislocations rarely arise in isolation; 20–60% are associated with fractures of the talus or calcaneus, malleolar or metatarsal fractures, and osteochondral fractures that are not visible on X-ray.12 Some 76.93% of patients in our study underwent CT imaging, most of them following reduction so as to prevent treatment delay. Only two patients with CT were found to have no associated fractures. Pure dislocation without associated fractures is rare, but evolves with minimal or no sequelae if properly treated.13 Nonetheless, few patients (30.77%) underwent MRI, which would account for ligamentous injuries being underdiagnosed, particularly as they are highly prevalent in this type of peritalar dislocation.2 That being said, the MRI findings did not change the treatment plan proposed, which is why it is not initially protocolised.
Closed reduction in the operating theatre under general anaesthesia or spinal anaesthesia is routinely recommended using on-axis traction with the knee flexed at 90° (Bohler manoeuvre), which allows the aquileocalcaneal system to relax.14 The first step is to increase the ankle deformity in order to relieve the subtalar joint and then the dislocation is reduced by applying force in the opposite direction to the trauma, under intraoperative fluoroscopic control.6 In our study, 76.93% of the reductions were carried out under general anaesthesia or spinal anaesthesia in the operating theatre. However, closed reduction of these dislocations as early as possible is the key to improving the prognosis of the injury. Forced reductions or multiple attempts should be avoided as they may result in injury to the skin and damage to neurovascular structures.15 Early reduction of dislocations was achieved in our patient cohort, which is an aspect that is not well covered in many articles.
If closed reduction cannot be achieved (10–30%), open reduction should be undertaken in the operating theatre using an anterior longitudinal approach in medial dislocations and between the head of the talus and the medial malleolus in lateral dislocations.7 Two cases of unsuccessful attempts at closed reduction were reported, one of which was a lateral peritalar dislocation that required open reduction because of the interposition of the posterior tibial tendon anterior to the neck of the talus, the same situation documented in another patient with a lateral open dislocation. Interposition of tendinous elements is documented in the literature as a cause of failed reduction: in medial dislocations, due to incarceration of the head of the talus in the extensor tendons of the toes, and in lateral dislocations, because of the interposition of the posterior tibial or hallux flexor tendon in the neck of the talus.16
Together with the impossibility of closed reduction, other indications for urgent surgery are open dislocation or associated neurovascular injury, as was the case in the four participants (30.77%) in our series with open dislocations (including the two-type IIIC dislocations). Up to 40% of cases are open dislocations, requiring initial lavage and debridement followed by reduction and subsequent wound closure if possible.2 If there is instability after reduction or close follow-up and wound care is required, a temporary transarticular EF should be used.16 Our four patients with open dislocations and one with instability post-reduction were treated with a delta-mounted external fixator (38.46%). There is no evidence concerning the best rehabilitation protocol, although four weeks of immobilisation is routinely recommended if it is a pure dislocation and 6–8 weeks if there are associated tarsal fractures17; although virtually no cases of residual instability have been reported.14
Short-term complications include infection, skin necrosis, or vascular lesions, and late complications consist of AVN of the talus, early osteoarthritis, and chronic pain.2 In any case, the data available in the published literature vary as to what is or is not considered a major complication, making it difficult to compare results. Our complication rate of 45.45% is within the range reported in most scientific articles, including an amputation rate of over 20% for severe neurovascular injuries. Only one patient with AVN of the talus was observed (9.09%), which is in line with the range of 5–29% depending on whether the dorsal pedicle artery remains intact or not.18
In 50–80% of subtalar dislocations, there will be long-term radiographic osteoarthritis and up to 80% decreased subtalar mobility with difficulty in adapting to unstable ground due to peritalar fibrosis. We observed tibiotalar, subtalar, or talonavicular subchondral sclerosis in 77.77% of our series of cases, although only one necessitated subtalar arthrodesis because of pain. This clinical–radiological discordance is well known and may explain why, in our case, these high figures of radiological osteoarthritis do not translate into a higher rate of subtalar or ankle arthrodesis.11,19 Although it should be remembered that the follow-up time in our series is short-intermediate term and longer period of evolution may be required.
Concerning the limitations of this study, it must be said that this is a retrospective observational study, with the biases inherent to this type of design. The collection of EHR variables could mean that some of them might not have been properly recorded or might have been reported in an incomplete and more subjective way, without the availability of functional scales. As previously remarked, other limitations are the small sample size and the short follow-up time, which is necessary to identify complications and long-term outcomes correctly. Nonetheless, it is a sufficiently important grouping of cases in a short time frame (5 years), given the rarity of the injury, for these results to be reported to the scientific community and for an urgent treatment proposal to be put forward.
ConclusionsPeritalar dislocations are a trauma emergency and require prompt reduction and subsequent immobilisation. Temporary transarticular EF is a good option to immobilise open dislocations for wound care. These are severe injuries with a high probability of early osteoarthritis despite the clinical–radiological mismatch observed.
Level of evidenceLevel of evidence iv.
FundingThis research has not received any funding from the public, comercial, or non-profit sectors.
Conflict of interestsThe authors have no conflict of interests to declare.