To study and evaluate the unusual findings in the natural history of parosteal osteosarcomas. Parosteal osteosarcomas are well-differentiated tumours of low grade malignancy, but may dedifferentiate into a more aggressive lesion.
Material and methodsWe reviewed 7 parosteal osteosarcomas treated in La Paz Hospital between 2005 and 2009 (3 were dedifferentiated parosteal osteosarcomas (ddPO)). The authors analysed the clinical and radiological features, histology, treatment and outcomes in this patient group.
ResultsThere were 5 men and 2 women, with a mean age of 32.14 years, range 24–47 years. Three of seven tumours (42.8%) were dedifferentiated osteosarcomas. All three patients received chemotherapy. One patient presented with pulmonary metastases. No patient died.
ConclusionsIt is important to understand that the biological phenomenon of dedifferentiation can occur in parosteal osteosarcomas. The prognosis, treatment and survival changes radically.
Estudiar y evaluar los hallazgos poco frecuentes en la historia natural de los osteosarcomas parostales. Los osteosarcomas parostales son tumores bien diferenciados de bajo grado de malignidad. La desdiferenciación en una lesión más agresiva.
Material y métodoSe revisaron una serie de 7 osteosarcomas parostales tratados en el Hospital la Paz entre 2005 y 2009 (tres fueron osteosarcoma parostales desdiferenciados). Los autores analizaron las características clínicas y radiológicas, la histología, tratamiento y resultados en este grupo de pacientes.
ResultadosLa distribución por sexos fueron: 5 varones y dos mujeres. La edad media de los pacientes fue: 32,14 años; rango: 24-47 años. Tres tumores de 7 (42,8%) fueron osteosarcomas desdiferenciados. Los tres pacientes recibieron quimioterapia. Un paciente debutó con metástasis pulmonares. Ningún paciente falleció.
ConclusionesEs importante la comprensión que el fenómeno biológico de la desdiferenciación puede ocurrir en los osteosarcomas parostales. El pronóstico, tratamiento y supervivencia cambia radicalmente.
Osteosarcomas are malignant primary tumours in which the neoplastic cells give rise to an osteoid matrix. Many osteosarcomas become settled in an intramedullary location, but there are other, extramedullary varieties, known as superficial osteosarcomas.1 Superficial osteosarcomas may be classified into 3 types: parosteal, periosteal and high-grade osteosarcomas. Parosteal osteosarcomas are the most common and least aggressive of superficial osteosarcomas. Dedifferentiated parosteal osteosarcomas (ddPO) represent a fourth variant of superficial osteosarcoma, in which a high-grade osteosarcoma (Broders grade 3–4) coexists with a conventional parosteal osteosarcoma (Broders grade 1–2), either at the time of presentation (synchronous type) or at the time of recurrence (metachronous type).2 The aim of this study was to evaluate findings differing from the typical natural history of parosteal osteosarcomas.
Material and methodWe conducted a retrospective review of 7 consecutive parosteal osteosarcomas treated at Hospital Universitario La Paz, in Madrid, between January 2005 and December 2009. Clinical information was obtained from medical records. The radiographic findings included location within the bone, location, presence and characteristics of the tumoural area and medullary invasion. The pathological samples were analysed in order to confirm the diagnosis and identify the dedifferentiated component. Only the areas of histological tumour with Broders grade 3 or 4 were considered dedifferentiated. All patients underwent imaging studies and percutaneous biopsy with a trocar (osteobone®).
ResultsClinical characteristicsThe series was composed of 5 males and 2 females. Patients were aged between 24 and 47 years (mean: 32.14 years). All tumours were located in long bones. The most common site of primary tumour was the proximal femur with 4 cases, followed by the humeral diaphysis with 1 case, the proximal humerus with 1 case and the distal femur with 1 case. The clinical presentation was as a mass in 2 cases, 1 patient noticed the mass after trauma, 1 case noticed pain and in 4 cases the diagnosis was incidental during imaging scans performed for other reasons. The mean duration of symptoms was 7 months.
Patient #3 debuted with pulmonary metastases and was diagnosed with parosteal osteosarcoma (Broders grade 1).
The diagnosis of ddPO was synchronous in 1 patient and metachronous in 2 cases. In metachronous patients the time elapsed between diagnosis of the initial lesion and diagnosis of ddPO was 11 months.
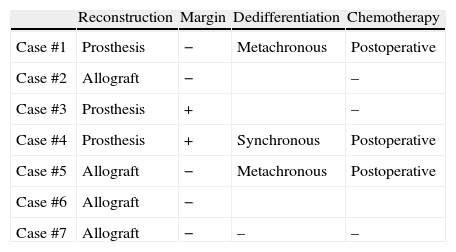
Radiographic findingsWe reviewed the plain radiographs of all patients, as well as computed tomography (CT) and/or magnetic resonance imaging (MRI) scans of entire limbs. We also examined chest CT and whole-body bone scintigraphy scans with Tc99m. Infiltration of the spinal canal occurred in 2 cases: patients #3 and #4 (28.5%) (Tables 1 and 2).
Clinical characteristics of patients.
| Age | Gender | Location | Diagnosis | Medullar invasion | Stage | |
| Case #1 | 29 | Male | Proximal femur | Mass | − | Ia |
| Case #2 | 47 | Male | Humeral diaphysis | Incidental | − | Ia |
| Case #3 | 24 | Male | Proximal humeral metaphysis | Incidental | + | III |
| Case #4 | 24 | Female | Distal femur | Pain | + | Ib |
| Case #5 | 37 | Male | Distal femur | Incidental | − | Ia |
| Case #6 | 27 | Male | Distal femur | Incidental | − | Ia |
| Case #7 | 37 | Female | Distal femur | Mass | − | Ia |
Treatment.
| Reconstruction | Margin | Dedifferentiation | Chemotherapy | |
| Case #1 | Prosthesis | − | Metachronous | Postoperative |
| Case #2 | Allograft | − | – | |
| Case #3 | Prosthesis | + | – | |
| Case #4 | Prosthesis | + | Synchronous | Postoperative |
| Case #5 | Allograft | − | Metachronous | Postoperative |
| Case #6 | Allograft | − | ||
| Case #7 | Allograft | − | – | – |
A total of 6 patients presented tumours of Broders grade 1 and patient #3 presented microscopic foci of Broders grade 3 at the surgical margins.
Histologically, the dedifferentiation component was osteoblastic.
Two local recurrences appeared during follow-up and both were high-grade malignancies (one had been a wide margin and the other had been marginal).
Treatment and follow-upAll 7 patients underwent surgical treatment. In all cases we attempted resection with wide margins, with this being achieved in 5 cases, whilst in the remaining 2 we obtained positive microscopic margins. Reconstruction was performed by tumoural prostheses in 3 cases (Fig. 1) and by allografts in 4 cases (Fig. 2).
Patient #4 (Fig. 3) in whom a positive margin was obtained underwent a wide and intercalary hemicortical resection, as well as reconstruction with hemicortical intercalary allograft. In the osteotomy area, the margin was positive with 2 microscopic nodules of high-grade malignancy. The case was assessed by a multidisciplinary committee which opted for neoadjuvant chemotherapy, reoperation to extend the margins and reconstruction with megaprostheses followed by postoperative chemotherapy.
Patient #3, who debuted with pulmonary metastases, underwent left lung lobectomy.
Three patients received postoperative chemotherapy.
DiscussionParosteal osteosarcomas are well-differentiated tumours, that is, a subtype of low-grade osteosarcoma, arising from the bone surface. They were first described as a new and separate entity by Geschickter and Copeland in 1951.3 This lesion is rare and only represents 5% of all osteosarcomas. Malignant tumours may appear without symptoms and only be identified as incidental findings in imaging studies conducted for other reasons. Patients may refer to the onset of symptoms after sport or trauma.4 The age of onset is between 20 and 40 years, with a predominance of adults over adolescents and females over males, unlike in classical osteosarcoma.5 In our study there was a predominance of males (5:2). Symptoms include slow growth, hard mass with or without mild pain, often associated with limitation of joint motion due to mechanical obstruction. It is striking that the discovery was incidental in 4 out of 7 tumours. These tumours usually affect the metaphysis of long bones, especially the posterior side of the distal femur in 70% of cases.6 This finding is similar to that obtained in our series. Larger tumours may surround the bone. The classical radiographic feature is a dense mass with a broad base of implantation in the cortex. Radiological diagnosis should consider a differential diagnosis with: parosteal osteoma, parosteal lipoma, myositis ossificans, melorheostosis, sessile osteochondroma and conventional osteosarcoma with an extraosseous component. The lesion presents increased uptake on bone scintigraphy scans.
Parosteal osteosarcomas are only treated by surgery, through surgical excision with wide margins. In some cases, the resection can be hemicortical.7 Bone reconstruction can be carried out by intercalary allograft, hemicortical intercalary allograft or tumoural prosthesis. Chemotherapy is reserved for cases of dedifferentiation to high-grade tumours.
The prognostic implications of intramedullary extension of parosteal osteosarcomas remain controversial. For some authors they do not imply a worse prognosis.8 Our group, like that of Campanacci,9 considers the invasion of the intramedullary canal as an extracompartmental extension,10 thus representing a more advanced stage. In our study there were 2 cases of intramedullary invasion (cases #3 and #4). One of them debuted with metastases and the other was a ddPO.
The definition of ddPO is the association of a low-grade parosteal osteosarcoma and a high-grade sarcoma. This case should be clearly distinguished from that of high-grade surface osteosarcoma, which lacks the presence of a low-grade parosteal component.11 This dedifferentiation may occur at the time of presentation (synchronous type) or at the time of recurrence (metachronous type).2
ddPO are not uncommon, with rates between 16% and 43% being reported in the literature. The incidence of ddPO in the series of the Rizzoli Institute was higher than that in the series of the Mayo Clinic (16% vs 20%). However, it was lower than those in the series of patients from Programs Division from Gainesville, Florida (33%) and the University of Texas MD Anderson Cancer Centre (43%). These variable rates may be a reflection of patient selection or a more cautious approach to preoperative identification.
ddPO have worse outcomes with higher rates of recurrence, metastasis and mortality. These rates are higher in metachronous cases. Since these are high-grade sarcomas, they should follow chemotherapy treatment protocols.
It is difficult to detect these areas of dedifferentiation through biopsy. Therefore, pathologists must analyse surgical specimens in detail, seeking areas of dedifferentiation which could lead to a change in prognosis and therapeutic approach. Adjuvant chemotherapy is administered to patients with ddPO after histopathological confirmation following tumour resection. If histological dedifferentiation can be confirmed during biopsy, then it may be possible to plan a more aggressive treatment with neoadjuvant chemotherapy.8
A systematic follow-up should be conducted when treating parosteal osteosarcomas, as the variety being treated may be the more aggressive one.
Some authors maintain that dedifferentiation should be suspected in large parosteal osteosarcomas, specifically those which appear as lobulated masses with irregular margins and those with a mixed radiographic pattern combining dense and lithic areas.12
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Encinas-Ullán CA, et al. Osteosarcomas parostales: resultados infrecuentes. Rev Esp Cir Ortop Traumatol. 2012;56:281–5.