Ligament reconstruction and tendon interposition (LRTI) arthroplasty is the procedure of choice of most hand surgeons in the treatment of basal joint arthritis of the thumb. Progressive and natural collapse after trapeziectomy is a common problem.
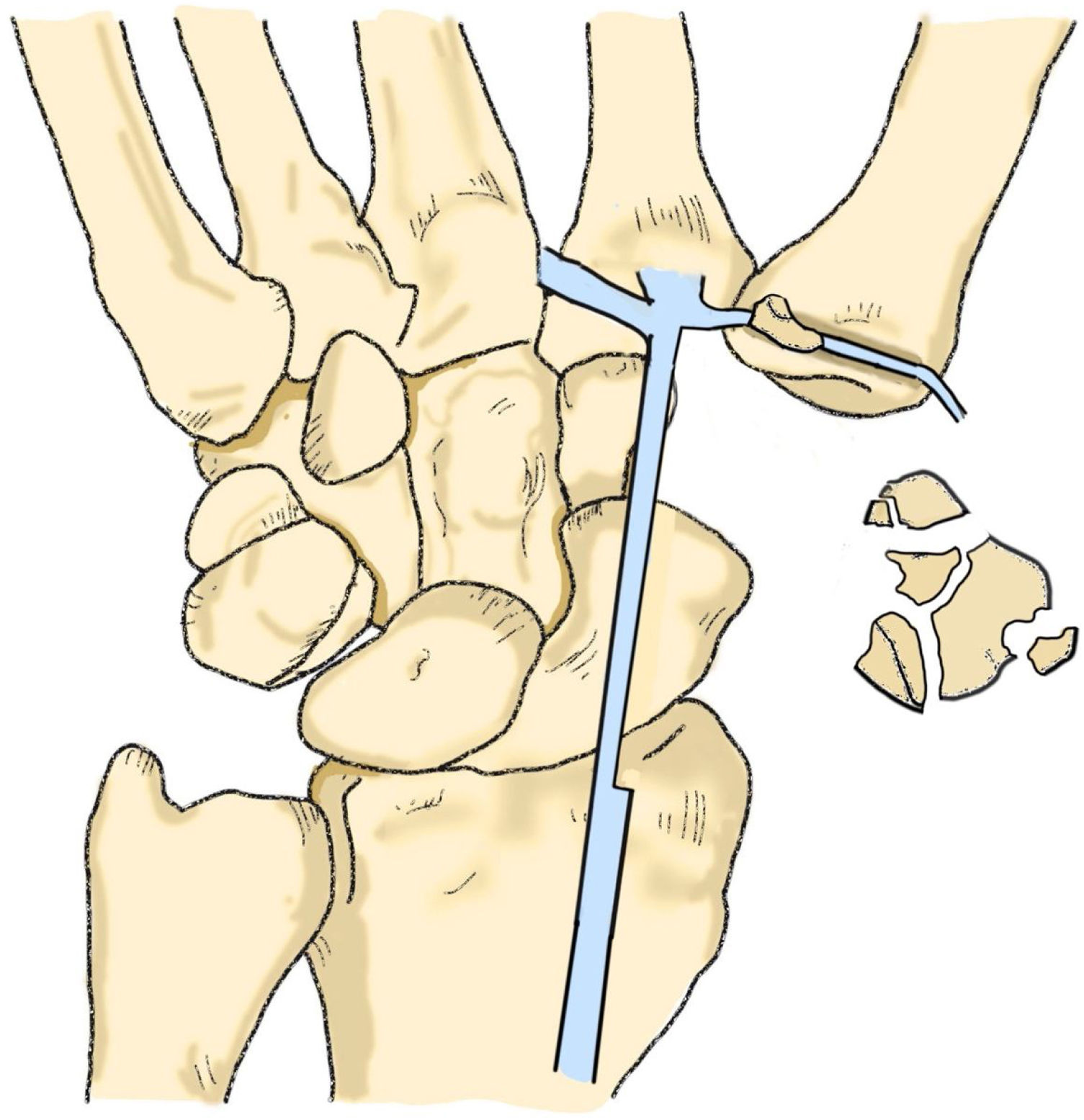
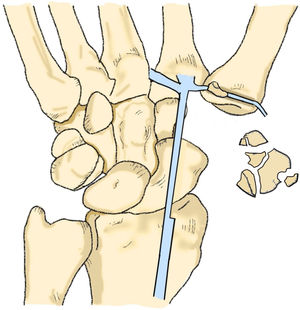
Description of techniqueWe performed LRTI with flexor carpi radialis (FCR) hemitendon technique, then proceeded to block the hemitendon plasty with a bone fragment at the base of the metacarpal. This technique allows us to maintain tension and to obtain immediate stability.
Patients and methodsWe conducted a single-center retrospective longitudinal observational study including 51 patients with diagnosis of symptomatic osteoarthritis of the trapeziometacarpal joint. Group A consisted of 24 thumbs treated with trapeziectomy with LRTI with FCR hemitendon using the Burton-Pellegrini technique. Group B included 27 thumbs treated using the modified technique. The postoperative height of the Scaphometacarpal (SM) space was analyzed. Clinical outcome, opposition, retroversion, patient satisfaction and surgical timing were studied.
ResultsThe difference of the SM space, after applying correction factor, at one and six months postoperative is significantly less in the modified technique group (p=0.033 and p=0.001 respectively). The average height loss of the SM space from one to six months postoperative measurement was smaller in the study group, showing greater stability of the plasty.
ConclusionsThe use of a bone fragment to block the FCR plasty improves the results at one and six months postoperatively, showing a diminished height loss of the SM space, improved thumb opposition and without prolonging surgical timing in our series.
La artroplastia con reconstrucción ligamentosa e interposición tendinosa (LRTI, en inglés) es el procedimiento de elección para tratar la rizartrosis. El colapso progresivo tras la trapeciectomía es un problema habitual.
Descripción de la técnicaRealizamos una LRTI con el hemitendón del flexor carpis radialis (FCR) y, posteriormente, colocamos un fragmento óseo en la base del metacarpo para bloquear la plastia. Esta técnica nos permite obtener estabilidad inmediata y mantener la tensión.
MétodoPresentamos un estudio observacional longitudinal retrospectivo unicéntrico, que incluye a 51 pacientes con diagnóstico de rizartrosis sintomática. Los pacientes se dividieron en 2 grupos: grupo A, pacientes intervenidos mediante trapeciectomía con LRTI del FCR según la técnica de Burton-Pellegrini y grupo B, pacientes intervenidos mediante la técnica modificada. Se analizó la altura del espacio escafometacarpiano (EM) restante en radiografías postoperatorias. Se valoraron los resultados clínicos, como la oposición o retroversión del pulgar, satisfacción del paciente y tiempo quirúrgico.
ResultadosLas diferencias en altura del espacio EM a uno y 6 meses tras la cirugía son significativamente menores con la técnica modificada (p=0,033 y p=0,001, respectivamente). La pérdida de altura media del espacio EM del primer al sexto mes tras la cirugía fue menor en el grupo B, con mayor estabilidad de la plastia.
ConclusiónEl uso de un fragmento óseo para bloquear la plastia del FCR mejora los resultados clínicos y radiológicos a uno y 6 meses tras la cirugía, con menor pérdida de altura del espacio EM y mejoría de la oposición del pulgar, sin aumentar el tiempo quirúrgico.
In the treatment of basal joint arthritis of the thumb, ligament reconstruction and tendon interposition arthroplasty (LRTI) as first described by Burton1 and then by Burton and Pelligrini,2 similar to the Eaton and Littler3 and Eaton et al. technique,4 is the procedure of choice of most hand surgeons.
This classic technique is based on performing a total or partial trapeziectomy followed by a ligamentoplasty to stabilize the thumb, in attempt to avoid losing too much length and maintaining the created space that would consequently improve the outcomes by diminishing the natural tendency of progressive collapse. The height of the Scaphometacarpal (SM) space has shown no direct influence in functional5 or clinical results,6 nevertheless it allows us to evaluate the stability of the arthroplasty. However, in cases of total collapse (subsidence), it does lead directly to pain and functional impairment,7 so it should therefore not be disregarded as clinically irrelevant.
Trapeziectomy alone has not been able to show better results,5,7–12 but does seem to have less adverse events according to the Cochrane revision.12 Recent literature fails to demonstrate superiority in LRTI technique over other procedures, due to the lack of methodological quality and inconsistency in the results published.10–16
The average height loss of the SM space after total trapeziectomy fluctuates from 45% to 80%, arriving sometimes to a total collapse of the space (subsidence). These results are similar throughout the different techniques applied, including those with the use of a temporal Kirschner wire.17
We aim to describe results of a modification of the widely applied technique, where an autograft bone fragment is used to stabilize the FCR plasty, in the surgical treatment of basal joint arthritis of the thumb.
Surgical techniqueUnder regional anesthesia, with the use of a tourniquet at the base of the arm we performed the LRTI with FCR hemitendon technique. Wagner anterior approach was used; we identified and protected the sensitive branches of the radial nerve, performed a total trapeziectomy through fragmenting and afterwards total excision. At the base of the first metacarpal the medial osteophytes were resected and a tunnel was perforated, using a 3.5 or 4mm drill depending on the thickness of the hemitendon. Beginning at the medial border of the base of the metacarpal directed to the dorsoradial cortex using an oblique orientation, perpendicular to the axis of the nail. Half of the FCR tendon was separated up until the beginning of the muscular mass and later on passed snugly through the tunnel. The thumb was placed in an abducted position, pressing the base of the first metacarpal toward the second metacarpal and meanwhile tightening the hemitendon from the radial side. Once the desired position was obtained, we proceeded to block the plasty at the base of the tunnel with a bone fragment. (Figs. 1 and 2) This technique allows us to maintain the tension as well as obtaining immediate stability. Finally, the transferred hemitendon is sutured to the other hemitendon and the remaining portion of the autograft was fashioned as a mass and interposed between the scaphoid and the base of the first metacarpal. The remaining of the procedure and closure were performed without modifications to usual approach.
The thumb and wrist were immobilized using a well-padded Spica cast, nonetheless avoiding hyperextension of the metacarpophalangeal of the thumb. Immobilization was removed after 2 weeks along with external suture and the patient was instructed on progressive rehabilitation exercises. Use of the hand was allowed except for weight carrying, which was delayed after 12 weeks post-operative.
Patients and methodsThis is a single center retrospective longitudinal observational study including 51 consecutive patients treated by the same surgeon (author of the technique JMAR), in our center with the diagnosis of symptomatic osteoarthritis of the trapeziometacarpal joint, of at least stage II of the Eaton classification.4 Informed signed consent was obtained in all patients. The institutional ethics and review boards committee approved the study (Register no. HCB/2020/1962). Group A consisted of 24 thumbs in 24 patients treated with trapeziectomy with LRTI with FCR hemitendon using the Burton and Pellegrini technique,2 between 2010 and 2015. Group B included 27 thumbs of 25 patients treated between 2015 and 2018, using the technique with the modification of blocking the hemitendon with a bone fragment at the base of the first metacarpal.
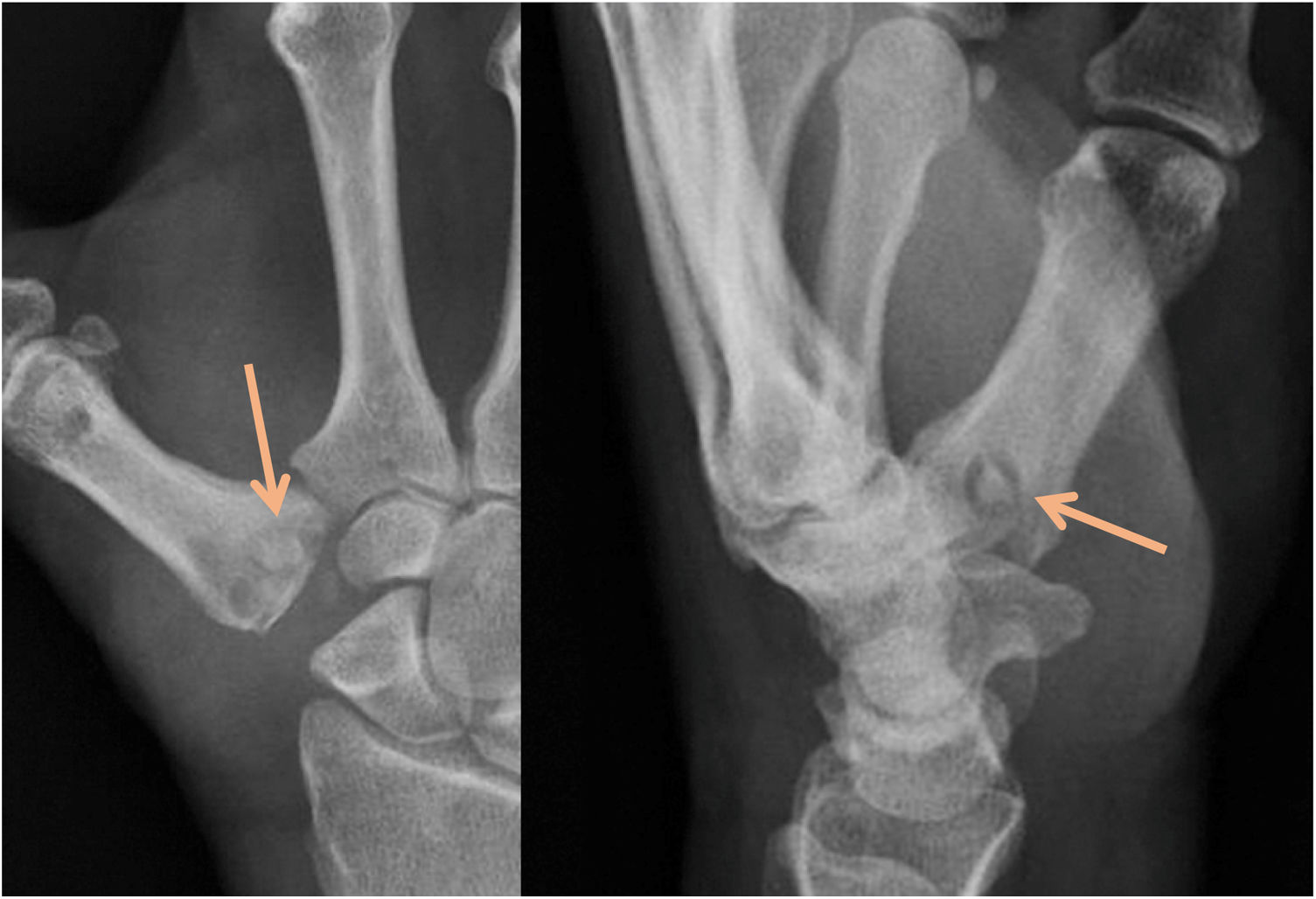
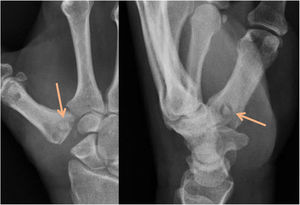
We analyzed the preoperative X-ray with the Eaton et al. scale,4 measured the SM space and the length of the first phalanx of the thumb following the Kadiyala et al. method,18 that is based upon the fundament that the measurement of the SM space done over an X-ray image might be altered by the technical characteristics. Therefore, needing a correction measurement such as the length of the phalanx as a stable reference not modified in the surgical procedure.
The SM space and the length of the first phalanx of the thumb were measured in X-rays taken preoperatively, 1 and 6 months after surgery (Raim DICOM Viewer imaging system). The height of the SM space and the length of the first phalanx were related using the technique proposed by Kadiyala et al.18
Thumb mobility was measured at 6 months follow up, using Kapandji's scales19 to evaluate opposition (ability to oppose it to the 5th finger), with a score between 0 and 10 (0 being only able to reach radial aspect of the proximal phalanx of the index finger and 10 being able to reach the distal palmar crease, considered maximal opposition). Retroversion was also evaluated (ability to lift up the thumb), with a score between 0 and 4.19
Baseline characteristics were described using median and 95% confidence intervals (95% CI) and absolute range (Minimum; maximum) or absolute frequencies and percentages (%) and analyzed by Mann–Whitney U test or Fisher's exact test for quantitative or qualitative variables, respectively. Final satisfaction and surgical time were also analyzed using Mann–Whitney U test. We assessed the longitudinal evolution according to surgical group. For these analyses, we used generalized estimating equations (GEE) models, with an estimation of within-subject correlation from autoregressive approach. A two-sided type I error of 5% was applied. Analyses were performed in the SPSS v.25 Statistical Package (Armonk, NY: IBM Corp.)
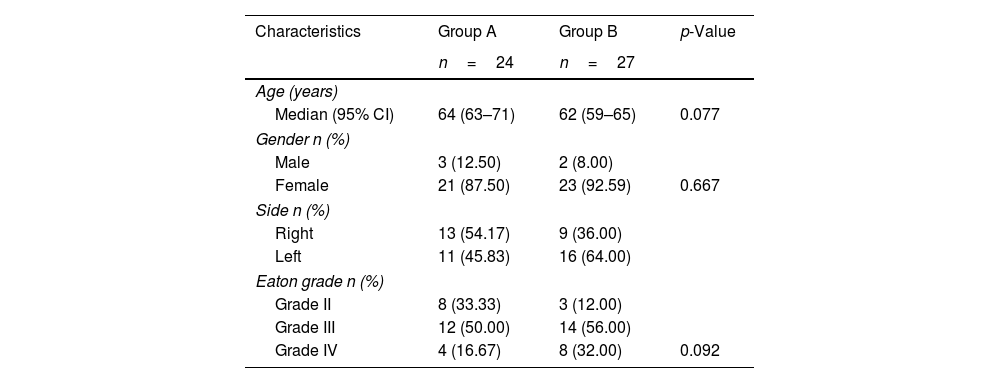
ResultsThere were no significant differences between the two series according to sex (p=0.667), age (p=0.077), preoperative SM space height (p=0.476), and arthrosis level (p=0.092) (Table 1) and therefore considered the groups to be similar.
Demographics of the patients.
| Characteristics | Group A | Group B | p-Value |
|---|---|---|---|
| n=24 | n=27 | ||
| Age (years) | |||
| Median (95% CI) | 64 (63–71) | 62 (59–65) | 0.077 |
| Gender n (%) | |||
| Male | 3 (12.50) | 2 (8.00) | |
| Female | 21 (87.50) | 23 (92.59) | 0.667 |
| Side n (%) | |||
| Right | 13 (54.17) | 9 (36.00) | |
| Left | 11 (45.83) | 16 (64.00) | |
| Eaton grade n (%) | |||
| Grade II | 8 (33.33) | 3 (12.00) | |
| Grade III | 12 (50.00) | 14 (56.00) | |
| Grade IV | 4 (16.67) | 8 (32.00) | 0.092 |
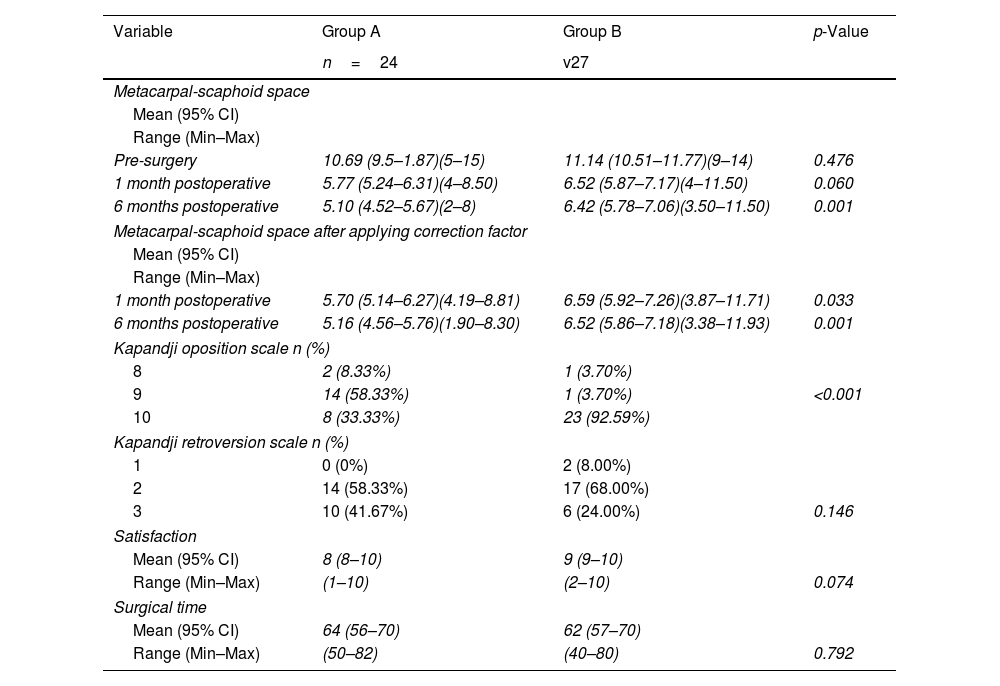
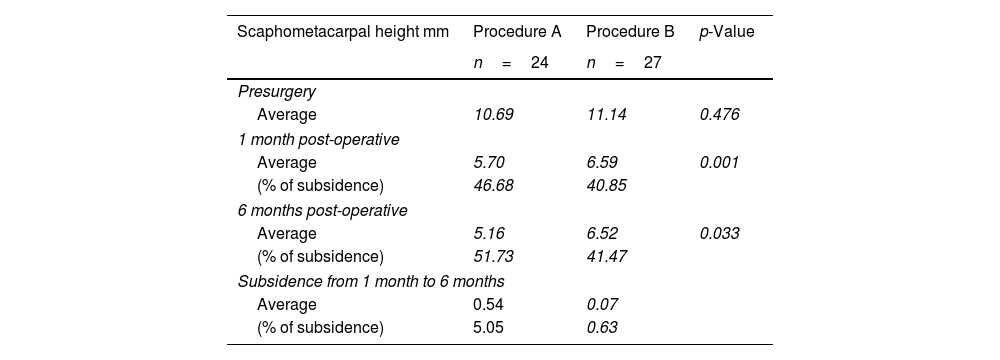
The difference of the SM space, after applying correction factor, at one month postoperative is significantly less in group B (p=0.033), as well as when evaluated at 6 months postoperative (6.52 vs 5.16) (p=0.001). The average height loss of the SM space from 1 month postoperative to the 6 months postoperative measurement was smaller in group B (0.54 vs 0.07), showing greater stability of the plasty. The height lost at 6 months follow up in group A was of 51.73%, meanwhile in group B it represented a 41.47% height loss. A predominance of favorable results in group B can be appreciated at 1 month postoperative as well as 6 months thereafter (Tables 2 and 3).
Results according to the applied procedure.
| Variable | Group A | Group B | p-Value |
|---|---|---|---|
| n=24 | v27 | ||
| Metacarpal-scaphoid space | |||
| Mean (95% CI) | |||
| Range (Min–Max) | |||
| Pre-surgery | 10.69 (9.5–1.87)(5–15) | 11.14 (10.51–11.77)(9–14) | 0.476 |
| 1 month postoperative | 5.77 (5.24–6.31)(4–8.50) | 6.52 (5.87–7.17)(4–11.50) | 0.060 |
| 6 months postoperative | 5.10 (4.52–5.67)(2–8) | 6.42 (5.78–7.06)(3.50–11.50) | 0.001 |
| Metacarpal-scaphoid space after applying correction factor | |||
| Mean (95% CI) | |||
| Range (Min–Max) | |||
| 1 month postoperative | 5.70 (5.14–6.27)(4.19–8.81) | 6.59 (5.92–7.26)(3.87–11.71) | 0.033 |
| 6 months postoperative | 5.16 (4.56–5.76)(1.90–8.30) | 6.52 (5.86–7.18)(3.38–11.93) | 0.001 |
| Kapandji oposition scale n (%) | |||
| 8 | 2 (8.33%) | 1 (3.70%) | |
| 9 | 14 (58.33%) | 1 (3.70%) | <0.001 |
| 10 | 8 (33.33%) | 23 (92.59%) | |
| Kapandji retroversion scale n (%) | |||
| 1 | 0 (0%) | 2 (8.00%) | |
| 2 | 14 (58.33%) | 17 (68.00%) | |
| 3 | 10 (41.67%) | 6 (24.00%) | 0.146 |
| Satisfaction | |||
| Mean (95% CI) | 8 (8–10) | 9 (9–10) | |
| Range (Min–Max) | (1–10) | (2–10) | 0.074 |
| Surgical time | |||
| Mean (95% CI) | 64 (56–70) | 62 (57–70) | |
| Range (Min–Max) | (50–82) | (40–80) | 0.792 |
Results of the scaphometacarpal space measurements.
| Scaphometacarpal height mm | Procedure A | Procedure B | p-Value |
|---|---|---|---|
| n=24 | n=27 | ||
| Presurgery | |||
| Average | 10.69 | 11.14 | 0.476 |
| 1 month post-operative | |||
| Average | 5.70 | 6.59 | 0.001 |
| (% of subsidence) | 46.68 | 40.85 | |
| 6 months post-operative | |||
| Average | 5.16 | 6.52 | 0.033 |
| (% of subsidence) | 51.73 | 41.47 | |
| Subsidence from 1 month to 6 months | |||
| Average | 0.54 | 0.07 | |
| (% of subsidence) | 5.05 | 0.63 | |
Regarding mobility we also found encouraging results, measuring opposition using Kapandji's method,19 showed better outcome in group B (p<0.001); nonetheless it showed no significant difference in retroversion (p=0.146). Surgical time was not different between the two groups (p=0.792), therefore obtaining the bone fragment represents no increment in surgical time. Subjective satisfaction with the procedure was high in both groups, without significant difference between them (p=0.085).
DiscussionIn the surgical treatment of basal joint arthritis of the thumb of Eaton et al. stages II, III and IV most hand surgeons prefer the LRTI technique.4 Yuan et al. analyzing the US clinical practice in regards to rizarthrosis of the thumb considered 3530 patients. 84% of the 2966 surgeons that answered the poll utilized the LRTI technique in the year 2001. Increasing to 90% in the year 2010.20 Nevertheless, its superiority over other procedures, such as simple trapeziectomy, arthrodesis or trapeziometacarpal prosthesis, has not yet been demonstrated,10–15,21,22 showing variation of results in the literature due to the different measurement systems applied.
When the trapezium has been removed, the intermetacarpal ligament reconstruction is responsible for stabilizing the first metacarpal.23 Between 62%24 and 67.6%25 of hand surgeons in the US, use LRTI with FCR. Of these between 29.7%25 and 34%24 use only half of the tendon and between 42.3%25 and 50%24 use it as a whole.
One of the technical problems of LRTI is achieving adequate ligamentoplasty tension to stabilize the first metacarpal. Various procedures have been used to maintain tension. Geldmacher in 1981 proposed a modification of the FCR ligamentoplasty technique without interposition.26 Brunton and Wittstad, use the entire FCR tendon, blocking it with an absorbable interferential screw placed at the tunnel exit27; Zlotolow et al. perform the plasty with abductor pollicis longus, fixing it with an interferential screw placed in the tunnel of the second metacarpal28 and Julien et al. fix it with a 3-mm screw.29 Three percent of the 1024 US hand surgeons who responded to the survey conducted by Brunton et al. fix the interposed tendon with a harpoon.25 Taylor and Strauch instead use a harpoon-fixed suspension.21
We hypothesize that using an autograft bone fragment to block the plasty at the base of the metacarpal, would provide the plasty immediate stability. We have analyzed a case series, measuring the height of the SM space after total trapeziectomy and LRTI using the measurement method described by Kadiyala et al.,18 comparing it to another similar series in which the tendon was blocked at the entry point of the metacarpal tunnel using a bone fragment. Height of the SM space, mobility of the thumb, surgical time and patient satisfaction were studied.
The first radiological evaluation was performed one-month post operation, seeing as an immediate evaluation would have limited value, added to the fact that some surgeons use a temporary Kirschner wire for four weeks. The second evaluation was performed at the 6 months follow up. After this period annual imaging can be made, but the SM space does not tend to modify in a high percentage throughout time (Fig. 3). Previous studies support that there is no difference when comparing measurements around the 18-month post-surgery.6,7,18,30
The use of this modification of this technique improves the results at 1 month and 6 months after surgery, showing a diminished height loss of the SM space, along with an improved thumb opposition and without prolonging surgical timing in our series.
Certain limitations regarding this study can be acknowledged. Its retrospective cohort nature, in which the cases were operated on by the same surgical team, limits the extent of our conclusions. Likewise, the fact that it is a single center study and having surgeries performed by the same surgeon, can diminish our spectrum as well, increasing internal validity.
Thumb mobility was not assessed preoperatively; it was only addressed in the follow up period. Making it unfeasible to calculate the difference with preoperative mobility, which could be limited in itself by osteoarthritis. Grip strength was also not assessed nor were instruments used to evaluate function and quality of life, since values were assumed to be similar in the two series, but the degree of satisfaction was evaluated. Nevertheless, these were not within the pretended analysis, which was to evaluate which of the two procedures offers greater stability of the plasty with less limitation of mobility.
The technical modification is recommended for all Eaton and Glickel stages,4 even when trapeziectomy is meant to be partial, and also for the treatment of stage I rizoarthrosis of the thumb with the Eaton technique,3 in which the trapezium is not resected. In these cases, the graft can be obtained from the trapezium itself or from the distal epiphysis of the radius with a trephine. If the ligamentoplasty procedure is performed by a dorsal access, the graft can be placed on the radial side, at the exit of the tunnel at the base of the first MC. The blocking of the plasty is applicable to other types of ligamentoplasty used for the treatment of rizarthrosis of the thumb.
ConclusionLRTI is the preferred method for thumb arthritis by most hand surgeons worldwide. Its superiority over other methods has not yet been described. We present a modification of Burton-Pellegrini technique which shows promising results at 1 and 6 months after surgery, both clinical and radiological.
Level of evidenceLevel of evidence ii.
Authors’ contributionCVR: design, data collection, draft of manuscript.
JRG: statistical analysis.
ACR: design, draft of manuscript.
CCP: data collection.
JNS: data collection.
JMAR: design, draft of manuscript, senior surgeon. Author of the modified technique.
All authors read and approved the final version.
Ethical approvalHCB/2020/1262.
FundingNone.
Conflict of interestNone.
Ms. Marina Prat Carreño for the schematic image of the technique.