Interstitial Lung Disease Associated with Autoimmune Diseases
Más datosAnti-synthetase syndrome is a recently characterized entity whose morbidity and mortality are mainly determined by interstitial lung involvement. For this reason, it is considered important to identify the association between the presence of anti-synthetase antibodies and the presence and putatively, the development of a specific radiological pattern of interstitial lung disease.
ObjectiveTo determine the association between the antibodies present at the time of diagnosis of anti-synthetase syndrome and the presence of interstitial lung disease.
Materials and methodsSystematic review of the literature and meta-analysis. The search strategy was carried out in: EMBASE, LILACS, PUBMED, CENTRAL (Cochrane), and Grey Literature. The primary outcomes were the detection of the different radiological patterns of interstitial lung disease, and the reported specific anti-synthetase antibody.
ResultsOne hundred seventy-six patients were identified; Jo-1 in combination with NSIP was the most frequent pattern. Quantitative analysis suggests that PL-7 expression is associated with the presence of UIP and NSIP. For obstructive pneumonitis, a relationship was observed with the presence of anti EJ, while the expression of PL-7 was negatively associated. Also, EJ had a negative association with the presence of NSIP. The observed associations were corroborated with the subgroup analysis carried out using the two retrospective observational studies identified.
ConclusionDespite the limitations, PL-7 and EJ showed significant associations with the presence of specific patterns of interstitial lung disease. Jo-1 did not have a significant specific association. Studies of higher methodological quality are required to generate recommendations that affect clinical practice.
El síndrome antisintetasa es una entidad recientemente caracterizada, cuya morbimortalidad está determinada principalmente por el compromiso pulmonar intersticial; por esta razón, se considera importante identificar la agrupación entre la presencia de los anticuerpos antisintetasa y el desarrollo de un patrón radiológico específico de la enfermedad pulmonar intersticial.
ObjetivoDeterminar la asociación entre los anticuerpos presentes al momento del diagnóstico de síndrome antisintetasa y el desarrollo de la enfermedad pulmonar intersticial.
MétodosRevisión sistemática de la literatura y metaanálisis; se empleó la estrategia de búsqueda en Embase, Lilacs, PubMed, Central (Cochrane) y Grey LIterature. Los desenlaces primarios fueron la detección de los diferentes patrones radiológicos de enfermedad pulmonar intersticial, así como el anticuerpo antisintetasa específico reportado.
ResultadosFueron identificados 176 pacientes, siendo antihistidil-ARNt (Jo-1) y el patrón de neumonía intersticial no específica (NINE), los de mayor frecuencia. El análisis cuantitativo sugiere que la expresión de treonil-ARNt sintetasa (PL-7) se asocia con el desarrollo de neumonía intersticial usual (NIU) y NINE. En el patrón de NO, se observó una relación con la presencia de anti-glicil-ARNt sintetasa (anti-EJ), mientras que la expresión de PL-7 presentó una asociación negativa. También, EJ tuvo una unión negativa con el desarrollo de NINE. Las asociaciones observadas fueron corroboradas con el análisis por subgrupos realizados con los dos estudios observacionales retrospectivos identificados.
ConclusiónSe pudo observar una relación entre Jo-1 y PL-7 con el desarrollo de patrones específicos radiológicos de enfermedad pulmonar intersticial. Se requieren estudios de mayor calidad metodológica para generar recomendaciones que impacten la práctica clínica sobre esta enfermedad.
Anti-synthetase syndrome is an autoimmune disease that is defined by the presence of inflammatory myopathy and/or extramuscular manifestations, especially pulmonary disease in the form of interstitial lung disease (ILD). Skin or joint involvement may also be seen. This entity is caused by the presence of antibodies directed against the enzyme aminoacyl transfer ribonucleic acid (tRNA) synthetase, of which 11 antibodies have been described (Jo-1, PL-12, PL-7, EJ, OJ, KS, Zo, SC, JS, YRS/Ha, Wa).1 Diagnostic criteria have been described within these are the criteria of Connor (2010) and Solomon (2011) which are used as initial consideration and as confirmatory respectively.2
Since the relatively recent description and diagnosis of this entity, its prevalence is still not well established. The interstitial lung involvement has been described as an important factor contributing to morbidity and mortality in these patients. Consequently, it is important to correlate the presence of specific anti-synthetase antibodies with the presence of pulmonary interstitial compromise.2
The objective of the study was to assess the association of these specific antibodies with the presence of ILD. Early detection of patients will allow timely and proper interventions to achieve better control of disease activity and quality of life.
Materials and methodsInclusion criteriaTypes of studiesA systematic literature review was conducted to identify observational studies, experimental studies, meta-analyses, and systematic reviews published in English and Spanish.
Types of participantsThe selected studies had to include adult patients over 18 years old diagnosed with anti-synthetase syndrome based on the Connors and Solomon criteria.
Types of interventionStudies reporting the identification of specific anti-synthetase antibodies (Jo-1, PL-7, PL-12, EJ, OJ, KS, ZO, SC, JS, YRS/Ha, or WA) were included.
Types of outcomesThe outcomes established for this review were the detection of ILD through computed tomography (CT) or high-resolution computed tomography (HRCT). Specific patterns of ILD were considered, including non-specific interstitial pneumonia (NSIP), usual interstitial pneumonia (UIP), organizing pneumonia (OP), and findings without a specified pattern. Additional outcomes considered were pulmonary function test results and the presence of pulmonary hypertension based on echocardiogram or right heart catheterization.
Exclusion criteria- •
Studies with experimental animal models.
- •
Lack of adequate results description.
- •
Editorials, letters, opinions, author responses, and comments.
- •
Patients with ILD related to the coexistence of other autoimmune diseases, including other idiopathic inflammatory myopathies.
- •
Patients with a recent diagnosis of pneumonia due to SARS-CoV-2 (within the last 3 months).
- •
Articles that do not meet the quality assessment checklist.
A systematic literature search was conducted to collect studies published between 1996 and March 2023 in English and Spanish. The search was performed in different electronic databases, including EMBASE, LILACS, PUBMED, and CENTRAL (Cochrane). Grey Literature was also used to identify additional publications.
The Boolean operators “AND”, “OR”, “NOT” were used to build the search strategy. Terms used for the searches included: ‘Interstitial lung disease’, ‘Interstitial lung diseases’, ‘Diffuse parenchymal lung disease’, ‘Diffuse parenchymal lung diseases’, ‘Interstitial pneumonitis’, “Interstitial pneumonia”, “Interstitial lung disease”, “Anti-synthetase syndrome”, “Histidine-tRNA Ligase” “Jo-1 antibody”, “PL-7 antibody”, “PL-12 antibody”, “OJ antibody”, “EJ antibody”, “Ks antibody”, “Zo antibody”, “Sc antibody”, “JS antibody”, “YRS/ha antibody”, “Wa antibody”, “Experimental study”, “Observational study”, “Systematic review”, “Meta-analysis’ (Supplementary data 1 and 2).
Data collection and study selectionThe search for studies in the various electronic databases was independently conducted by two researchers (GA and UM) applying the same search terms and strategy. Each researcher performed the study selection process based on the predefined inclusion and exclusion criteria. The initial screening was based on the title, followed by abstract reading, and finally full-text reading. The results of each search and selection process were compared between the researchers to identify redundant reporting. In case of discrepancies regarding a study, a consensus was reached between the two researchers. If the discordance persisted, a third investigator (FSJ) acted as a mediator to determine inclusion eligibility.
For the selection, inclusion, and exclusion of studies, the Rayyan platform was used, considering descriptors such as publication year, primary author, journal, study type, main results, and statistical estimator.
Data storageAn initial database was constructed using Microsoft Office Excel to organize and store relevant information from each selected study for the final review. The information included consisted on number of patients, sex, age, anti-synthetase antibodies, other positive antibodies, diagnosis of ILD (pulmonary function tests, diagnostic method – CT scan or HRCT), compliance with diagnostic criteria, creatin phosphokinase (CPK) levels, environmental exposure history and results of echocardiogram and right heart catheterization, if performed. This information was subsequently entered into the RedCap software to ensure reliability and non-modification of the obtained information, reducing the risk of biases.
Data analysisQuality assessment of evidenceThe CARE guidelines were used for case reports, the instrument proposed by the Joann Briggs Institute was used for case series, the STROBE guidelines for observational studies, the JADAD guidelines for clinical trials, and the AMSTAR-2 guidelines for systematic reviews and meta-analyses (Supplementary data 4–7).3–5
Descriptive analysisA descriptive analysis of measures of central tendency and dispersion was performed for continuous variables based on reported outcomes, available information from the selected studies and depending on the fulfilment of parametric distribution assumptions (means and standard deviations) or not (medians and interquartile ranges). Absolute and relative frequencies were provided for categorical variables.
Measurement of association effectBased on the obtained results, the calculation of size effect (odds ratio) corresponding to the expression of specific anti-synthetase antibodies and the presence of different patterns of ILD was performed.
Meta-analysisA meta-analysis was conducted taking into consideration the quality, design and the provided information from the selected studies. Most studies were case reports. Analysis was performed for the size effect calculated for the presence of each pattern of ILD and the specific antibodies. A forest plot was constructed, and heterogeneity was assessed using the I2 statistic. Heterogeneity was considered substantial if the result was greater than 40% and less than 70%, requiring the use of a random-effects model for its analysis. Additionally, based on the two identified retrospective cohort studies, a subgroup analysis was performed to determine whether the effect size patterns observed in the case reports correlated with the data presented by both cohorts.
These statistical analysis processes were conducted using Cochrane Review Manager (RevMan) 5.3 version (Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014) and STATA 17.0 version.
Bias control strategiesBased on the designs of the included studies, the assessment of the risk of biases was performed. This analysis was also based on the quality assessment using the respective instruments described earlier.
Meta-biasIn this review, most studies were case reports, and the meta-analysis was performed by grouping patients based on antibodies and patterns of ILD. Therefore, the necessary information for a publication meta-bias analysis using funnel plots was not available.
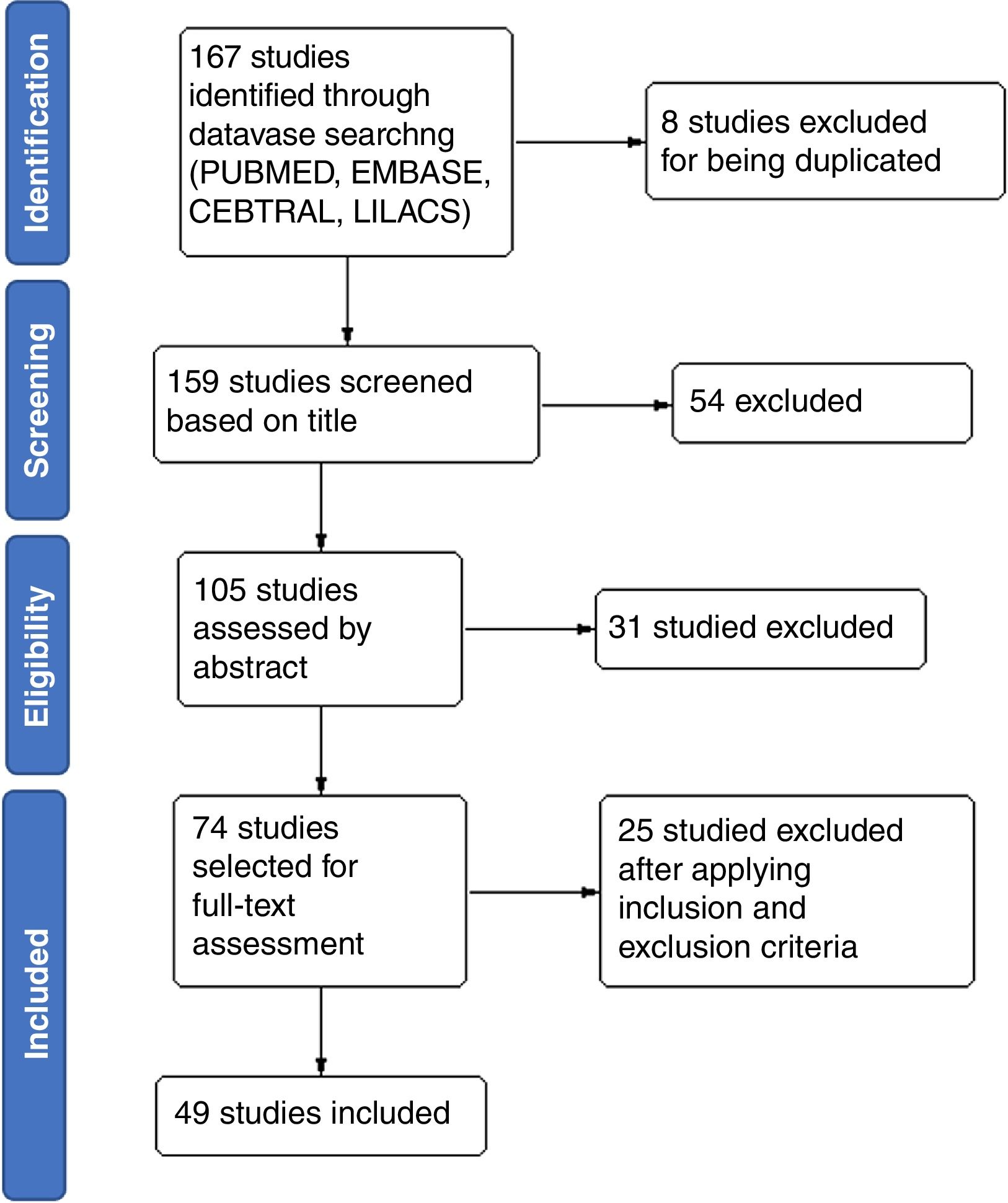
ResultsA total of 167 studies were found after searching in the different electronic databases (EMBASE, MEDLINE, PUBMED, LILACS, Grey Literature). Of these, eight studies were excluded for being duplicates, leaving a total of 159 studies for further assessment. After title screening, 105 studies were selected for abstract reading, from which 74 were selected for full-text assessment. Finally, 49 studies were included in the review (Fig. 1). The description of the main characteristics of the studies excluded in this review can be seen summarized in Supplementary data 3.
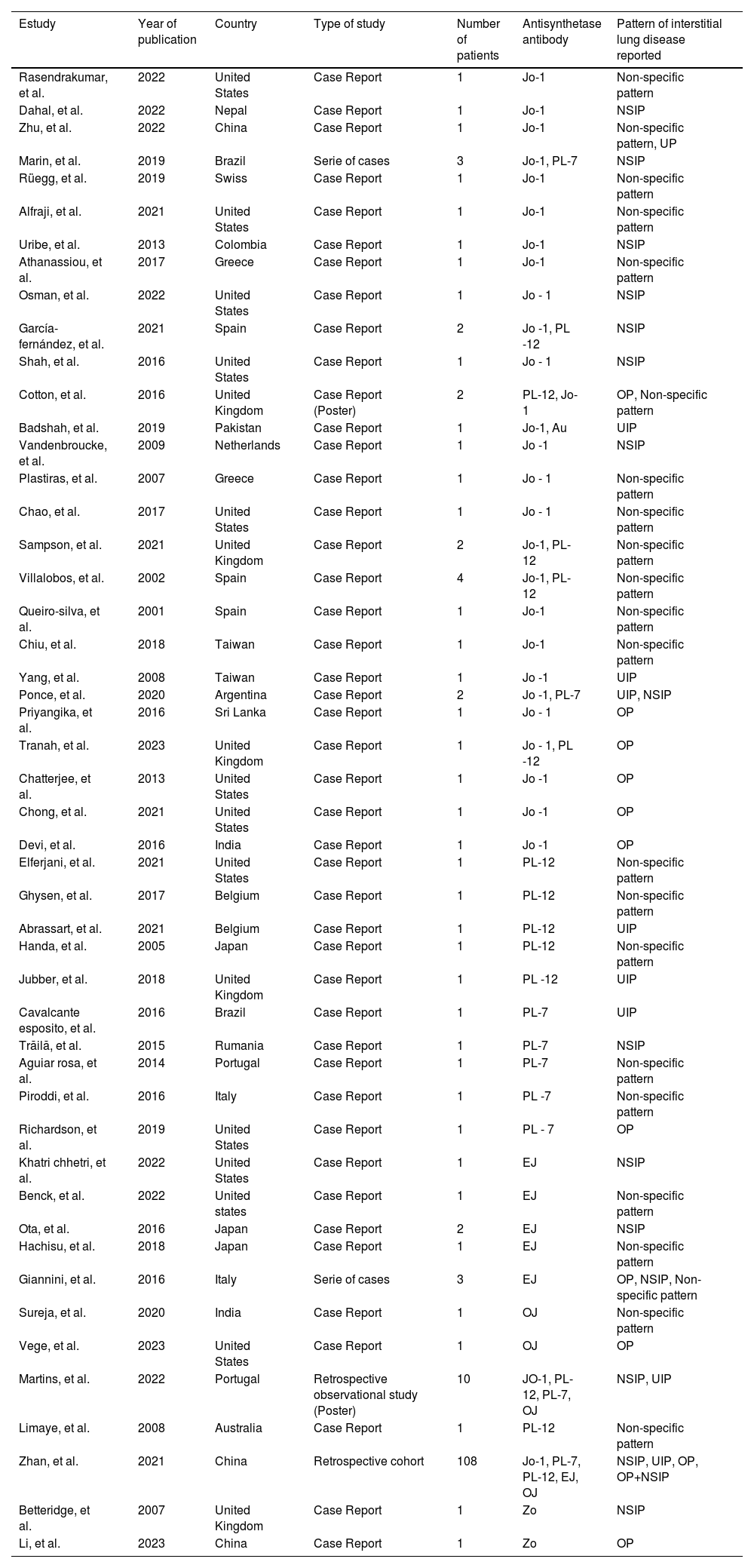
Description of studies and quality assessmentThe description of the main characteristics of the studies included in this review are summarized in Table 1.
Summary of included studies characteristics.
| Estudy | Year of publication | Country | Type of study | Number of patients | Antisynthetase antibody | Pattern of interstitial lung disease reported |
|---|---|---|---|---|---|---|
| Rasendrakumar, et al. | 2022 | United States | Case Report | 1 | Jo-1 | Non-specific pattern |
| Dahal, et al. | 2022 | Nepal | Case Report | 1 | Jo-1 | NSIP |
| Zhu, et al. | 2022 | China | Case Report | 1 | Jo-1 | Non-specific pattern, UP |
| Marin, et al. | 2019 | Brazil | Serie of cases | 3 | Jo-1, PL-7 | NSIP |
| Rüegg, et al. | 2019 | Swiss | Case Report | 1 | Jo-1 | Non-specific pattern |
| Alfraji, et al. | 2021 | United States | Case Report | 1 | Jo-1 | Non-specific pattern |
| Uribe, et al. | 2013 | Colombia | Case Report | 1 | Jo-1 | NSIP |
| Athanassiou, et al. | 2017 | Greece | Case Report | 1 | Jo-1 | Non-specific pattern |
| Osman, et al. | 2022 | United States | Case Report | 1 | Jo - 1 | NSIP |
| García-fernández, et al. | 2021 | Spain | Case Report | 2 | Jo -1, PL -12 | NSIP |
| Shah, et al. | 2016 | United States | Case Report | 1 | Jo - 1 | NSIP |
| Cotton, et al. | 2016 | United Kingdom | Case Report (Poster) | 2 | PL-12, Jo-1 | OP, Non-specific pattern |
| Badshah, et al. | 2019 | Pakistan | Case Report | 1 | Jo-1, Au | UIP |
| Vandenbroucke, et al. | 2009 | Netherlands | Case Report | 1 | Jo -1 | NSIP |
| Plastiras, et al. | 2007 | Greece | Case Report | 1 | Jo - 1 | Non-specific pattern |
| Chao, et al. | 2017 | United States | Case Report | 1 | Jo - 1 | Non-specific pattern |
| Sampson, et al. | 2021 | United Kingdom | Case Report | 2 | Jo-1, PL-12 | Non-specific pattern |
| Villalobos, et al. | 2002 | Spain | Case Report | 4 | Jo-1, PL-12 | Non-specific pattern |
| Queiro-silva, et al. | 2001 | Spain | Case Report | 1 | Jo-1 | Non-specific pattern |
| Chiu, et al. | 2018 | Taiwan | Case Report | 1 | Jo-1 | Non-specific pattern |
| Yang, et al. | 2008 | Taiwan | Case Report | 1 | Jo -1 | UIP |
| Ponce, et al. | 2020 | Argentina | Case Report | 2 | Jo -1, PL-7 | UIP, NSIP |
| Priyangika, et al. | 2016 | Sri Lanka | Case Report | 1 | Jo - 1 | OP |
| Tranah, et al. | 2023 | United Kingdom | Case Report | 1 | Jo - 1, PL -12 | OP |
| Chatterjee, et al. | 2013 | United States | Case Report | 1 | Jo -1 | OP |
| Chong, et al. | 2021 | United States | Case Report | 1 | Jo -1 | OP |
| Devi, et al. | 2016 | India | Case Report | 1 | Jo -1 | OP |
| Elferjani, et al. | 2021 | United States | Case Report | 1 | PL-12 | Non-specific pattern |
| Ghysen, et al. | 2017 | Belgium | Case Report | 1 | PL-12 | Non-specific pattern |
| Abrassart, et al. | 2021 | Belgium | Case Report | 1 | PL-12 | UIP |
| Handa, et al. | 2005 | Japan | Case Report | 1 | PL-12 | Non-specific pattern |
| Jubber, et al. | 2018 | United Kingdom | Case Report | 1 | PL -12 | UIP |
| Cavalcante esposito, et al. | 2016 | Brazil | Case Report | 1 | PL-7 | UIP |
| Trăilă, et al. | 2015 | Rumania | Case Report | 1 | PL-7 | NSIP |
| Aguiar rosa, et al. | 2014 | Portugal | Case Report | 1 | PL-7 | Non-specific pattern |
| Piroddi, et al. | 2016 | Italy | Case Report | 1 | PL -7 | Non-specific pattern |
| Richardson, et al. | 2019 | United States | Case Report | 1 | PL - 7 | OP |
| Khatri chhetri, et al. | 2022 | United States | Case Report | 1 | EJ | NSIP |
| Benck, et al. | 2022 | United states | Case Report | 1 | EJ | Non-specific pattern |
| Ota, et al. | 2016 | Japan | Case Report | 2 | EJ | NSIP |
| Hachisu, et al. | 2018 | Japan | Case Report | 1 | EJ | Non-specific pattern |
| Giannini, et al. | 2016 | Italy | Serie of cases | 3 | EJ | OP, NSIP, Non-specific pattern |
| Sureja, et al. | 2020 | India | Case Report | 1 | OJ | Non-specific pattern |
| Vege, et al. | 2023 | United States | Case Report | 1 | OJ | OP |
| Martins, et al. | 2022 | Portugal | Retrospective observational study (Poster) | 10 | JO-1, PL-12, PL-7, OJ | NSIP, UIP |
| Limaye, et al. | 2008 | Australia | Case Report | 1 | PL-12 | Non-specific pattern |
| Zhan, et al. | 2021 | China | Retrospective cohort | 108 | Jo-1, PL-7, PL-12, EJ, OJ | NSIP, UIP, OP, OP+NSIP |
| Betteridge, et al. | 2007 | United Kingdom | Case Report | 1 | Zo | NSIP |
| Li, et al. | 2023 | China | Case Report | 1 | Zo | OP |
Abbreviations: NSIP: non-specific interstitial pneumonia, UIP: Usual interstitial pneumonia, OP: organizing pneumonia
A total of 28 case reports were found for Jo-1, with a total of 32 patients. In seven studies, eight patients with NSIP were reported.6–12 Ten studies reported a non-specific pattern in 13 patients.13–23 Four case reports with UIP pattern were identified.14,24–26 Finally, six case reports describing an OP pattern were obtained.27–32
A total of five case reports of EJ antibody were found with a total of seven patients. Khatri et al. and Ota et al.,33,34 reported three patients with NSIP, while Benck et al. and Hachisu et al.,35,36 reported three patients with non-specific patterns. Finally, Giannini et al.37 reported a patient with OP.
For OJ antibody, two case reports were obtained for a total of two patients, one with a non-specific pattern38 and another with OP.39
Regarding the presence of PL-7, nine case reports were found, three of them7,26,40 reported four patients with NSIP. Aguiar et al., and Piroddi et al.41,42 presented two patients with a non-specific pattern. One study reported a patient with UIP.43 Finally, a male patient with OP was reported.44
A total of 10 case reports with PL-12 antibody were found. NSIP was reported once,10 while seven cases with non-specific pattern were reported.20,21,27,45–48 UIP pattern was detected in two case reports.49,50 Finally, only Tranah et al. reported a patient with OP.29
Two case reports with ZO antibodies were found, one patient with a NSIP,51 and the other with OP.52
Martins et al., published as an abstract the results of a retrospective observational study with 17 patients from the Portuguese Registry of Rheumatic Diseases, of whom only ten had lung involvement. Of these, six patients were positive for Jo-1 and NSIP, two were Jo-1 positive with UIP pattern, one was OJ positive with NSIP pattern, and one OJ positive with a non-specific pattern.53
Finally, the study of Zhan et al., was a retrospective cohort describing 108 cases from the Chaoyang Hospital in Beijing, China, between December 2017 and March 2019. Of 33 Jo-1 positive patients reported, 18 had OP, 13 with NSIP, and two with NSIP+OP. There were 30 PL-7 positive patients: eight with OP, 15 with NSIP, three with NSIP+OP, and four with UIP. Of the 13 patients with PL-12, four presented OP, eight with NSIP, and one with NSIP+OP. Nine patients with OJ were reported, of which five had OP, two had NSIP, and two had NSIP+OP. Finally, there were 23 EJ positive patients, 18 with OP, four with NSIP, and one with NSIP+OP.54
The CARE guideline was applied to assess the quality of the case reports (Supplementary data 4). In general, none of the studies met all the proposed elements. Only 11 studies included “case report” in the title and two included it within the keywords. Only three studies included the time-line as recommended. Regarding therapeutic interventions, only two studies did not mention the type of intervention carried out, and five did not indicate if there were changes in the treatment and the justification for this conduct. In six studies, no reference was made to follow-up tests. Under the rubric discussion, 28 studies reported the strengths and weaknesses. Unfortunately, none of the included case reports make any mention of the patient's perspective on their case. Finally, 22 case reports do not mention whether informed consent was obtained from the patient for the publication of the study.
There were three studies categorized as case series. The instrument developed by the Joann Briggs Institute (JBI) was used to assess these studies. Only one of the studies presented a standardized method to clearly measure outcomes. It was not clear in any of the studies performed a consecutive case inclusion (Supplementary data 5).
For the quality assessment of the poster published by Martins et al., the STROBE instrument for conference abstracts was used. The title does not mention the type of study carried out, which in this case was a retrospective cohort. They do not specify the use of statistical methods for data analysis. Finally, no associations were made, only the description of results (Supplementary data 6).
Lastly, for the quality assessment of the study by Zhan et al., the STROBE instrument for observational studies was used. The manuscript fully complies with all the parameters requested for quality assessment (Supplementary data 7).
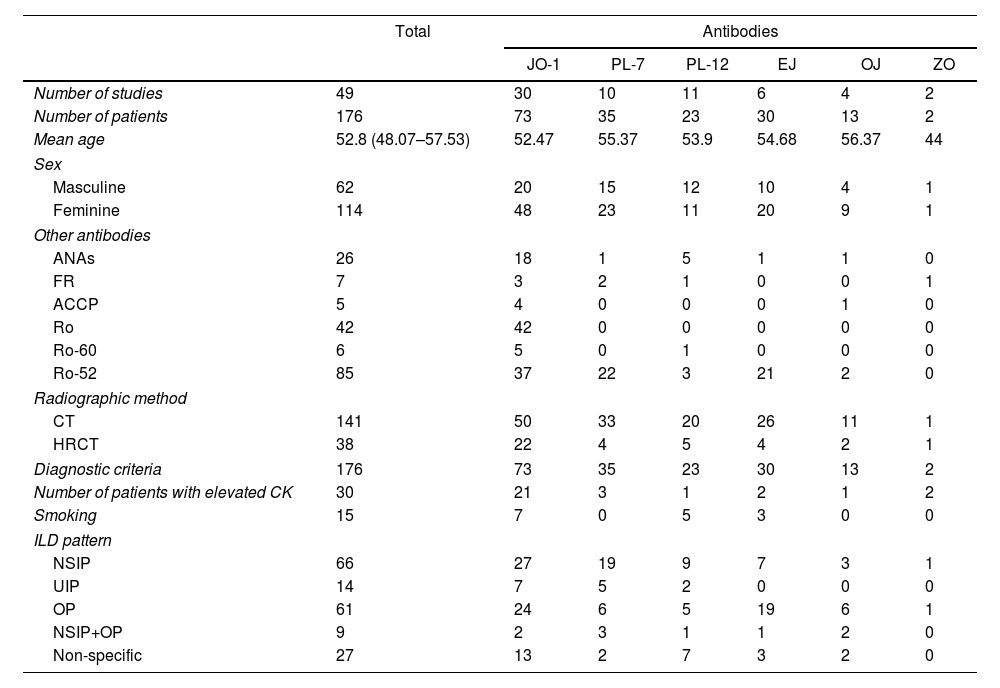
Quantitative analysisBased on the 49 studies included, 176 patients were identified that fulfilled the inclusion criteria for the current study. Demographic characteristics and clinical findings presented by the studies are summarized in Table 2. Mean age of patients was 52.8 years (95% CI: 48.07–57.53). 64% of patients were female. Jo-1 was the most frequently reported anti-synthetase antibody, as well as the most prevalent in patients, and Ro-52 was the most frequent non anti-synthetase antibody registered. The most frequent diagnostic methodology used for the detection of ILD was conventional computed tomography (CT). Interestingly, only 17.2% of patients had elevated CPK levels. Regarding ILD patterns, NSIP was the most frequent (66 patients), followed by OP (61 cases).
Demographic characteristics, and summary of findings in the selected studies.
| Total | Antibodies | ||||||
|---|---|---|---|---|---|---|---|
| JO-1 | PL-7 | PL-12 | EJ | OJ | ZO | ||
| Number of studies | 49 | 30 | 10 | 11 | 6 | 4 | 2 |
| Number of patients | 176 | 73 | 35 | 23 | 30 | 13 | 2 |
| Mean age | 52.8 (48.07–57.53) | 52.47 | 55.37 | 53.9 | 54.68 | 56.37 | 44 |
| Sex | |||||||
| Masculine | 62 | 20 | 15 | 12 | 10 | 4 | 1 |
| Feminine | 114 | 48 | 23 | 11 | 20 | 9 | 1 |
| Other antibodies | |||||||
| ANAs | 26 | 18 | 1 | 5 | 1 | 1 | 0 |
| FR | 7 | 3 | 2 | 1 | 0 | 0 | 1 |
| ACCP | 5 | 4 | 0 | 0 | 0 | 1 | 0 |
| Ro | 42 | 42 | 0 | 0 | 0 | 0 | 0 |
| Ro-60 | 6 | 5 | 0 | 1 | 0 | 0 | 0 |
| Ro-52 | 85 | 37 | 22 | 3 | 21 | 2 | 0 |
| Radiographic method | |||||||
| CT | 141 | 50 | 33 | 20 | 26 | 11 | 1 |
| HRCT | 38 | 22 | 4 | 5 | 4 | 2 | 1 |
| Diagnostic criteria | 176 | 73 | 35 | 23 | 30 | 13 | 2 |
| Number of patients with elevated CK | 30 | 21 | 3 | 1 | 2 | 1 | 2 |
| Smoking | 15 | 7 | 0 | 5 | 3 | 0 | 0 |
| ILD pattern | |||||||
| NSIP | 66 | 27 | 19 | 9 | 7 | 3 | 1 |
| UIP | 14 | 7 | 5 | 2 | 0 | 0 | 0 |
| OP | 61 | 24 | 6 | 5 | 19 | 6 | 1 |
| NSIP+OP | 9 | 2 | 3 | 1 | 1 | 2 | 0 |
| Non-specific | 27 | 13 | 2 | 7 | 3 | 2 | 0 |
Abbreviations: ANA: antinuclear antibodies; RF: rheumatoid factor; CCPA: cyclic citrullinated peptides antibodies; CT: computed tomography; HRCT: high-resolution computed tomography; NSIP: non-specific interstitial pneumonia; UIP: usual interstitial pneumonia; OP: organizing pneumonia.
Quantitative analysis from the information obtained was limited by the fact that 96% of studies were case reports that did not give enough information to calculate individual effect size measurements for each study. For this reason, all patients from the studies were categorized based on the specific anti-synthetase antibody they expressed (Jo-1, PL-7, PL-12, EJ, OJ, ZO). For each group, the specific ILD pattern was determined (NSIP, UIP, OP, NSIP+OP, non-specific pattern). With these data, the odds ratio (OR) for the presence of each pattern based on the specific antibody were calculated.
Based on the calculated OR for each pattern, a meta-analysis focused on comparing the probability of developing each ILD pattern for every antibody was made. For this process, Forest plots were built to assess the heterogeneity between antibodies using the I2 statistic. Given the characteristics of the available data, and the inherent heterogeneity from the use of case reports, a random effect model was applied.
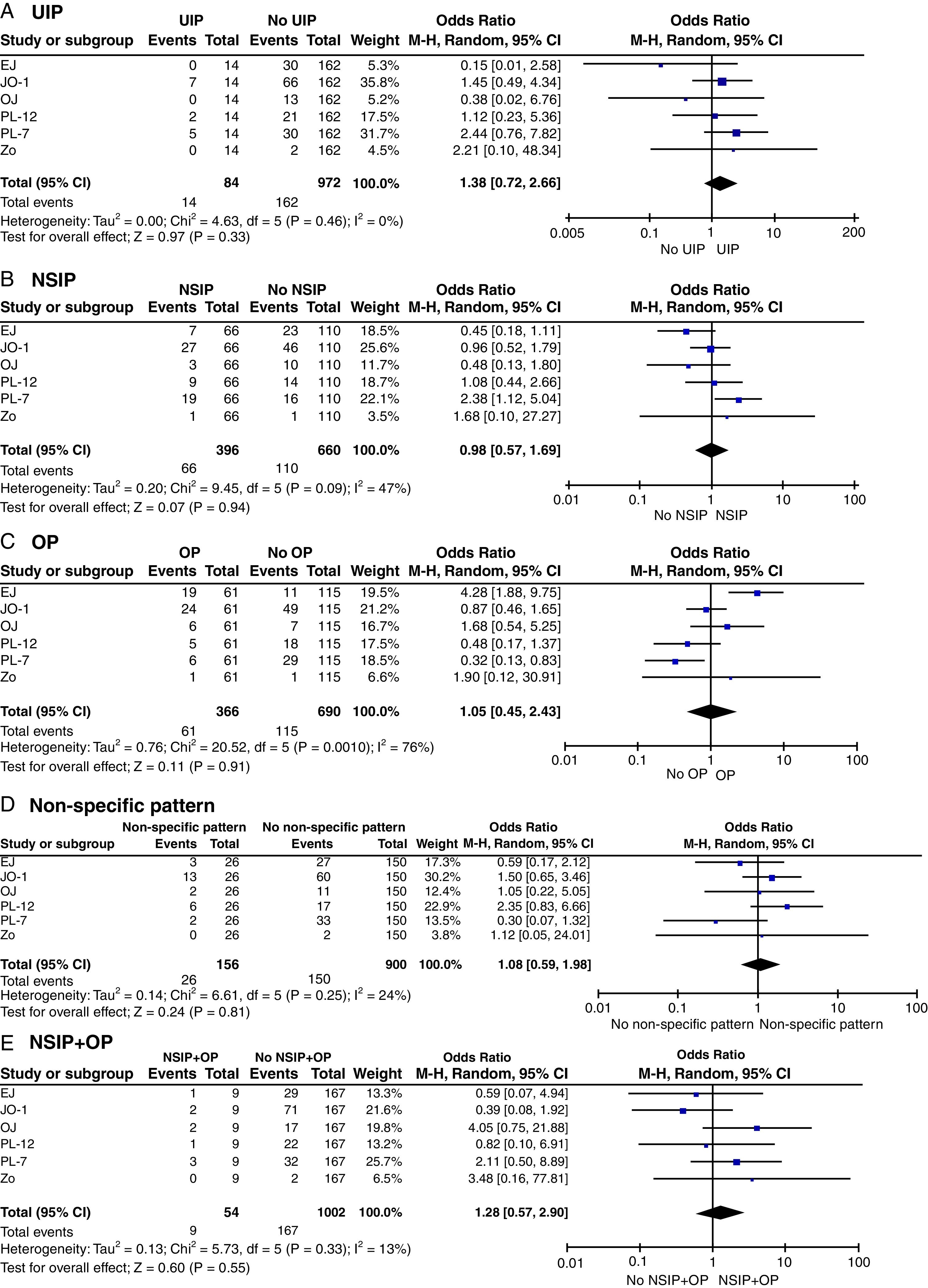
The presence of PL-7 had the greatest positive association with the UIP pattern (OR 2.44, 95% CI 0.76–7.82), but it was not statistically significant. For the expression of PL-12 or Jo-1, the OR showed a positive association (OR (PL-12): 1.12, 95% CI 0.23–5.36; OR (Jo-1): 1.45, 95% CI 0.49–4.34) but in a lower magnitude compared to PL-7. There were no cases of UIP with the expression of EJ, OJ or ZO. In general, the expression of anti-synthetase antibodies was associated with UIP (OR: 1.38, 95% CI 0.72–2.66) although not reaching statistical significance. There was a low heterogeneity of 0% (Fig. 2A).
Forest plots comparing the association with the development of ILD patterns (NSIP, UIP, OP, NSIP+OP, non-specific pattern), based on the specific anti-synthetase antibodies expressed (Jo-1, PL-7, PL-12, EJ, OJ, Zo). Outcome: Development of ILD specific pattern. Abbreviations: NSIP: non-specific interstitial pneumonia; UIP: usual interstitial pneumonia; OP: organizing pneumonia; NSIP+OP: non-specific interstitial pneumonia+organizing pneumonia.
Regarding the NSIP pattern, a strong and statistically significant association was observed with the expression of PL-7 (OR: 2.32, 95% CI 1.12–5.04). The presence of Jo-1 and PL-12 did not show a clear negative or positive association (OR (Jo-1): 0.96, 95% CI 0.52–1.19; OR (PL-12): 1.08, 95% CI 0.44–2.66). The expression of EJ and OJ antibodies seems to have a negative association with the presence of NSIP, but did not reach statistical significance (OR (EJ) 0.45, 95% CI 0.18–1.11; OR (OJ) 0.48, 95% CI 0.13–1.8). High heterogeneity between the antibodies was observed (I2=47%) (Fig. 2B).
For OP, the expression of EJ was strongly associated with the presence of this pattern (OR: 4.28, 95% CI 1.88–9.75), while PL-7 showed a tendency towards a negative association (OR: 0.32, 95% CI 0.13–0.83). The expression of Jo-1 did not show a clear positive or negative association with the presence of this pattern (OR: 0.87, 95% CI 0.46–1.65), although it was the most common antibody reported in patients (21.2% of weight). The expression of OJ and Zo tends towards positive association with OP, but it was not statistically significant (OR (OJ) 1.68, 95% CI 0.54–5.25; OR (Zo) 1.9, 95% CI 0.12–30.91). PL-12, similar to the behaviour of PL-7, tends towards a negative association, although not statistically significant (OR: 0.48, 95% CI 0.17–1.37). It is important to highlight the significant heterogeneity of this analysis, reaching 76% (Fig. 2C).
In some case reports, the authors describe the radiologic findings (CT/high-resolution CT) but did not report a specific ILD pattern. For this reason, it was decided to group these patients in a single category named “non-specific pattern”. In this case, no significant associations were observed between antibodies and these radiologic findings. However, it is notable that the expression of Jo-1 and PL-12 tends to have a positive association (OR (Jo-1): 1.5, 95% CI 0.65–3.46; OR (PL-12): 2.35, 95% CI 0.83–6.66) with ILD. On the contrary, PL-7 and EJ tend to present a negative association (OR (EJ): 0.59, 95% CI 0.17–2.12; OR (PL-7) 0.3, 95% CI 0.07–1.32). OJ did not show a specific tendency of association. No cases were reported with the expression of Zo. A low heterogeneity of 24% was observed (Fig. 2D).
The study of Zhan et al.54 reported nine patients in which a single pattern was not found, but rather an overlap between NSIP and OP. Although there was not a statistically significant association observed, the expression of OJ and PL-7 tend to be positively associated with this pattern (OR (OJ): 4.05, 95% CI 0.75–21.88; OR (PL-7) 2.11, 95% CI 0.5–8.89). On the other hand, the expression of Jo-1, and EJ tend to have a negative association (OR (Jo-1): 0.39, 95% CI 0.08–1.92; OR (EJ) 0.59, 95% CI 0.07–4.94). No patients with expression of Zo were reported. Low heterogeneity was noted, although it could be explained by the fact that all patients were derived from the same study (I2=13%) (Fig. 2E).
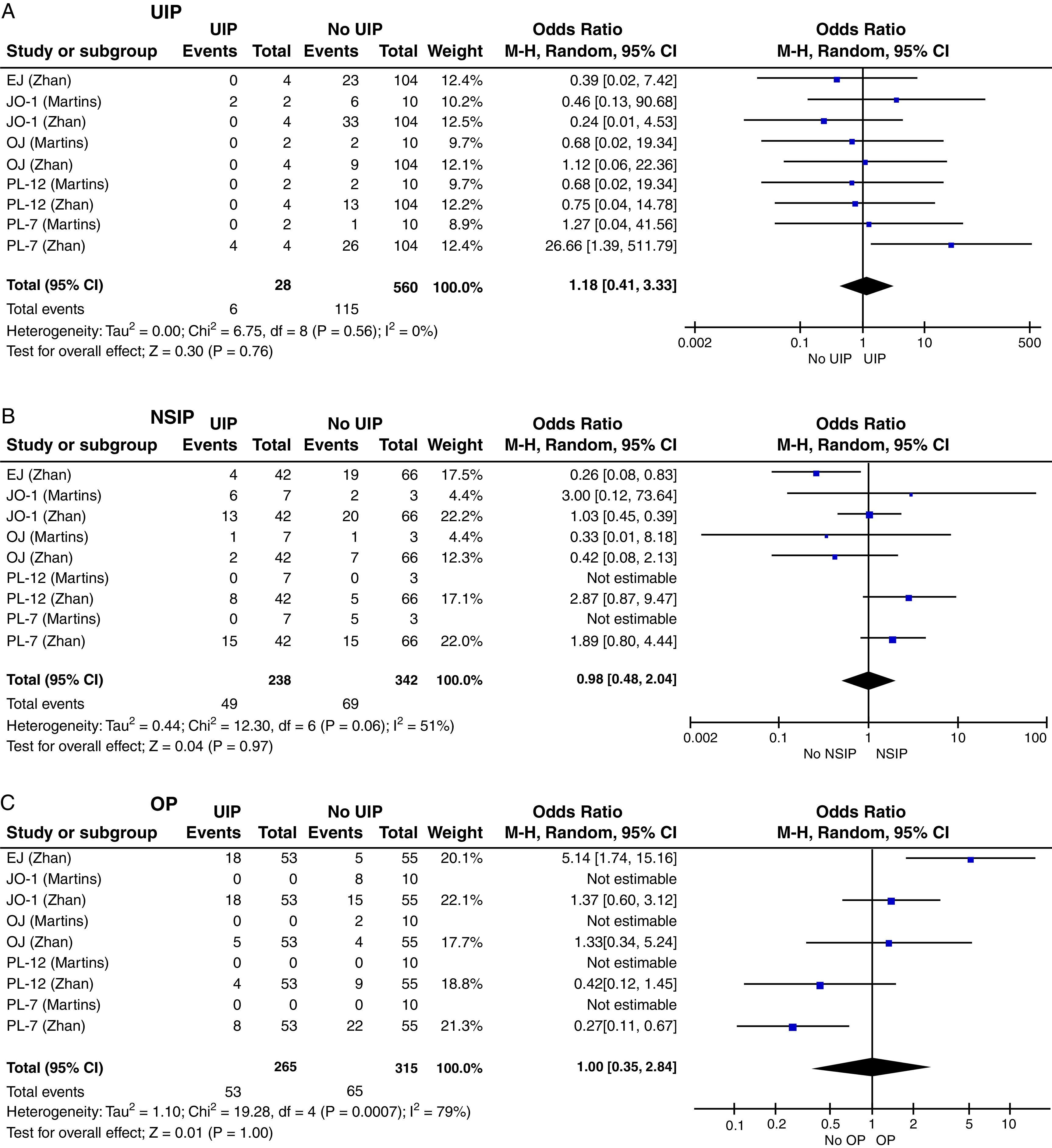
Subgroup analysisTwo retrospective cohorts were identified with a total of 125 patients (Martins et al. and Zhan et al.53,54). Based on their results, a subgroup analysis was performed aiming to establish if the behaviour from the effect size measurements from the quantitative analyses correlates with the data in both cohorts. For this, the OR was calculated between the expression of each antibody, and the presence of the different ILD patterns (UIP, NSIP, OP) for each study. Based on these results, Forest plots were developed to the respective comparisons.
Subgroup analysis of the study of Zhan et al. showed that the presence of PL-7 was significantly associated with the UIP pattern (OR: 26.66, 95% CI 1.39–511.79). It was not possible to compare the size effect with the study of Martins et al.,53 because they did not report cases of patients with UIP and PL-7. The behaviour of PL-7 in Zhan et al.54 reflects the overall results, although this cohort was the one that represents the most weight in the original plot. The study of Martins et al.53 presented two cases with expression of Jo-1, representing a positive association with UIP, although not statistically significant (OR: 3.46, 95% CI 0.13–90.68), which correlates with the observation in the general analysis. On the contrary, Zhan et al., did not report any Jo-1 positive patients with this pattern. No heterogeneity was observed in this case (Fig. 3A).
Forest plots with subgroup analysis comparing the association with the development of ILD patterns (NSIP, UIP, OP, NSIP+OP, non-specific pattern), with the specific anti-synthetase antibodies expressed (Jo-1, PL-7, PL-12, EJ, OJ, Zo), based on the observational studies of Martins et al., and Zhan et al. Outcome: Development of ILD specific pattern. Abbreviations: NSIP: non-specific interstitial pneumonia; UIP: usual interstitial pneumonia; OP: organizing pneumonia; NSIP+OP: non-specific interstitial pneumonia+organizing pneumonia.
Regarding the NSIP pattern, there was a tendency towards negative association with EJ expression (OR 0.26, 95% CI 0.08–0.83) in the study of Zhan et al.54 This finding correlates with the overall quantitative analysis. The study of Martins et al.53 did not report patients who were EJ positive, so it was not possible to compare with the cohort of Zhan et al.54 For the expression of PL-12 and PL-7, a tendency towards a positive association was observed, based on the data from Zhan et al.54 (OR (PL-12): 2.87, 95% CI 0.87–9.47; OR (PL-7): 1.89, 95% CI 0.8–4.44). However, in the study of Martins et al.53 the OR was not calculated due to the absence of patients with NSIP and these antibodies. The tendency of PL-7 with the development of NSIP correlates with the observed behaviour in the general analysis, although in the latter the association reached statistical significance (OR: 2.32, 95% CI 1.12–5.04). For PL-12, the same tendency towards a positive association is observed, and in both cases it was not significant (OR: 1.08, 95% CI 0.44–2.66) (Fig. 3B).
Both studies showed a tendency towards a positive association between NSIP with positive Jo-1 expression, but none were statistically significant (OR (Martins): 3, 95% CI 0.12–73.64; OR (Zhan): 1.03, 95% CI 0.45–2.39). In contrast to the previous cases, this behaviour does not correlate with the one observed in the overall analysis, where Jo-1 had a tendency towards a negative association, although not statistically significant (OR: 0.96, 95% CI 0.52–1.79). Finally, the expression of OJ had a negative association in both retrospective studies, but was not statistically significant (OR (Martins): 0.33, 95% CI 0.01–8.18; OR (Zhan): 0.42, 95% CI 0.08–2.13). This behaviour correlates with the observation in the overall analysis, although it could be explained by the fact that all cases were derived from both studies. Heterogeneity was of 51% (Fig. 3B).53,54
The OP pattern had a clear positive association with EJ expression, with an OR of 5.14 (95% CI 1.74–15.16) calculated for Zhan et al. This correlates with the behaviour described previously in the quantitative analysis (OR: 4.28, 95% CI 1.88–9.75). Regarding PL-7, there is a negative association, with an OR of 0.27 (95% 0.11–0.67) found in the study of Zhan et al., which corroborates the results described in the quantitative analysis (OR: 0.32, 95% CI 0.13–0.83). The presence of Jo-1 and OJ in Zhan et al., tends towards a positive association with the development of OP, but it was not statistically significant (OR (Jo-1): 1.37, 95% CI 0.6–3.12; OR (OJ): 1.33, 95% CI 0.34–5.24). In the overall quantitative analysis, OJ had the same behaviour (OR: 1.68, 95% CI 0.54–5.25), while Jo-1 appeared to be a possibly protective factor (OR: 0.87, 95% CI 0.46–1.65). Finally, the presence of PL-12 in the study of Zhan et al., had a negative association, although not significant with OP (OR: 0.42, 95% CI 0.12–1.45) which adequately correlates with the behaviour observed in the overall quantitative analysis (OR: 0.48, 95% CI 0.17–1.37). It is important to mention that in the study of Martins et al., no patients with OP pattern were reported, which made it impossible to calculate an OR to compare both studies, generating a high heterogeneity (79%) (Fig. 3C).53,54
DiscussionThe anti-synthetase syndrome, as a disease of low global prevalence, nevertheless has grave health consequences because of the high morbidity and mortality secondary to interstitial lung involvement occurring in these patients. The purpose of this systematic review was to identify the association between the presence of anti-synthetase antibodies and the presence of ILD. Improved knowledge of these associations is necessary in order to implement a more rigorous and cost-effective screening approach that allows for early identification of patients at higher risk of lung involvement, thus enabling opportune interventions to prevent the progression to end-stage disease.
In the current study, the majority of available studies correspond to case reports, where the most frequently identified antibody was anti-Jo-1, followed by PL-7, EJ, and PL-12, respectively. The most commonly reported patterns of interstitial lung involvement were NSIP and OP, although there was a considerable number of cases where only radiographic findings were described without categorizing them into a specific pattern.
When comparing the data obtained in the quantitative analysis, a high heterogeneity is evident, which may be caused by the nature of the different antibodies, which, having different substrates, affect different amino acids. Therefore, it is considered that it is not a weight factor to consider when analyzing the findings. However, in order to establish whether the effect size behaviours seen with the overall quantitative analysis correlate with data reported by retrospective observational studies, subgroup analysis was performed.
Attention is drawn to the fact that the expression of Jo-1 did not show significant associations with the presence of a specific pattern of ILD, both in the general quantitative analysis and in the subgroup analysis, despite being the most expressed antibody and having the highest number of patients in the review. This behaviour may indicate that its expression is related to the development of all patterns, without a specific predilection.
In most cases where there was a correlation between what was observed in the general quantitative analysis and the subgroup analysis. This finding was mainly due to the data from the retrospective study by Zhan et al., which provided the largest number of patients (108 cases) and adequate comparisons studies to the Zhan et al. study were lacking. Unfortunately, the study by Martins et al., although it provides valuable information, only reports 17 patients, of whom only 10 had ILD, and among them, only Jo-1 and OJ expression was identified, which affects the validity of the subgroup analysis conducted, as it does not allow for proper comparison with all the antibody profiles reported by Zhan et al.
When evaluating the strengths of this systematic review, although there is still limited evidence from studies on anti-synthetase syndrome, it was possible to gather a large number of patients (176 patients in total) with properly identified radiographic characteristics and patterns associated with ILD, despite being a disease of low prevalence. This number of patients improves the statistical significance of the results, making the estimates and findings more reliable. Moreover, the diverse demographic characteristics of the patients allow for a large and representative sample, reducing the possibility of results being biased by specific subgroup characteristics. Additionally, to the authors’ knowledge, this is the first systematic review attempting to establish the association between specific antibodies for anti-synthetase syndrome and their relationship with the development of different patterns of interstitial lung disease.
However, concerning the overall quality of the studies found during this review, an important weakness can be identified, which is the strength of the evidence from the review's results, as the majority of patients were obtained from case reports. These reports, being based on observations of individual cases, are not designed to establish causal relationships, limiting the analysis and search for associations between specific anti-synthetase antibodies and the occurrence of radiographic patterns. Likewise, the limited number of observational studies used and the high heterogeneity due to the nature of the antibodies did not allow for the development of a high-quality meta-analysis.
In pursuit of the research question regarding antibody and ILD patterns, we identified significant information gaps in available data. The majority of studies identified consisted of case reports, and only two cohort studies fulfilled inclusion criteria for our analyses, limiting the analysis of the association between the antibodies and the radiological pattern. However, a sufficient sample of patients was obtained to analyze the existing data in the literature up to this point. The study of this disease and the associated antibodies is relatively recent and no large-scale data sets are available. In fact, in most case reports the diagnosis was reached incidentally after ruling out infectious processes, especially in critically ill patients. Increasing recognition and study of this condition by clinicians and conduct of more clinical studies will help fill the existing gaps in the literature, especially regarding the behaviour of this disease at the pulmonary level. This will allow for the development of improved diagnostic and follow-up protocols that aid in the appropriate management of this disease entity, thereby reducing its morbidity and mortality and improving the quality of life for patients.
There are still many questions to be addressed in the field of autoimmune related ILD. This review contributes to pursuit of new lines of research in this arena that will better define proper management and timely treatment of anti-synthetase syndrome.
ConclusionAnti-synthetase syndrome has a high morbidity and mortality secondary to the interstitial lung involvement in affected patients. In this systematic review, we aimed to identify if there is an association between the expression of specific anti-synthetase antibodies and the presence, and putative development, of specific patterns of ILD. Despite the limitations due to the quality of the studies, it was observed that the expression of PL-7 tends to be positively associated with the presence of UIP and NSIP, while it shows a negative association with the presence of organizing pneumonia OP. EJ is strongly related to the presence of OP, while it tends to have a negative association with the presence of NSIP. Jo-1, despite being the most frequently expressed antibody, did not show a significant association with specific patterns. Although this provides a good general approximation of the behaviour of different antibodies and the presence and, putatively, development of interstitial lung disease patterns, studies of higher methodological quality are still required to generate recommendations that have an impact on clinical practice.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.