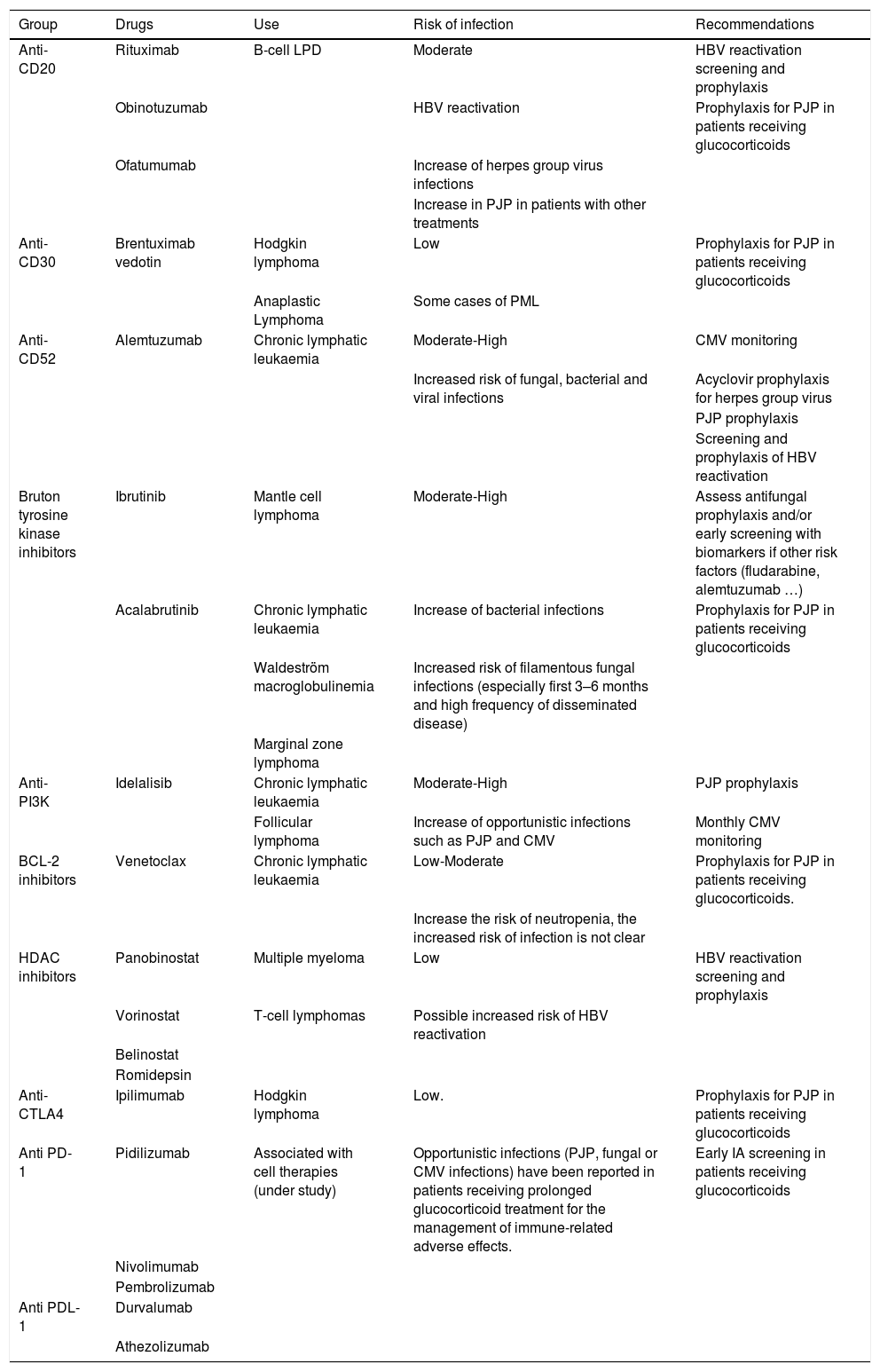
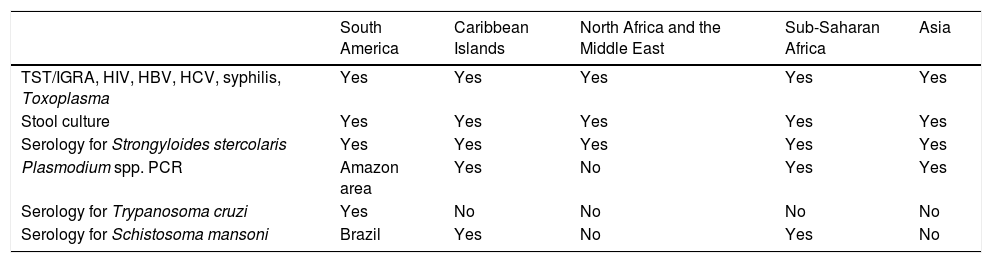
Over the last decade, there have been important developments in the treatment of lymphoproliferative disorders. Apart from conventional chemotherapy, a wide array of therapies have been developed, with different indications. The aim of this review is to evaluate the risk of infection associated with these therapies, as well as establishing prevention recommendations. In all cases, the patient’s underlying disease as well as concomitant or previous therapies have an impact in the risk of infection. Anti-CD20 antibodies (rituximab, ofatumumab and obinutuzumab) have been associated to a higher risk of bacterial and viral infection, as well as reactivation of latent infections and opportunistic infections. Alemtuzumab is associated to severe, protracted immunosuppression. Ibrutinib and acalabrutinib have been linked to bacterial infections (especially respiratory infections), invasive fungal infections and opportunistic infections. Idelalisib carries a higher risk of Pneumocystis jirovecii and infection and cytomegalovirus reactivation. Venetoclax is associated with respiratory infections and neutropenia. Immune checkpoint inhibitors are not directly associated with a higher risk of infection; nevertheless, the use of corticosteroids and immunosuppressants to control immune-related adverse events results in an increase of the risk of infection. Brentuximab, lenalidomide and HDAC inhibitors do not seem to be associated to a higher risk of infections. Although data are scarce, a higher number of infections have been observed with cellular therapies, mostly in patients with more than 3 previous antineoplastic treatments or those receiving tocilizumab or corticosteroids for managing the cytokine release syndrome.
In all patients, we recommend appropriate vaccination, screening for latent infections, and individualized prophylaxis recommendations.
En la última década se han experimentado grandes cambios en los tratamientos de los síndromes linfoproliferativos. A la quimioterapia convencional se suman ahora un amplio abanico de terapias dirigidas con diferentes indicaciones. El objetivo de esta revisión es evaluar el riesgo de infección asociado a estas terapias, así como tratar de establecer unas recomendaciones de prevención. En todos los casos, la enfermedad de base del paciente, así como los tratamientos concomitantes o los recibidos previamente impactan en el riesgo de infección. Los anticuerpos anti CD20 (rituximab, ofatumumab y obinutuzumab) se asocian a un mayor riesgo de infección bacteriana, vírica y de reactivación de infecciones latentes, así como a infecciones oportunistas. Alemtuzumab se asocia a inmunosupresión grave y mantenida. Ibrutinib y acalabrutinib se asocian a infecciones bacterianas, especialmente respiratorias, infección fúngica invasora e infecciones oportunistas. Idelalisib se asocia a un aumento de la incidencia de neumonía por Pneumocystis jirovecii y reactivación de citomegalovirus (CMV). Venetoclax se asocia a infecciones respiratorias y neutropenia. Los inhibidores de checkpoint inmune parecen no incrementar, por sí mismos, el riesgo de infección; sin embargo, el uso de glucocorticoides e inmunosupresores para controlar efectos adversos inmunorelacionados sí conlleva un aumento del número de infecciones, incluyendo infecciones oportunistas. Brentuximab, lenalidomida y los inhibidores de HDAC no parecen asociarse a un mayor riesgo de infección. Aunque existe poca experiencia en el uso de terapias celulares, se ha observado un mayor número de infecciones en pacientes que han recibido más de 3 tratamientos antineoplásicos previamente, o en aquellos que han requerido tocilizumab o glucocorticoides para el manejo del síndrome de liberación de citocinas.
En todos los pacientes se recomienda una actualización del calendario vacunal, despistaje de infecciones latentes y profilaxis individualizada.