Diabetic feet ulcer is four times more likely to be found in patients who suffer from diabetes mellitus than in those who don’t. Diabetic feet ulcer is one of chronic complications of diabetes mellitus which causes defects even deaths. Diabetes mellitus in one of the ten most frequent diseases in Indonesia. According to Riskesdas (Riset Kesehatan Dasar – Basic Health Research), the increment number of patients with diabetes mellitus from 2007 up to 2013 is 330,512.1 The research is aimed to find out the effect of oral hydrotherapy on risk reduction of diabetic feet ulcer in patients with type-2 diabetes mellitus. The research was done by applying quasi-experimental design (pre-test and post-test design with control group). By total population sampling, there were 68 respondents who participated. About 34 of the respondents were in experimental group at Dr. Soediran Mangun Sumarso of Wonogiri, and 34 respondents were patients who had check-ups at RS PKU Muhammadiyah of Surakarta. The research result shows that oral hydrotherapy can minimize risk reduction of diabetic feet ulcer in patients with type-2 diabetes mellitus significantly with p-value of 000.0 (α=0.005).
Diabetic feet ulcer is an infection, ulceration, or destruction of inner connective tissue related to neuropathy and peripheral vascular disease in lower limbs. According to May,1 patients who suffer from diabetes mellitus are four times more likely to have peripheral arterial disease compared to those who do not. PAD is a common macrovascular complication in T2DM patients, which not only may contribute for initiation and aggravation of diabetic foot ulcer but also is an efficient predictor of cardiovascular mortality and morbidity.2
WHO estimated that three hundred sixty six million people have DM in 2011; half of these (183 million people) are undiagnosed. The number of people with DM worldwide is increasing and by 2030 this will have risen to 552 million.3 According to Basic Health Research in 2007, deaths caused by diabetes mellitus in the 45–54-year age group in cities ranked second at the percentage of 14.7%, while in villages, it ranked sixth at the percentage of 5.8%.4
Diabetic feet ulcer is one of the most serious complications, and for people with diabetes mellitus, it can lead to defects. People with diabetes account for more than 40% of hospitalizations for major amputations and 73% of emergency room admissions for minor amputations.5 According to Navarro-Peternella et al.6 women have higher risk six times to have diabetic feet ulcer than man.
Furthermore, Navarro-Peternella et al.6 stated that the older the age of the people with diabetes mellitus, the higher the risk to have diabetic feet ulcer since old people have less body movement, worse eyesight, and other health problems. According to Martínez-Castelao et al.,7 10–25% of diabetes mellitus cases lead to diabetic feet ulcer.8 This indicates that 58% of 100 patients suffering from diabetes mellitus with diabetic feet ulcer have suffered from diabetes mellitus for more than 10 years.
Management of diabetes can be conducted pharmacologically by glucose and/or insulin control treatment, or non-pharmacologically such as healthy lifestyle modification, activity and energy management, and complementary therapy. One example of complementary therapies which is usually used is oral hydrotherapy. It is done by drinking 1.5l of warm water every morning soon after getting up, or by drinking 8 glasses of water at the least every day.
Hydrotherapy is the cheapest health therapy and it has a lot of benefits. According to Daniel and Popkin,9 drinking water can lessen obesity and fulfill the need of fiber. Water consumption helps the process of detoxification including getting rid of sugar excess in body.10 Explains that drinking water can release chemical substances such as glucose and other substances through kidneys and through the body organ cleaning process.
Osmotic increase and glucose dilution in plasma can increase peripheral circulation. Guaranteed adequate circulation leads to the decrease of peripheral arterial disease (PAD) so that feet ulcer can be prevented as early as possible. PAD check can be done by a measurement using Ankle Brachial Index (ABI). Study was conducted by Xu et al.11 show that the ABI value=0.9 can be a simple diagnosing instrument, can be used to identify peripheral arterial disease with severe stenosis, and can be a substitute instrument to do another non-invasive check-up clinically.
MethodsThe research applies quasi-experimental design by pre and post-test with control group. The 68 samples were taken by using totally sampling method. 34 respondents at RSUD dr. Soediran Mangoen Sumarso of Wonogiri got pharmacological treatment therapy and oral hydrotherapy. The other 34 respondents at RS PKU Muhammadiyah of Surakarta only got pharmacological therapy.
ResultsUnivariate analysisBy univariate analysis, respondent characteristics based on age, sex and Ankle Brachial Index can be identified.
Homogeneity testAgeThe average age of the respondents in the control group is 56.32 with the standard deviation of 7.36. The youngest age is 40 years old and the oldest is 70 years old. In the intervention group, the average age of the respondents is 52.41 with the standard deviation of 9.88. The youngest age is 31 years old and the oldest age is 70 years old. Based on homogeneity test, it was found that there was parity of the ages of the respondents with p-value of 0.069, α=0.05, in both the control group and the intervention group.
SexAmong 68 respondents involved in the research, 22 respondents of them are male and the other 46 respondents are female. There are 9 male respondents (26.5%) in the control group and 13 male respondents (38.2%) in the intervention group. There are 25 female respondents (73.5%) in the control group and 21 female respondents (61.80%) in the intervention group. Sex parity with p=0.26 and α=0.05.
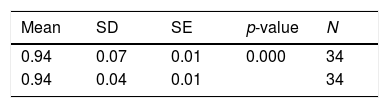
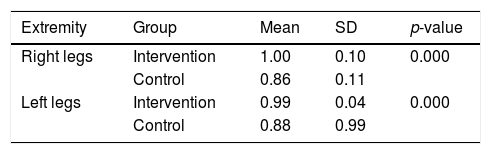
Ankle Brachial IndexThe measurement using Ankle Brachial Index, in the control group, it was found that the extremity average of the right legs of the respondents before oral hydrotherapy was 0.86 with the standard deviation of 0.11, and the extremity average of the left legs of the respondents before oral hydrotherapy was 0.88 with the standard deviation of 0.10. After oral hydrotherapy treatment, the extremity average of the right legs was 1.00 with the standard deviation of 0.10, and the extremity average of the left legs was 0.99 with the standard deviation of 0.04.
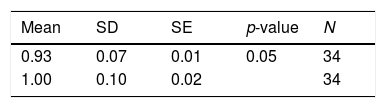
In the intervention group, the extremity average of the right legs of the respondents was 0.93 with the standard deviation of 0.07, and the extremity average of the left legs of the respondents was 0.94 with the standard deviation of 0.07. After the intervention, the extremity average of the right legs of the respondents in the intervention group was 0.93 with the standard deviation of 0.07, and the extremity average of the left legs was 0.94 with the standard deviation of 0.07.
Table 1 shows the result of homogeneity test with one-way ANOVA (one-way analysis of variance) technique. There is equal values of ABI of right legs with p-value of 0.74 and equal values of ABI of left legs with p-value of 0.61 and α=0.05.
Normality testOn the normality test, it was found that the skewness value of ABI variable of right legs before hydrotherapy was 0.037, with standard error value of 0.403, so that the value of skewness normality was 0.092 (<2). This means the data distribution was normal. On the test of left legs before hydrotherapy, it was found that the skewness value was 0.827, with standard error value of 0.403, so that the value of skewness normality was 2.00 (<2). This means the data distribution was also normal. On the normality test of ABI variable of right legs after hydrotherapy, it was found that the skewness value was 0.614, with standard error value of 0.403, so that the value of skewness normality was 0.092 (<2). This shows the data distribution was normal. On the test of left legs after hydrotherapy, it was found that the skewness value was 0.561, with standard error value of 0.403, so that the value of skewness normality was 1.39 (<2). This also shows normal data distribution.
Based on normality test previously shown, bivariate analysis was done by using paired t test. Table 2 shows there is difference of ABI values of right legs before and after oral hydrotherapy treatment with p-value of 0.005. Table 3 shows there is difference of ABI values of left legs of the respondents before and after oral hydrotherapy treatment with p-value of 0.000. Table 4 shows the increase of mean values of ABI after the intervention both on right legs (0.14) and left legs (0.11). p-value of right legs is 0.000 and p-value of left legs is 0.000. Thus, it can be concluded that oral hydrotherapy helps in minimizing risk of diabetic feet ulcer.
According to the research result, it was found that oral hydrotherapy helped in minimizing risk of diabetic feet ulcer in patients with type 2 diabetes mellitus with p-value of 0.000 (α=0.005). Oral hydrotherapy helps patients with diabetic feet ulcer in the process of body detoxification, including releasing excess of sugar. The research goes along with MacAulay and Zeuthen12 who states that body fluid can lead to osmotic increase that can dilute glucose in plasma. When glucose in blood is in normal condition, food supply can be more easily transferred to repair organ with diabetic feet ulcer. According to Ikem et al.,13 diluting glucose is the best solution for people suffering from diabetes mellitus in lowering blood sugar level.
The research result of study conducted by Daniels and Popkin14 explains that drinking water can fulfill the need of fiber and fluid in people suffering from diabetes mellitus. The research result also shows that diabetic feet ulcer occurs more in women, which is 67.65% compared to the number of men with diabetic feet ulcer. The result goes along with the research conducted by Chivese et al.15 and Younis et al.16 which tells that diabetic feet ulcer occurs more in women.
Aging leads to higher risk of diabetic feet ulcer because body function worsens physiologically. The average age of patients with diabetic feet ulcer in the research is 56.32 in the control group and 52.41 in the intervention group. The research result goes along with the research result of Younis et al., 2018 in which there is significant relation between age and the increasing number of peripheral arterial disease cases in patients with type 2 diabetes mellitus.17
ConclusionOral hydrotherapy can minimize the risk of diabetic feet ulcer in patients with type 2 diabetes mellitus. Oral hydrotherapy is done by drinking 1.5l of boiled water within 2h every morning (after getting up before rinsing mouth and brushing teeth) for 30 days and the water must be daily consumed, odorless, colorless, and tasteless.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Conference on Healthcare and Allied Sciences (2019). Full-text and the content of it is under responsibility of authors of the article.