The 4th Udayana International Nursing Conference (4th INC)
Más datosThe COVID-19 pandemic has impacted breastfeeding self-efficacy directly or indirectly. This is likely due to the adverse effect of movement and community activity restrictions to prevent virus transmission. This study aims to measure how breastfeeding self-efficacy has been affected by the COVID-19 pandemic.
MethodThis study uses a cross-sectional design with participants consisting of mothers giving birth from June to July 2021 in Bekasi, Indonesia. The recruitment used a consecutive sampling method. The data were collected using the breastfeeding self-efficacy scale-short form, the postpartum bonding questionnaire, the Zung self-rating anxiety scale, and the multidimensional scale of perceived social support. The COVID-19-related factors, i.e., anxiety, bonding and social support on breastfeeding self-efficacy, were measured using the Path Analysis.
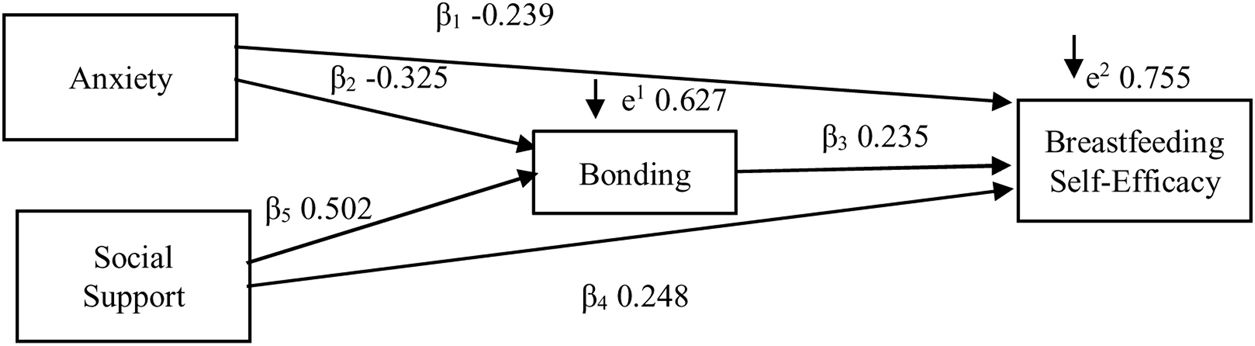
ResultsThe results showed that anxiety, bonding, and social support affected breastfeeding self-efficacy among the 118 respondents. While anxiety had a negative effect on breastfeeding self-efficacy, bonding and social support had a positive effect. The effect of anxiety was more direct (β −0.239; p 0.00) than indirect (β −0.076; p 0.04). Social support also had a more direct (β 0.248; p 0.00) than indirect effect (β 0.118; p 0.046). Likewise, bonding had a significant impact on breastfeeding self-efficacy (β 0.235; p 0.039). However, the effect of anxiety and social support indirectly on breastfeeding self-efficacy via bonding was less significant than their direct impacts.
ConclusionThe factors related to breastfeeding self-efficacy affected by the COVID-19 pandemic are anxiety, bonding, and social support. Interventions during a crisis such as the pandemic could aim to reduce anxiety and improve social support. Health education and counselling are essential to enhance competence and self-efficacy in breastfeeding their babies and build more positive interactions with their children.
Breastfeeding self-efficacy (BSE) is the most influential factor in predicting and improving exclusive breastfeeding in the third month after giving birth.1,2 BSE is a mother's belief in her ability to breastfeed, which is highly predictive of breastfeeding behaviours.2 BSE affects the success of achieving exclusive breastfeeding for up to six months. Mothers with a high BSE have a higher potential for exclusive breastfeeding than those with a low BSE. Early breastfeeding cessation may result in mothers losing confidence in breastfeeding, as well as chest pain and breast milk insufficiency.1 Before discharging mothers from the hospital, health professionals should monitor breastfeeding behaviours and provide mothers with sufficient information and help to improve their self-efficacy.1,3
During the COVID-19 pandemic, movement restrictions to curb the transmission in Indonesia reduced public access and visits to maternal and child health services at the primary health centre (PHC) or mother–child health centre, including access to services related to lactation.4,5 This restriction indirectly impacted the health status of mothers and children because the services were temporarily stopped. In addition, the movement restrictions could be one of the stressors for postpartum mothers during breastfeeding.
The reduced access to PHC services and the declining number of maternal visits could indirectly pose a risk of escalating the number of infants who were not exclusively breastfed. Breastfeeding difficulties coupled with the absence of healthcare providers’ support may demotivate mothers to continue breastfeeding exclusively for up to six months.6 Encouragement to continue breastfeeding from experts and health providers is vital to optimising exclusive breastfeeding.1
The COVID-19 pandemic has directly and indirectly affected several factors related to BSE. The government's imposition of COVID-19 health protocols and restrictions on community activities to prevent COVID-19 cases separated mothers from their families and health services. This separation may lead to an increase in anxiety and a decrease in perceived social support. In case of infection, mother-infant bonding could also suffer. In other words, the COVID-19 pandemic may have significantly affected BSE. However, there have not been studies focusing on this relationship, so this study aims to fill the gap by measuring the direct and indirect factors affecting BSE, namely anxiety, social support, and mother-infant bonding during the COVID-19 pandemic.
Given that bonding was related to anxiety, social support, and BSE, this study examines bonding as a bridging factor to mediate the direct and indirect effects of the independent variables on BSE. In other words, bonding is an intervening variable between independent variables (anxiety, social support) and dependent variable (BSE).
MethodThis study applies a cross-sectional design to 118 breastfeeding mothers in Bekasi, West Java, Indonesia, from June to July 2021. The respondents were selected using the consecutive sampling method. The inclusion criteria were mothers who gave birth during the COVID-19 pandemic, had babies aged less than six months, and lived in Bekasi. The mothers who were not present at the time of the study were excluded from the study. Research data collection was conducted face-to-face by applying health protocols.
This study utilised the breastfeeding self-efficacy scale-short form, the postpartum bonding questionnaire, the Zung self-rating anxiety scale, and the multidimensional scale of perceived social support. The validity and reliability were tested, and the results revealed that all the instruments were valid and reliable.
The research procedure was explained to prospective respondents by upholding the principles of confidentiality, integrity, and non-maleficence. This research protocol fulfilled the ethical clearance by the Research Ethics Commission of the Faculty of Medicine, Universitas Pembangunan Nasional Veteran Jakarta, with an Ethical Approval Letter Number: 171/IV/2021/KEPK. Data collection was carried out after obtaining approval from respondents and witnesses. Path analysis was performed to measure factors affecting BSE during the COVID-19 pandemic, specifically anxiety, bonding, and social support for BSE.
ResultsThis study involved 118 respondents. Table 1 describes the characteristics of respondents in this study. The data met the requirements of the classical assumption test before the path analysis was conducted. The result of the Kolmogorov-Smirnov test showed that all data were normal (p>0.05) with the following details: anxiety (p=0.070), social support (p=0.200), and bonding (p=0.200). The heteroscedasticity test result showed no heteroscedasticity problem in the data (p>0.05; anxiety p=0.363, social support p=0.052, and bonding p=0.594). The multicollinearity test result showed no symptoms of intercorrelation in the data (tolerance value>0.10; the tolerance values for the variables of anxiety, social support, and bonding were 0.379, 0.332, and 0.394, respectively).
Characteristics of respondents.
| No. | Respondent characteristics | Mean | Min | Max | SD | Total (n) | % |
|---|---|---|---|---|---|---|---|
| 1. | Mother's age (year) | 28.72 | 17 | 41 | 4.367 | ||
| Baby's age (month) | 3.68 | 1 | 5 | 1.345 | |||
| 2 | Level of education | ||||||
| - Basic (elementary school) | 11 | 9.3 | |||||
| - Middle (junior to senior high school) | 93 | 78.8 | |||||
| - Higher education (college) | 14 | 11.9 | |||||
| 3 | Working status | ||||||
| - Not working | 98 | 83.1 | |||||
| - Working | 20 | 16.9 | |||||
| 4 | Parity | ||||||
| - Primipara | 30 | 25.4 | |||||
| - Multipara | 88 | 74.6 | |||||
| 5 | Type of delivery | ||||||
| - Normal/spontaneous | 88 | 74.6 | |||||
| - Section Caesarea | 30 | 25.4 | |||||
| 6 | Anxietya | 63.07 | 37 | 80 | 14.40 | ||
| 7 | Social supportb | 51.69 | 30 | 68 | 8.79 | ||
| 8 | Bondingc | 36.74 | 20 | 52 | 11.11 | ||
| 9 | Breastfeeding self-efficacyd | 54.77 | 41 | 70 | 7.69 | ||
Table 1 shows that the average age of mothers was in the range of the fertile age category. They had a medium level of education and were not employed. Additionally, more than half of breastfeeding mothers involved in this study were multiparas who gave birth spontaneously during the pandemic. The pandemic had induced anxiety in the respondents. Nevertheless, respondents had good bonding, social support, and BSE on average.
The results of Model I (Table 2) show the effect of the independent variable on the dependent variable with a p-value=0.000, meaning that anxiety, social support, and bonding directly affect breastfeeding self-efficacy. The value of R2 of 0.430 shows the contribution of the direct effect of 43%, whereas the remaining 57% is the influence of other contributing variables not included in the study. The results of Model II show a significant effect of the independent variable on the dependent variable with the value of p=0.044. This result indicates that anxiety and social support affect BSE via bonding. The value of R2 is 0.606, indicating that the contribution effect of anxiety and social support via bonding on BSE is 60.6%. Meanwhile, the remaining 39.4% is the contribution of other variables not included in the study. The test results of Models I and II are combined in the following path analysis structure model (Picture 1).
Path analysis of factors affected breastfeeding self-efficacy.
| Dependent variables | Independent variables | ba | SE | p-Value | βb | R2 | Coef p |
|---|---|---|---|---|---|---|---|
| Model I | |||||||
| Bonding | ← Anxiety | −0.251 | 0.070 | 0.000 | −0.325 | 0.430 | 0.044 |
| Bonding | ← Social support | 0.635 | 0.114 | 0.000 | 0.502 | ||
| Model II | |||||||
| Breastfeeding self-efficacy | ← Anxiety | −0.128 | 0.061 | 0.040 | −0.239 | 0.606 | 0.000 |
| Breastfeeding self-efficacy | ← Social support | 0.217 | 0.107 | 0.046 | 0.248 | ||
| Breastfeeding self-efficacy | ← Bonding | 0.163 | 0.078 | 0.039 | 0.235 | ||
As seen in Table 3, the results show that anxiety, bonding, and social support significantly affect BSE. Anxiety has a negative effect, while both bonding and social support have a positive impact on BSE. The level of anxiety has a more direct effect (β −0.239; p 0.00) than the indirect effect (β −0.076; p 0.04) on BSE. Social support is also more direct (β 0.248; p 0.00) than indirect effect (β 0.118; p 0.046) on BSE. On the other hand, bonding also significantly impacts BSE (β 0.235; p 0.039). However, the effect of anxiety and social support indirectly on BSE via bonding is not more significant than their direct impact.
DiscussionAnxiety, social support, and bonding, directly affects BSE during the COVID-19 pandemic in this study. This result is consistent with previous studies conducted before the pandemic which proved that anxiety, social support, and bonding affected self-efficacy.1,7–10 It is suggested to raise self-efficacy education, provide information and awareness and also psychological intervention for mothers.1 The current study set the bonding variable as an intervening variable. As a result, the variables of anxiety and social support have a significant indirect effect on BSE through the bonding variable. Therefore, it is recommended raising interventions that modify anxiety and social support. However, further analysis shows that the direct effect magnitude is greater than the indirect effect between the independent and dependent variables.
Regarding anxiety, the magnitude of the direct effect on BSE is bigger than the indirect effect. A total of direct and indirect effect has a minus value. The minus value indicates the opposite direction, meaning the higher the anxiety, the lower the BSE. The path analysis results show that the direct effect of anxiety on BSE is greater than the indirect effect of anxiety on BSE through the bonding factor. In other words, interventions for reducing anxiety during the pandemic alone will consequentially increase BSE without interventions to the bonding. Therefore, interventions are recommended to modify the anxiety of breastfeeding mothers during the pandemic as it is proved affected BSE.
The direct effect magnitude on the social support factor is greater than the indirect effect with a total effect in a positive value. The positive value indicates the proponent direction, meaning the bigger social support of mother, the BSE will be greater. Furthermore, the results of the path analysis show that the direct effect of social support on BSE is greater than the indirect effect of social support on BSE through the bonding factor. In other words, providing interventions only to improve social support during the pandemic without interventions for the bonding will increase BSE. Therefore, interventions are recommended to raise social support for breastfeeding mothers during this pandemic because it positively affects BSE.
Interventions are recommended to reinforce BSE in breastfeeding mothers. Health education and counselling are essential to enhance mothers’ competence and self-efficacy in breastfeeding their babies and build positive interactions with their children.11 Psychological care and training programmes are also recommended to boost self-efficacy, exclusive breastfeeding, and duration of breastfeeding among mothers.1 Aside from this, improving social support and reducing anxiety during the pandemic is also necessary. For example, healthcare providers can promote individual visits to help mothers optimise results, but in doing so, they must strictly implement COVID-19 health protocols.6 What needs to be noted is that, even during the COVID-19 pandemic, the recommended interventions are still in the ‘meeting in person’ context for practical issues. Health providers can immediately recognise and support mothers struggling with anxiety or mental health challenges by contacting the mothers directly. However, the effectiveness of online versus offline contact is currently uncertain and requires further evaluation.12
The magnitude of the bonding effect is not large enough to mediate the relationship between anxiety and social support with BSE. It is in line with the result of the Sobel test, indicating that bonding is not a significant intervening variable in the indirect effect among independent and dependent variables (z value 2.796>1.994). The effect is reasonable considering that most breastfeeding mothers in this study were multiparous with babies older than three months. Their previous breastfeeding experiences can be a determinant.13,14
This current study did not control the confounding variables between the independent and dependent ones. As a result, the number of confounding variables in the direct effect path is fewer than in the indirect path. The independent variable must go through via bonding before contributing to the effect on BSE.
To summarise, the factors related to breastfeeding self-efficacy affected by the COVID-19 pandemic include anxiety, social support, and bonding, which have a significant and indirect effect. In other words, the COVID-19 pandemic may have significantly affected BSE in breastfeeding mothers. Nevertheless, bonding could not be considered an intervening factor as Sobel tests showed insignificant results and a shallow indirect effect. Therefore, we recommend that relevant interventions target anxiety and social support to improve BSE during the pandemic.
FundingLPPM Universitas Pembangunan Nasional “Veteran” Jakarta (Contract agreement No. 062/UN.61.0/HK.02/LIT.RUPS/2021).
Conflict of interestThe authors declare no conflict of interest.
All researchers would like to thank the head of primary health center of Bekasi regency, community health volunteers and Imanuel Sianipar for the support given during the study.
Peer-review under the responsibility of the scientific committee of “The 4th Udayana International Nursing Conference (4th INC)”. Full text and its content are under the responsibility of the authors of the article.